Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.57 supl.1 Cuernavaca 2015
Artículo original
Frailty among Mexican community-dwelling elderly: a story told 11 years later. The Mexican Health and Aging Study
Fragilidad en adultos mayores mexicanos: la historia 11 años después. Encuesta Nacional sobre Salud y Envejecimiento en México
Sara G Aguilar-Navarro, MD, MSc,(1) Hélène Amieva, PhD,(2) Luis Miguel Gutiérrez-Robledo, MD, PhD,(3) José Alberto Avila-Funes, MD, PhD(1,2)
(1) Departamento de Geriatría, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Mexico City, Mexico.
(2) Centre de Recherche Inserm (Inserm Research Center), Université Victor Segalen Bordeaux 2. Bordeaux, France.
(3) Instituto Nacional de Geriatría. México City, Mexico.
Abstract
Objective. To describe the characteristics and prognosis of subjects classified as frail in a large sample of Mexican community-dwelling elderly.
Materials and methods. An eleven-year longitudinal study of 5 644 old adults participating in the Mexican Health and Aging Study (MHAS). Frailty was defined by meeting at least three of the following criteria: weight loss, weakness, exhaustion, slow walking speed and low physical activity. The main outcomes were incident disability and death. Multiple covariates were used to test the prognostic value of frailty.
Results. Thirty-seven percent of participants (n= 2 102) met the frailty criteria. Frail participants were significantly older, female, less educated, with more chronic disease, lower income, and poorer self-reported health status, in comparison with their non-frail counterparts. Frailty was a predictor both for disability activities of daily living and for mortality.
Conclusion. After a follow-up of more than ten years, the phenotype of frailty was a predictor for adverse health-related outcomes, including ADL disability and death.
Key words: disability; mortality; elderly; health vulnerability; Mexico.
Resumen
Objetivo. Describir las características y el pronóstico de una muestra representativa de ancianos de la comunidad clasificados como frágiles.
Material y métodos. Estudio longitudinal de 11 años de seguimiento a 5 644 sujetos mayores de 60 años, participantes de la Encuesta Nacional sobre Salud y Envejecimiento en México (Enasem). Fragilidad se definió con, al menos, tres de los siguientes criterios: pérdida de peso, debilidad, extenuación, enlentecimiento de la marcha y baja actividad física. Los desenlaces de ésta fueron incidencia de discapacidad y muerte. Se construyeron modelos multivariados para probar el valor pronóstico de la fragilidad.
Resultados. Del total de participantes, 37% reunió los criterios de fragilidad (n= 2 102). Estos, en comparación con los clasificados como no frágiles, fueron significativamente más ancianos y mujeres; asimismo tuvieron menor nivel educativo, más enfermedades crónicas, bajos ingresos y mala autopercepción de salud. La fragilidad fue un predictor de discapacidad para las actividades básicas de la vida diaria y mortalidad.
Conclusión. El fenotipo de fragilidad fue un predictor de discapacidad y muerte después de un seguimiento de más de 10 años.
Palabras clave: discapacidad; mortalidad; anciano; vulnerabilidad en salud; México.
Aging in population has raised concerns about its adverse health-related outcomes. The concept of frailty has emerged as a condition associated with an increased risk of functional decline among elderly people, which may be differentiated from aging, disability, and co-morbidity.1,2 Frailty involves a state of vulnerability to adverse effects of a variety of environmental stressors, expressed as an increased risk of accumulating health related problems, hospitalization, need for long-term care, and also death.3
In order to identify frail individuals, several criteria have been proposed recently.1 According to the criteria used, heterogeneous results regarding prevalence have been obtained.4 However, there is a remarkably higher frequency of frailty among Latin-American populations in comparison with European or American elderly.4-6 Nevertheless, there is a general agreement that the core feature of this syndrome is an increased vulnerability due to impairments in multiple inter-related systems resulting in homeostatic reserve disturbance.7 The most popular definition of frailty is that derived from the Cardiovascular Health Study (CHS), which was proposed at the end of the 90's by Fried and colleagues1 and accepted by the American Geriatrics Society.8 This definition conceptualizes frailty as a clinical syndrome defined as the combination of weight loss, weakness, exhaustion, low walking speed and low physical activity.1 In addition, this conception of physical frailty implies a biological connection between all five components and has been demonstrated to have high predictive validity for adverse health-related outcomes in very different populations.9
Recently, our team reported the predictive validity of frailty among Mexican community-dwelling elderly.6 However, outcomes such as mortality could be influenced by other factors beyond the syndrome of frailty because of the shortness of the two-year follow-up. Thus, the longer follow-up of the Mexican Health and Aging Study (MHAS) provides now a unique opportunity to a longer-term study of the relationship between frailty and the ability to identify elder persons at risk for adverse health-related outcomes. Therefore, the main objective of this report is to describe the features and prognosis of subjects classified as frail in a large sample of Mexican community-dwelling elderly studied during 11 years. The main hypothesis is that frail individuals, in comparison with non-frail subjects, present more adverse health-related outcomes even after an adjustment for potential confounders.
Materials and methods
Study population
The participants in the present study are a subset from the Mexican Health and Aging Study (MHAS), a prospective panel study of health and aging in Mexico. The aim and design of the MHAS have been published previously.10 Briefly, the baseline survey was conducted in the summer of 2001, and followed-up in 2003 and 2012 It was derived from the fourth wave of the National Employment Survey and it is regarded as a nationally representative sample of Mexicans aged 50 and older and their spouse/partners regardless of their age. It considers subjects from both urban and rural areas. Data were obtained from direct face-to-face interviews and individual audits, and proxy interviews were conducted when poor health or temporary absence prevented a direct interview. The MHAS is only representative of community-dwelling people. In the case of Mexico, it is not an important omission because, according to the 2000 National Population Survey, less than 1% of people aged 60 years and older live in an institution. The MHAS includes data from 15 230 interviews (9 806 index cases and 5 424 spouses/partners). It contains self-reported information regarding health measures (functional status and health related behaviors [e.g. smoking and drinking history]), access to health services, depressive symptoms, pain, cognitive performance, and anthropometrical measurements. The MHAS was supported by a grant from the National Institutes of Health/National Institute of Aging. The study is a collaborative effort among researchers from the University of Pennsylvania, the University of Maryland, and the University of Wisconsin in the US and the Instituto Nacional de Estadística, Geografía e Informática (INEGI) in Mexico. Oral informed consent was obtained in accordance with the provisions of the ethical principles of the Declaration of Helsinki.11
Definition of frailty
Frailty was defined according to the construct previously validated in the CHS.1 All five components were retained, but the metrics used were slightly different and adapted by an expert panel. The composite measures were defined as follows:
• Weight loss was defined as a self-reported, unintentional weight loss of 5 kg or more in the previous two years or as a calculated body mass index (BMI), assessed through self-reported anthropometrical measurements, lower than 22 kg/ m2. This threshold has been associated with increased several adverse health-related outcomes in community-dwelling elderly.12 -13
• Exhaustion was evaluated with the following question: "During the last two years, have you frequently had severe fatigue or exhaustion?"
• Low walking speed was assessed through the following two questions: "Because of a health problem, do you experience difficulty walking one block?" and "Because of a health problem, do you have difficulty climbing flights of stairs without resting?". Participants answering affirmatively to either of these questions were considered frail regarding this component.
• Weakness was considered to be present when subjects answered the following question positively: "Because of a health problem, do you have difficulty lifting or carrying objects over 5 kg, such as a heavy bag of groceries?"
• Low physical activity was defined as a negative answer to the question: "During the last two years have you exercised or done hard physical work on average at least three times a week?"
As recommended, the subjects were considered to be frail if they had three or more frailty components among the five criteria; they were considered prefrail if they fulfilled one or two frailty criteria, and nonfrail if none.
Outcomes
Three disability domains were specifically investigated: mobility, instrumental activities of daily living (IADL) and basic activities of daily living (ADL). Mobility was assessed using a modified version of the Nagi scale,14 through which participants reported their ability to perform four tasks: pushing or pulling objects, stooping or crouching or kneeling, reaching or extending arms, and handling small objects. For IADL, participants reported their ability to perform four tasks based on the Lawton and Brody scale:15 administering their own medication, handling money, shopping and grooming. For ADL, participants were asked about their ability to perform five tasks from the Katz ADL scale:16 bathing, walking, transferring themselves from bed to chair, handling continence and feeding themselves. For each domain of disability, if participants indicated that they were unable to perform one or more activities without help, they were considered as having mobility, IADL or ADL disability. The cumulative 11-year incidence of disability was established only among those without prevalent disability in the same domain at baseline, when they declared it either at the first (two years) or at subsequent follow-up interviews (11 years).
Time of death was obtained from interviews with proxies at both follow-ups, and it was treated as cumulative 11-year mortality.
Covariates
Sociodemographic variables such as age, sex, living alone, and educational level (i.e. years of education) were obtained at baseline and used as covariates. In the same vein, self-reported health and financial situation were recorded and treated as categorical variables (good, fair, or poor). Participants were asked whether they had a physician's diagnosis of hypertension, diabetes, cancer, myocardial infarction or angina pectoris, chronic obstructive pulmonary disease, fractures after age of 50, or arthrosis. The presence of each of these diseases was summed up to in a comorbidity score (ranging from 0 to 7), where higher score indicates more chronic diseases. The presence or absence of visual and hearing impairment was also self-reported.
Depressive symptoms were evaluated using a modified and validated version of the Center for Epidemiological Studies-Depression scale.17 A score ≥5 was positive for depressive symptoms.
Cognitive impairment was evaluated using a brief and validated version of the Cross-Cultural Cognitive Examination (CCCE), which considers five items for evaluating different cognitive domains. The cut-off points for each item were set using the 10th percentile and adjusted by sex and educational level for participants younger than 60 years of age.18
Smoking status ("Have you ever smoked cigarettes?") and alcohol intake ("Do you ever drink any alcoholic beverages?") were considered dichotomous self-reported variables.
Sample
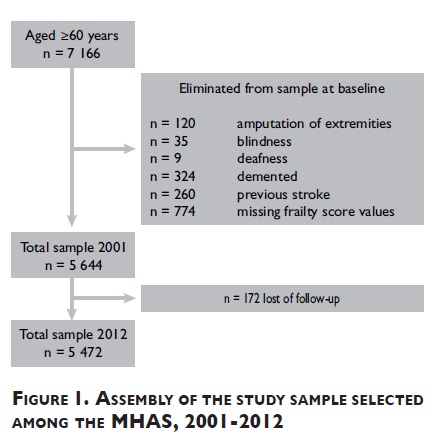
For the present study, 7166 participants aged 60 years and older were considered. However, subjects with single conditions that could yield a similar phenotype to frailty were excluded (figure 1). Therefore, data from 2 618 (46.4%) men and 3 026 (53.6%) women who completed the clinical and functional evaluation at baseline were included in the statistical analysis.
Statistical analysis
Variables are described using arithmetic mean and standard deviation (SD) or the frequency and proportion where appropriate. The following statistical procedures were used according to the characteristics of each variable: chi square test for qualitative data or analysis of variance (Anova) for continuous data. Post-hoc comparisons between frailty subgroups were conducted for continuous data where indicated (Bonferroni's correction). In order to determine the predictive validity of the frailty phenotype, separate logistic regression models were created to describe the unadjusted effect of frailty on 11-year incident mobility IADL, and ADL disability. In a second step, multivariate logistic regression analyses were used to study the effect of frailty, adjusting for multiple covariates (age, sex, education level, number of chronic diseases, smoking status, drinking status, self-reported health, cognitive impairment, and depressive symptoms) on the described outcomes. Incidence of IADL disability was also adjusted for baseline mobility disability, whereas for the analysis of incident ADL disability, baseline mobility and IADL disability were included. Probability of death without depending on the status of frailty survival was estimated by Kaplan-Meier method. Cox proportional hazard model was performed to estimate the risk of death, and later was also performed using all variables mentioned above, including the three domains baseline disability, with frailty status as the main explanatory variable. All statistical tests were performed at the 0.05 level and 95% confidence intervals (CI) were given. All statistical tests were performed using the SPSS software for Windows (SPSS Inc., Chicago, IL, version 16.0).
Results
The study sample comprised 5 644 individuals. Mean age was 68.7 years (SD 6.9) years and 53.6% were women. The most frequently reported chronic diseases were hypertension (41.4%), arthrosis (24.3%), and diabetes (16.9%). 37% of participants had depressive symptoms, and 25.9% had cognitive impairment. At baseline, 48.3, 10.1, and 3% were disabled for mobility, IADL, and ADL, respectively. Table I shows the frequency of each frailty component. Frailty was present in 37.2% of the participants, 51.3% were prefrail, and 11.5% were nonfrail. Lower physical activity was the most frequent frailty component for both sexes.
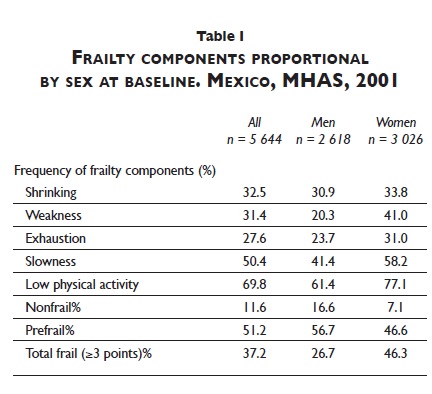
Table II shows the sociodemographic and health characteristics of the participants according to their frailty status at baseline. As expected, participants classified as frail were older, more likely to be women, to have lower education, reporting more chronic diseases, presenting poorer self-reported health and economic status (all p values < .001), this in comparison with prefrail and nonfrail persons. In addition, frail subjects were more frequently cognitively impaired, had more depressive symptoms, and had more sensory impairment. Disability for mobility, IADL, and ADL was significantly more frequent in the frail and prefrail subgroups than in the nonfrail subgroup.
Disability
After 11-years of follow-up, 51.9% nonfrail, 67.5% prefrail, and 82% frail participants developed mobility disability. Incident IADL disability was 24.2, 27.1, and 40.8% among nonfrail, prefrail, and frail subgroups respectively; whereas the incidence of ADL disability was 19.9, 30, and 44.6% in nonfrail, prefrail, and frail participants, respectively.
The unadjusted regression analysis showed that, in comparison with nonfrail subjects, frail participants had significant higher risk of incident mobility, IADL, and ADL disability. However, concerning the incidence of IADL disability, there was not an association with a frail or prefrail status. Multivariate logistic regression analysis showed that, after adjusting for sociodemo-graphic and health covariates, there were significant differences between prefrail and nonfrail subgroups,
but not between frail and nonfrail participants regarding the incidence of mobility disability. There is not an association between frailty and disability for IADL. Finally, concerning the incidence of ADL disability, there were significant differences between frail and nonfrail, but not between prefrail and nonfrail subjects (table III).
Mortality
Death incidence was 32.9% (n = 1 807) at the 11-year follow-up assessment (n = 251 between 2001-2003, and n = 1 556 between 2003 and 2012).
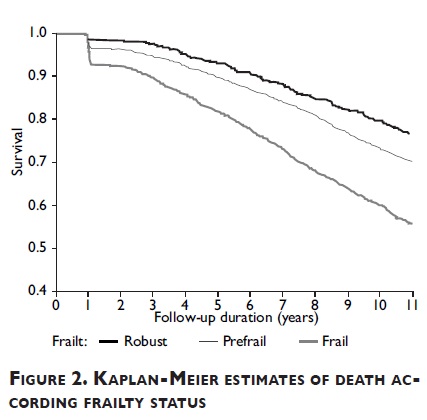
The cumulative risk of death was significantly increased in frail and pre-frail participants compared to robust subjects (log-rank test = 152.3, p < .0001). After two years of follow up, 7.6% fragile died, 3.7% pre-frail, against 1.9% robust. After 10 years of follow up, 39.9% of fragile died, 26.7% of pre-frail, against 20.4% robust (figure 2).
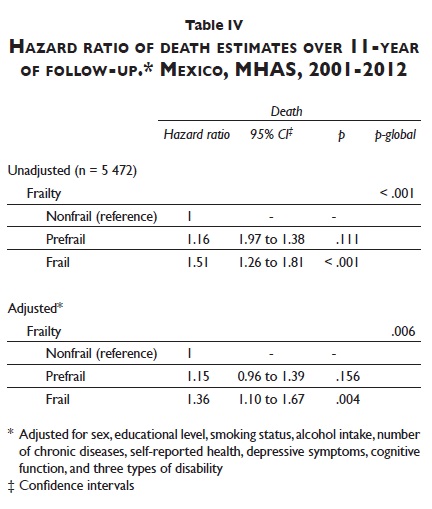
The unadjusted Cox proportional hazard model showed that, in comparison to nonfrail, being prefrail or frail at baseline significantly increased the risk of cumulative death at 11 years. After adjusting for multiple covariates including mobility, IADL, and ADL disability at baseline, there were significant differences between frail and nonfrail, but not between prefrail and nonfrail subgroups associated to mortality incidence. The risk of death for frail participants was increased by a factor of 1.36 (table IV).
Discussion
The results from the MHAS show that frailty is a frequent condition among the Mexican community-dwelling elderly and is an independent predictor of the incidence of disability and death, even after adjusting for potentially confounding variables. It is widely recognized that frail individuals have lower physiological capacity to adapt to stress, and therefore have a higher risk of adverse health-related outcomes than those non-frail subjects. Ours results partially replicate those previously described in other populations. This study, as far as we know, is one of the first to explore the predictive capacity of the phenotype of frailty in a cohort of older Mexican people over 10 years follow-up. Therefore, we are making a contribution to the growing interest in frailty studies among developing countries which may have greater vulnerability due to multiple factors, including limited socioeconomic, human and health resources that precipitate a greater burden of morbidity, disability, and decreased quality of life.
The main limitation of this study is the use of different metrics from those originally proposed by Fried and colleagues in order to define each of the frailty domains. The original proposed metrics were not available in the MHAS cohort. However, though the use of proxy criteria did not affect the predictive validity of the frailty phenotype, it could result in a possible overestimation of the prevalence of frailty. Slowness and low physical activity were particularly higher, which could partially explain the elevated prevalence of frailty. However, this same bias might also be present in previous studies of frailty in Latin American countries. For example, the results of a cross-sectional study of five Latin-American cities (SABE study) showed a prevalence of frailty ranged from 26.7 to 42.6%.4 In the same vein, a previous report of the MHAS has shown a prevalence of 33% frailty and 43% prefrailty. Our team already reported this higher prevalence of frail and prefrail persons in the MHAS.6 A recent systematic review incorporating 31 studies of frailty in persons aged 65 and older found a prevalence from 4.0 to 17.0% of frailty, markedly increased in subjects older than 80.19 Although the role of the components of frailty should be universal, it is possible that in the case of Mexico the prevalence of frailty may be influenced by other characteristics, such as inequality in health conditions, sociodemographics or genetic factors.20
Another limitation of our study is that disability was measured only one time at 11 years of follow up. This could result in a considerable number of disability events not registered because they did not last long enough to be measured given that disability can remit over time.
In addition, this higher prevalence may be due to differences in cultural elements that influence the perception of health and/ or the interpretation of questions concerning frailty. It has been reported that the phenotype of the Cardiovascular Health Study is useful to identify frail subjects, regardless of their ethnicity, which reinforces its validity across different cultures.21,22 In addition, the Hispanic Established Populations for Epidemiologic Studies of the Elderly (HEPESE) reported a frailty prevalence of 21% among Mexican-American elderly.23,24 European studies have shown similar inconsistencies among reports of frailty prevalence. For example, an epidemiological study conducted in France (n = 6 078, aged 64 and older) estimated the prevalence of frailty at 7.0%,25 whereas in a survey of 7 510 community-dwelling elderly in 10 European countries the prevalence of frailty was estimated to be between 9 to 60%; there was a higher prevalence in southern Europe.26 In previous studies, this geographic variation was not explained. This has led to studies which also evaluate the psychosocial factors associated with frailty.27,28,29
Nonetheless, despite these limits, the strengths of the study are its population-based design, sample size, almost complete older participants follow-up, and the adjustments for an extensive number of potential confounders.
Frailty has been studied in different populations, regarding its association with the risk of death and other adverse outcomes such as functional impairment. By assessing Mexican-American community individuals older than 70, in 2009 Graham JE and colleagues found that frail and pre-frail status increased the risk of death at 10 years follow-up.30
The main strength of this study relies on that it has provided an opportunity to recognize and describe frailty in populations that have specific sociodemographic and cultural circumstances. A better understanding of frailty will allow for complex care of adults suffering from the condition and allow researchers and caregivers to focus on the health needs of this population. Research should be encouraged in Latin-American countries, where little is known about frailty and where the prevalence of frailty could be underestimated, with terrible consequences for the health of elderly persons.
References
1. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146-M156. [ Links ]
2. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004;59:255-263. [ Links ]
3. Ensrud KE, Ewing SK, Cawthon PR Fink HA Taylor BC, Cauley JA. Osteoporotic fractures in men research group (2009).A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriat Soc 2009;57:492-498. [ Links ]
4. Alvarado BE, Zunzunegui MY Béland F, Bamvita JM. Life course social and health conditions linked to frailty in Latin American older men and women. J Gerontol A Biol Sci Med Sci 2008;63A1399-1406. [ Links ]
5. García-García FJ, Larrión-Zugasti JL, Rodríguez-Mañas L. Fragilidad: un fenotipo en revisión. Gac Sanit 2011;25 Suppl 2:51-58. [ Links ]
6. Aguilar-Navarro S, Gutiérrez-Robledo LM, García-Lara JM, Payette H, Amieva H, Ávila-Funes JA et al. The phenotype of frailty predicts disability and mortality among Mexican community-dwelling elderly. J Frailty Aging 2012;1:111-117. [ Links ]
7. Fried LP, Xue QL, Cappola AR, Ferrucci L, Chaves R, Varadhan R, et al. Nonlinear multisystem physiological dysregulation associated with frailty In older women: implications for etiology and treatment. J Gerontol A Biol Sci Med Sci 2009;64( 10): 1049-1057. [ Links ]
8. Rockwood, Bergman H. Frailty: a report from the 3rd joint workshop of IAGG 2012 Can Geriatr J 2012; 15:31 -36. [ Links ]
9. Morley J E. Vellas B, van Kan G, Anker S, Bauer J, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 20l3;14(6):392-397. [ Links ]
10. Wong R, Espinoza M, Palloni A. Adultos mayores mexicanos en contexto socioeconómico amplio: salud y envejecimiento. Salud Publica Mex 2007;49 supl 4:S436-S447. [ Links ]
11. Estudio Nacional sobre Salud y Envejecimiento en México (Enasem) 2001. Documento metodológico. Reporte de proyecto [internet document] [accessed April 13,2015]. México: Enasem, 2004. Available at: http://mhas.pop.upen.edu/espanol/documentos/Metodologico/Doc_metodologico-v2.pdf. [ Links ]
12. Nourhashemi F, Deschamps V, Larrieu S, Letenneur L, Dartigues JF, Barberger-Gateau P et al. Body mass index and incidence of dementia: the PAQUID study. Neurology 2003;60:117-119. [ Links ]
13. Larrieu S, Peres K, Letenneur L, Berr C, Dartigues JF, Ritchie K, et al. Relationship between body mass index and different domains of disability in older persons: the 3C study. Int J Obes Relat Metab Disord 2004;28:1555-1560. [ Links ]
14. Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc 1976;54:439-467. [ Links ]
15. Lawton MR Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179-186. [ Links ]
16. Katz S, Downs TD, Cash HR. Progress in the development of the ADL Index. Gerontologist 1976; 1:20-30. [ Links ]
17. Aguilar-Navarro SG, Fuentes-Cantú A, Avila-Funes JA, García-Mayo EJ. Validity and reliability of the screening questionnaire for geriatric depression used in the Mexican Health and Age Study. Salud Publica Mex 2007;49:256-262. [ Links ]
18. Glosser G. Wolfe N. Albert ML, Levine L, Steele JC, Calne DB. Cross-cultural cognitive examination: validation of a dementia screening instrument for neuroepidemiological research. J Am Geriatr Soc 1993;41:931-939. [ Links ]
19. Goldstein JRAndrew MK.Travers A. Frailty in older adults using prehospital care and the emergency department: a narrative review. Can Geriatr J 2012;15:16-22. [ Links ]
20. Díaz de León-González E. Tamez-Pérez HE, Gutiérrez-Hermosillo H. Cedillo Rodriguez JA Torres G. Frailty and its association with mortality, hospitalization and functional dependency among 60 year and older Mexican people. Med Clin (Bare) 2012;138:468-474. [ Links ]
21. Lacas A Rockwood K. Frailty in primary care: a review of its conceptualization and implications for practice. BMC Med 2012; 10:4. [ Links ]
22. Collard RM, Boter H, Schoevers RA Oude-Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487-1492. [ Links ]
23. Espinoza SE, Hazuda HP. Frailty in older Mexican-American and European-American adults: is there an ethnic disparity? J Am Geriatr Soc 2008;56:1744-1749. [ Links ]
24. Masel MC, Ostir GV, Ottenbacher KJ. Frailty, mortality, and health-related quality of life in older Mexican-Americans. J Am Geriatr Soc 2010;58:2149-2153. [ Links ]
25. Avila-Funes JA, Helmer C, Amieva H, Barberger-Gateau R, Le Goff M, Ritchie K, et al. Frailty among community-dwelling elderly people in France: the three-city study. J Gerontol A Biol Sci Med Sci 2008;63:1089-1096. [ Links ]
26. Santos-Eggimann B, Cuénoud R Spagnoli JJunod J. Prevalence of frailty In middle-aged and older community-dwelling Europeans living in 10 Countries. J Gerontol A Biol Sci Med Sci 2009;64:675-681. [ Links ]
27. Cesari M, Leeuwenburgh C, Lauretani F, Onder G, Bandinelli S, Maraldl C. Frailty syndrome and skeletal muscle: results from the Invecchiare in Chianti Study. Am J Clin Nutr 2006;83:1142-1148. [ Links ]
28. Alcalá MV, Puime AO, Santos MT, Barral AG, Montalvo JL, Zunzunegui MV. Prevalence of frailty in an elderly Spanish urban population. Relationship with comorbidity and disability. Aten Primaria 2010;42:520-527. [ Links ]
29. Espinoza SEJung I, Hazuda H.The Hispanic paradox and predictors of mortality in an aging biethnic cohort of Mexican-Americans and European-Americans: The San Antonio Longitudinal Study of Aging. J Am Geriatr Soc 2013;6:1522-1529. [ Links ]
30. Graham JE, Al Snih S, Berges IM, Ray LA Markides K, Ottenbacher K J. Frailty and 10-year mortality in community-living Mexican-American older adults. Gerontology 2009:55:644-651. [ Links ]
Received on: December 9, 2013
Accepted on: July 16, 2014
 Corresponding author:
Corresponding author:
Dr. José Alberto Avila Funes.
Departamento de Geriatría,
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán.
Vasco de Quiroga 15. 14000. Tlalpan, Mexico City, Mexico.
E-mail: avilafunes@live.com.mx.
Declaration of conflict of interests: The author declares not to have conflict of interests.













