Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de investigación clínica
versión On-line ISSN 2564-8896versión impresa ISSN 0034-8376
Rev. invest. clín. vol.59 no.2 Ciudad de México mar./abr. 2007
Artículo original
Aldosterone receptor antagonists induce favorable cardiac remodeling in diastolic heart failure patients
Antagonistas de receptores de aldosterona inducen remodelación cardiaca favorable en pacientes con insuficiencia cardiaca diastólica
Arturo Orea-Tejeda,*,** Eloísa Colín-Ramírez,*,** Lilia Castillo-Martínez,*,** Enrique Asensio-Lafuente,** Dora Corzo-León,* Rafael González-Toledo,* Verónica Rebollar-González,** Rene Narváez-David,** Joel Dorantes-García*
* Heart Failure Clinic.
** Cardiology Department. Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Mexico City.
Correspondence and reprint request:
Lilia Castillo-Martínez, MSc
Providencia 1218-A 402, Col. Del Valle,
03100, México, D.F.
Tel./fax: (5255) 5513-9384.
E-mail: camll225@yahoo.com
Recibido el 13 de junio de 2006.
Aceptado el 15 de diciembre de 2006.
ABSTRACT
Background. Serum levels of aldosterone in heart failure are increased up to 20 times compared to normal subjects. After an acute myocardial infarction, aldosterone increases progressively as well as interstitial fibrosis and collagen synthesis from cardiac fibroblasts, forming a patchy heterogeneous interstitial collagen matrix that affects ventricular function. Even if angiotensine converting enzyme inhibitors (ACEI) or angiotensin II receptor antagonists (ARA) can reduce aldosterone levels early during treatment, they increase again after a 12 week treatment. The aim of this study was to evaluate the changes in structure and function of the left ventricle in symptomatic (NYHA I-III) diastolic heart failure patients receiving an aldosterone receptor antagonist.
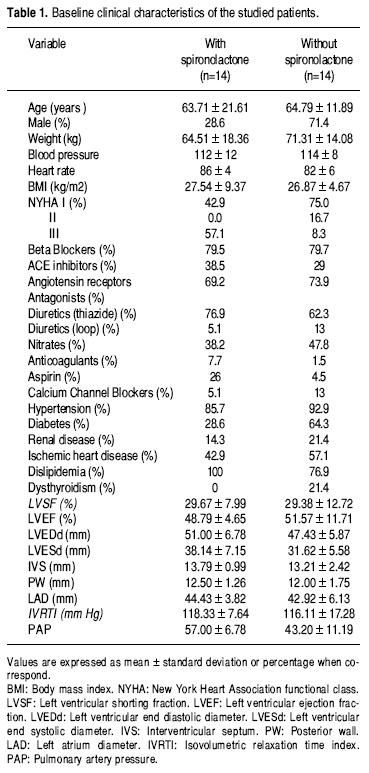
Methods. Twenty-eight subjects with diastolic heart failure, on BB, ACEI and/or ARA were randomized to receive spironolactone (group A) on a mean dose of 37.5 mg once a day (n =14, age 63.7 ± 21.6 years and body mass index, BMI 27.5 ± 9.4), or not (group B, n = 14, Age 64.8 ± 11.9, BMI 26.9 ± 4.7). All patients were followed-up for a mean of 13.79 ± 0.99 months.
Results. Group A showed a 42.8% ischemic origin of heart failure, while in group B was 55% (p = 0.2). No other co-morbidities were significativelly different among both groups. Mean percentage of changes by echocardiogram was as follows: Interventricular septum (IVS) -12.2 ± 11% vs. 1.3 ± 15.2 (p = 0.03), pulmonary systolic artery pressure (PSAP was 0.99 ± 3.8% vs. 10.5 ± 9.1, p = 0.05). Other parameters did not show statistically significant differences.
Conclusion. Aldosterone receptor antagonists reduce or avoid increasing of PSAP and inducing a favorable remodeling of the left ventricle, especially in the IVS in diastolic heart failure patients.
Key words. Aldosterone antagonist receptors. Diastolic heart failure.
RESUMEN
Antecedentes. En pacientes con insuficiencia cardiaca existen aumentos de aldosterona hasta 20 veces mayores que en sujetos control. Después de un infarto miocárdico la aldosterona aumenta progresivamente, así como la fibrosis intersticial y la síntesis de colágena por fibroblastos cardiacos, provocando parches intersticiales heterogéneos en la matriz de colágena que afecta la función ventricular. El tratamiento inicial con inhibidores de enzima convertidora de angiotensina (IECA) y/o antagonistas de receptores de angiotensina II (ARA) puede reducir estos niveles; sin embargo, aumentan nuevamente después de 12 semanas de tratamiento. El propósito de este estudio fue evaluar los cambios estructurales y funcionales en el ventrículo izquierdo en pacientes con insuficiencia diastólica tratados con ARA angiotensina (NYHAI-III).
Métodos. Veintiocho pacientes con insuficiencia cardiaca diastólica en tratamiento con BB, IECA y/o ARA se aleatorizaron a recibir una dosis media de 37.5 mg una vez al día de espironolactona (grupo A) (n - 14, edad 63.7 ± 0 21.6 años e índice masa corporal IMC 27.5 ± 9.4), o no (grupo B, n =14, edad 64.8 ± 11.9, IMC 26.9 ± 4.7). Todos los pacientes fueron seguidos por 13.79 ± 0.99 meses.
Resultados. De los pacientes del grupo A, 42.8% y el 55 del grupo B (p = 0.2), tenían cardiopatía isquémica. No se encontraron diferencias significativas en otras comorbilidades. El porcentaje promedio de cambios en el ecocardiograma se observó en septum interventricular (SIV) -12.2 ± 11% vs. 1.3 ± 15.3% (p = 0.02), y la presión sistólica de la arteria pulmonar (PSAP, 0.99 ± 3.8% vs. 10.5 ± 9.1, p = 0.05, para los grupos A y B, respectivamente). Los otros parámetros no mostraron diferencias estadísticamente significativas.
Conclusión. El tratamiento con antagonistas de receptores de aldosterona disminuye o limita aumentos de PSAP e inducen una remodelación favorable del ventrículo izquierdo, especialmente del SIV en pacientes con insuficiencia cardiaca diastólica.
Palabras clave. Antagonistas de receptores de aldosterona. Insuficiencia cardiaca diastólica.
INTRODUCTION
Myocardial hypertrophy is a common consequence of several co-morbidities, arterial hypertension and obesity are frequently involved through several mechanisms.1 The pathophysiology involves left ventricular remodeling in combination with several degrees of myocardial fibrosis that are finally associated to left ventricular dysfunction and a symptomatic heart failure state.2
Myocardial hypertrophy can be present in asymptomatic patients, including those with abnormal systolic or diastolic function; however, particularly in subjects with diastolic dysfunction, the early presence of effort symptoms like fatigue, and dyspnea are the rule.3
Experimental studies relate aldosterone in the genesis of myocardial fibrosis, hypertrophy and myocardial dysfunction.4,5 Hypothetic positions have considered that aldosterone antagonism could improve the outcome of systolic and diastolic heart failure because of its antifibrotic effects.6 In addition, clinical and experimental studies have associated aldosterone with abnormal vascular function7 and with diastolic dysfunction frequently accompanied by impairment of left systolic dysfunction despite a normal ejection fraction.8 Even if angiotensin converting enzyme inhibitors (ACEi) or angiotensin II receptor antagonists (ARA) medication can reduce aldosterone levels early during treatment, these increase again after a 12 week treatment. 9
We designed this study in order to examine the effects of aldosterone antagonism with spironolactone on myocardial structural and functional changes in heart failure patients with PRESERVED systolic function.
METHODS
Patients with diastolic heart failure attending to Heart Failure Clinic were considered eligible, independently of the etiology, if they had history of arterial hypertension (and/or were on antihypertensive treatment), but no history of angina, myocardial infarction or myocardial revascularization (PTCA and / or aorto-coronary by pass grafting) during the 3 months previous to recruitment and they referred fatigue, dyspnea on exercise and/or orthopnea. All patients were followed-up for a mean of 13.79 ± 0.99 months.
All patients had a TRANSTHORACIC echocardiogram study and an exercise treadmill test, at the beginning and at the end of the follow-up. Patients were consecutively randomized, independently of heart failure treatment, to receive spironolactone 25-50 mg once a day (Group A, n = 14) or to not receive spironolactone (Group B, n = 14). During the follow-up, clinical and laboratory evaluation were made bimonthly, with special emphasis in serum electrolytes (particularly potassium).
The echocardiogram was made by a Cardiologist blinded to the clinical evaluation and treatment received. Wide angle, two dimensional echoes were videotaped on a ¾ inches videocassette recorder with patients in left lateral decubitus position, using HP Sonos ultrasound 5000 imaging system. Apical four chambers and apical two chambers were the views selected for left ventricular long axis at the end diastole and at the end systole to calculate ejection fraction, and stroke volume. The echocardiograms were made according to the recommendations of the American Society of Echocardiography.
Ventricular dysfunction was diagnosed according recommendations of Heart Failure Society of America10 and I-Preserved trial11. Diastolic dysfunction was considered when the ejection fraction was over 45%, and shortening fraction = 28%, without severe segmental dyskynesia of the left ventricle, left atrial enlargement, or increased thickness of posterior wall, interventricular septum, and left ventricular mass index.
For comparisons between the groups we used Fisher's Exact Test for categorical and Mann-Whitney U Test for continuous variables. A p value < 0.05 was considered statistically significant. All analyses were performed using a commercially available package (SPSS for Windows, version 10.0, 1999 Chicago: SPSS Inc.).
RESULTS
Twenty-eight patients were included, 20 (71.42%) females and 8 males (28.57%). Characteristics of patients are presented in Table 1. Group A showed a 42.8% ischemic origin of heart failure, while in group B was 57.1% (p = 0.2). There were more women on spironolactone treatment compared with those without it, with no statistical significance. Co-morbidities and concomitant treatment were similar in both groups. In group A more patients were in functional clase III compared with group B. No other characteristics, co-morbidities or treatment were significativelly different among both groups. Blood pressure and results on exercise treadmill test, were similar in both groups at the beginning and at the end of the follow-up. Mean serum levels of potassium, creatinine, and the rest of laboratory test did not show significant differences at the beginning and at the end of follow-up (13.79 ± 0.99 months).
Regarding the echocardiographic parameters, the only significant change was the reduction in the interventricular septum dimension observed in patients receiving spironolactone compared with the control where an increased thickness was found (-12.2 ± 11 % vs. 1.3 ± 15.3 %, p = 0.02), as well as pulmonary arterial pressure (0.99 ± 3.8% us. 10.5 ± 9.1 p = 0.05) although this change was not statistically significant. No case required reduction of the drug dosage because of adverse events.
DISCUSSION
Aldosterone has been involved in vascular response to acetylcholine infusion, free oxygen radicals, TNF-α and other citokines production; however, the aldosterone receptors antagonists were able to block these effects.12 It has also been demonstrated an increase of pro-collagen pro peptide type I levels in blood samples from the coronary sinus, which is a fibrosis marker in hypertensive heart disease.13 An improved endothelial function in brachial artery flow at 4 weeks was demonstrated in CHF patients on conventional medical therapy. This benefit was still present after 8 weeks of treatment, presumably due to reversal of aldosterone impairment of endothelial nitric oxide activity.14 Duprez, et al.15 also demonstrated the presence of a good correlation between left ventricular mass index and aldosterone serum levels as well as an inverse correlation with this and the compliance of one proximal artery.
Heart failure patients on treatment with ACEI or ATI antagonist receptors, showed a regression to initial aldosterone serum levels after 12 weeks,9 indicating an aldosterone escape after this time. In addition, after acute myocardial infarction, an early remodeling process starts, and it could be reduced using earlier aldosterone receptors antagonists.16
Diastolic dysfunction is frequently accompanied by impaired left ventricular systolic function despite a normal ejection fraction.7,8 Monttram, et al.17 demonstrated that in an ambulatory hypertensive population with left ventricular preserved systolic function, myocardial function was improved after 6 months of aldosterone blocked with spironolactone, independently of the antihypertensive effect, as was demonstrated by no significant changes in ambulatory blood pressure.
In our cases, the most important structural change was observed in the diastolic interventricular septum thickness, while in other cases was most important in the left ventricular posterior wall.17 It is thus possible that in the presence of an adverse stimulus, myocardial wall responds with an heterogeneous hypertrophy distribution, perhaps depending on the coronary blood flow reserve, related to the angiographic coronary representation, as has been suggested in several types of systolic overload or in post infarction myocardial patients,18 and it could explain the differential beneficial effect in different segments.
Spironolactone antagonism has been associated with improvement of some indirect parameters of diastolic function as left atrial area19 and decrease in pulmonary venous A wave reversal velocity, consistent with reduction in left ventricular stiffness and /or end diastolic pressure.17 In this way, it is possible to infer that a lack of increase in pulmonary blood pressure, as observed in our group on spironolactone, could be related to an easier filling of the left ventricle as an indicator of improvement in diastolic function, even if such a change was not statistically significant, and unrelated to blood pressure levels.
Although there is not enough evidence to use specific agents to treat patients with diastolic heart failure,19 there is hypothetical support that optimization of antihypertensive treatment reduces the progression of myocardial hypertrophy and diastolic dysfunction. It has been suggested that blockade of type 1 angiotensin receptors reduces the left ventricular stiffness in hypertensive patients, and it was associated to myocardial fibrosis regression.20 In the same way, aldosterone blockade with spironolactone, an agent with more antifibrotic power and less antihypertensive effect, improved myocardial function in symptomatic patients with diastolic dysfunction, but not necessarily left ventricular hypertrophy.17
In our study, patients with diastolic heart failure were all treated with ACE inhibitors/ARA and Beta blockers, with a good antihypertensive treatment response in rest and in exercise in both groups.
They all showed a significant difference regarding the reduction of interventricular septum thickness that increased in the control group, suggesting that the most complete blockade of renin-angiotensin-aldosterone system improves myocardial structure and function in heart failure patients treated with spironolactone. These findings are in concordance with improvement in arterial stiffness with spironolactone in experimental studies with angiotensin receptor blockade.5
REFERENCES
1. Vasan RS, Levy D. The Role of hypertension in the pathogenesis of heart failure: a clinical mechanistic overview. Arch Intern Med 1996; 156: 1789-96. [ Links ]
2. Douglas PS, Talland B. Hypertrophy, fibrosis and diastolic dysfunction in early canine experimental hypertension. J Am Coll Cardiol 1991; 17: 530-6. [ Links ]
3. Orea-TA, Castillo-ML, Férez SS, Ortega SA. Programa Nacional de Registro de Insuficiencia Cardiaca. Resultados de un Estudio Multicéntrico Mexicano. Med Int Mex 2004; 20(4): 243-60. [ Links ]
4. Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstisium: fibrosis and renin-angiotensin-aldosterone system. Circulation 1991; 83: 1849-65. [ Links ]
5. Lacolley P, Safar ME, Lucet B, et al. Prevention of aortic and cardiac fibrosis by spironolactone in old normmotensive rats. J Am Coll Cardiol 2001; 37: 662-7. [ Links ]
6. Zannad F, Alia F, Dousset B, et al. Limitation of excessive extracellular matrix turnover may contribute to survival benefit of spironolactone therapy in patients with congestive heart failure: insights from the randomized aldactone evaluation study (RALES). Rales Investigators. Circulation 2000; 102: 2700-6. [ Links ]
7. Struthers AD. Impact of aldosterone on vascular pathophysiology. Congest Heart Failure 2002; 8: 18-22. [ Links ]
8. Poulsen SH, Andersen NH, Ivarsen PI, et al. Doppler tissue imaging reveals systolic dysfunction with hypertension and apparent "isolated" diastolic dysfunction. J Am Soc Echocardiogr 2003; 16: 724-31. [ Links ]
9. Staessen J, Lijnen P, Fagard R, et al. Rise in plasma concentration of aldosterone during long-term angiotensin II suppression. Endocrinol 1981; 91: 457-65. [ Links ]
10. Arnold JM, Massie BM, Baker DW, Mehra MR, Barnard DH, Miller AB, et al. HFSA 2006 Comprehensive HF Practice Guideline. J Card Fail 2006; 12(1): e1-e122. [ Links ]
11. Carson P, Massie BM, McKelvie R, McMurray J, Komajda M, Zile M, et al. The irbesartan in heart failure with preserved systolic function (I-PRESERVE) trial: rationale and design. J Card Fail 2005; 11(8): 576-85. [ Links ]
12. López B, Querejeta R, Varo N, et al. Usefulness of serum carboxy-terminal propeptide of procollagen type I in assessment of the cardioreparative ability of antihypertensive treatment in hypertensive patients. Circulation 2001; 104: 286-91. [ Links ]
13. Querejeta R, Lopez B, Gonzalez A, et al. Increased collagen type I synthesis in patients with heart failure of hypertensive origin: relation to myocardial fibrosis. Circulation 2004; 110: 1263-8. [ Links ]
14. Abiose AK, Mansoor GA, Barry M, et al. Effect of spironolactone on endothelial function in patients with congestive heart failure on conventional medical therapy. Am J Cardiol 2004; 93: 1564-6. [ Links ]
15. Duprez DA, Bauwens FR, De Buyzere ML, et al. Influence of arterial blood pressure and aldosterone on left ventricular hypertrophy in moderate essential hypertension. Am J Cardiol 1993; 71: 17A-20A. [ Links ]
16. Pitt B, Remme W, Zannad E, et al. Eplererone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348: 1309-21. [ Links ]
17. Mottram PM, Haluska B, Leano R, et al. Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation 2004; 110: 558-65. [ Links ]
18. Sánchez G, Orea A, Trevethan S, et al. La circulación coronaria en la hipertrofia asimétrica del septum interventricular. Acerca de una nueva hipótesis patogénica. Arch Inst Cardiol Mex 1984; 54: 235-44. [ Links ]
19. Douglas PS. The left atrium: a biomarker of chronicdiastolic dysfunction and cardiovascular disease risk. J Am Coll Cardiol 2003; 42: 1206-7. [ Links ]
20. Diez J, Querejeta R, Lopez B, et al. Losartan-dependent regression of myocardial fibrosis is associated with reduction of left ventricular chamber stiffness in hypertensive patients. Circulation 2002; 105: 2512-17. [ Links ]














