Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de investigación clínica
versión On-line ISSN 2564-8896versión impresa ISSN 0034-8376
Rev. invest. clín. vol.57 no.5 Ciudad de México sep./oct. 2005
Artículo original
Endoscopic retrograde cholangiopancreatography in the elderly
Colangiopancreatografía endoscópica retrógrada en el adulto mayor
José Alberto Ávila–Fuñes,* Aldo Montaño–Loza,** Sergio Zepeda–Gómez,*** Judith Meza–Junco,* Efrén Melano–Carranza,**** Francisco Valdovinos–Andraca,*** Miguel A. Valdovinos–Díaz,** Sergio Ponce de León–Rosales****
Departments of * Geriatrics,
** Gastroenterology,
*** Endoscopy and
**** Internal Medicine. Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán.
Reimpresos:
Dr. Aldo Montaño Loza
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Department of Gastroenterology.
Vasco de Quiroga # 15, Sección XVI, Tlalpan.
14080, Mexico City
Phone 5487–0900, ext. 2706. Fax: 5655–09–42.
Email: montano@quetzal.innsz.mx
Recibido el 10 de marzo de 2005.
Aceptado el 29 de junio de 2005.
ABSTRACT
Background. Endoscopic retrograde cholangiopancreatography (ERCP) is a widely used technique for the diagnosis and treatment of biliary and pancreatic diseases.
Objective. To know the complication rate of ERCP in the elderly.
Patients and methods. Patient files who underwent ERCP were reviewed and were divided into two groups: aged 65 and older (group 1) and less than 65 years (group 2). Sociodemographic variables, prophylactic antibiotic use, indications for ERCP and outcomes were assessed.
Results. Mean age in group 1 was 72.9 years and 41.7 years in group 2. Group 1 had more comorbidity (p < 0.001). The most frequent indication for the procedure was obstructive jaundice in both groups (63% versus 44%; p = 0.002). Malignancy was more frequent as a cause of biliary obstruction in group 1 (45% versus 21%; p < 0.001). ERCP was performed once in 76% in group 1 and 93% in group 2 (p = 0.001). Prophylactic antibiotics were used more frequently in group 1 (84% versus 60%; p < 0.001). There were no differences between groups regarding infectious complications (p = 0.700). There was no difference in mortality rates between groups.
Conclusion. ERCP is a safe procedure in elderly patients. The elderly frequently have more comorbidity. Nevertheless, the complication and mortality rates did not differ in this study. It is noteworthy that elderly patients received prophylactic antibiotics more frequently than younger patients but infectious complications were not different. The patients should not be excluded from ERCP based on their age.
Key words. ERCP. Jaundice. Elderly. Complication.
RESUMEN
Introducción. La colangiopancreatografia retrógrada endoscópica (CPRE) es un procedimiento ampliamente utilizado para el diagnóstico y tratamiento de las enfermedades biliares y pancreáticas.
Objetivo. Conocer la frecuencia de complicaciones de la CPRE en los adultos mayores.
Pacientes y métodos. Se revisaron los expedientes clínicos de pacientes que se sometieron a CPRE y se dividieron en dos grupos: de 65 años o mayores (grupo 1) y menores de 65 años (grupo 2). Se documentaron variables sociodemográficas, uso de antibióticos profilácticos, indicación de la CPRE y evolución.
Resultados. El promedio de edad fue de 72.9 años en el grupo 1 y 41.7 años en el grupo 2. El grupo 1 presentó mayor frecuencia de comorbilidad (p < 0.001). La indicación más frecuente para la realización del procedimiento en ambos grupos fue la ictericia obstructiva (63 vs. 44%; p = 0.002). El cáncer fue más frecuente causa de obstrucción en el grupo 1 (45 vs. 21%; p < 0.001). La CPRE se realizó una vez en 76% del grupo 1 y en 93% en el grupo 2 (p = 0.001). Los antibióticos profilácticos se utilizaron con mayor frecuencia en el grupo 1 (84 vs. 60%; p < 0.001). Sí bien, no hubo diferencias en relación con la frecuencia de complicaciones infecciosas (p = 0.700). No hubo diferencias en mortalidad entre los dos grupos.
Conclusión. La CPRE es un procedimiento seguro para los adultos mayores. Los adultos mayores frecuentemente presentan mayor comorbílídad. Sin embargo, la frecuencia de complicaciones y mortalidad no fue diferente en este estudio. Es importante señalar que los adultos mayores recibieron con mayor frecuencia antibióticos profilácticos que los pacientes de menor edad, pero la frecuencia de complicaciones infecciosas no fue diferente. No debe excluirse a los pacientes de la CPRE por su edad.
Palabras clave. CPRE. Ictericia. Adultos mayores. Complicaciones.
BACKGROUND
Since 1970s, endoscopic retrograde cholangiopancreatography (ERCP) changed the diagnosis and treatment of pancreatic and biliary disease. ERCP as gastrointestinal endoscopy has been proved to be a safe and useful procedure in the elderly population.1–9 Although ERCP is considered as a minimally invasive procedure, it has potential serious complications.1,2 The incidence of complications has risen with the increment in therapeutic interventions,1,3 especially when a sphincterotomy is performed or a stent is placed.12 The prevalence of complications varies among 5.4% to 10% whereas the mortality is reported between 0.5% to 4.7%.1–58,10–14
There are well–defined risk factors for post–ERCP complications: less than 59 years of age, opacification of the pancreatic duct and the absence of stones in the common biliary duct.1 Other proposed risk factors are: difficulty to cannulate the biliary duct, a previously cut sphincter, Oddi's sphincter dysfunction and the numbre of procedures done in the endoscopy unit.1,15,16 Due to their severity, infectious complications shall be discussed in a separate paragraph. Antibiotic prophylaxis is used based on the extrapolation of the results obtained in surgery of the biliary tract and their utility has not been proved convincingly.1–3
The aim of this study is to describe the prevalence of post–ERCP complications in the geriatric population in a universitary third level hospital.
PATIENTS AND METHODS
Patient clinical files were reviewed from subjects submitted to ERCP in a universitary tertiary referral center between May 2001 to May 2002. Data regarding age, gender, indication and results of the procedure and complications were collected. The use of prophylactic antibiotics (defined as the administration in the hour prior to the procedure, and up to two more doses afterwards) was noted.
The patients were divided in two groups according to their age: Group 1 > 65 years and Group 2 < 65 years.
Statistical analysis was performed with Student t test,  and Fisher exact tests. A p value < 0.05 was considered as statistically significant. For < the main variables 95% confidence intervals were calculated. All analyses were made on SPSS version 10.0 for Windows.
and Fisher exact tests. A p value < 0.05 was considered as statistically significant. For < the main variables 95% confidence intervals were calculated. All analyses were made on SPSS version 10.0 for Windows.
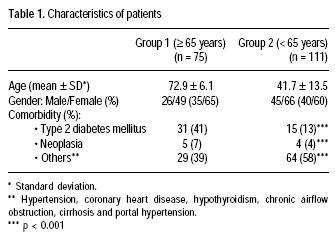
During the study period a total of 186 patients underwent ERCP were included. Group 1 was composed of 75 patients and group 2 had 111. The general characteristics are described in table 1. The average age for group 1 was 72.9 ±6.1 years and in group 2 the average age was 41.7 ± 13.5 years. Women predominated in both groups (p = 0.419). There was a higher comorbidity in group 1, where diabetes mellitus was the most frequent disease (p < 0.001).
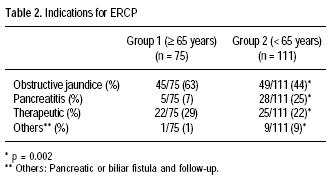
The evaluation of obstructive jaundice was the most frequent indication in both groups (63% versus 44%; p = 0.002). Malignant biliary obstruction was more frequent in group 1 (45% versus 21%; p < 0.001). Biliary tract drainage was more successful in those with < 65 years (76% versus 93%; p = 0.001). There were no differences in the way it was drained (p = 0.153); tables 2 and 3.
Complications are listed in table 4. The prevalence of any type of complication attributable to the procedure was not different between the groups (p = 0.590). There was one death in each group and was not related to ERCP. There were no differences related to the number of infectious complications (7/75 [8%], p = 0.700 [95% IC 0.34–0.93] versus 11/111 [10%], p = 0.611 [95% IC 0.35–0.82]). Antibiotic prophylaxis were used more frequently in group 1 (63/ 75 [84%] versus 67/111 [60%]; p < 0.001). Of those who did not receive prophylaxis, only two had an infectious complication (p = 0.065). There were no differences between the group that did receive prophylaxis and the group that had a formal antibiotic regime (p =0.572).
DISCUSSION
Endoscopic retrograde cholangiopancreatography has shown to be a safe and well tolerated procedure in the geriatric patient. As in other series, the incidence of complications seems to be independent of age.1,17 The group aged 65 and older had a significant higher comorbidity and increment in morbi–mortality could be expected, this was not true. The prevalence of complications was not different between the groups, however, the overall frequency was slightly higher than the reported elsewhere.1,10,16,18,19 This is probably related to the hospital population, a third level reference hospital with a sicker population.
The indications for the procedure and the findings were similar as those of other groups.1,18,20
Even though the benign obstruction was the most frequent finding in both groups, the malignant obstruction was significantly higher in our series; this is a reflection of the population in our hospital. The number of instrumentations in the biliary tract was similar between both groups and the rate of successful drainage in younger subjects was similar to other series (93%). This was not repeated in the older subjects where the rate of success was 76%, related to the high frequency of malignant stenosis which is harder to cannulate.8,20,21 Still, ERCP is a safer procedure to drain the biliary duct than surgery, with a less than one percent mortality.22–27
The fear of major complications associated with ERCP in the geriatric population limits its use and its benefits. As in other series, this study show ERCP to be a safe procedure in this patients, even in the very elderly people, with a rate of complications (infectious and non infectious) similar to that of the younger group.10–18–21–22–28–30
Nevertheless, it is worth to mention that in our series, the older group received more antibiotic prophylaxis than the other group. The incidence of infectious complications was very low and was not different between the two groups. Maxton et al. reported an incidence of post–ERCP colangitis of 26% in patients which required an endoprothesis placement.20 Thirty–six percent of the patients in the older group required a prothesis, we didn't observe such incidence.
It is not clear if this is the result of the antibiotic prophylaxis because its use is not recommended widely.31–35 The results in these studies support our findings in which only two patients who did not receive antibiotics had an infectious complication. More research is needed to define why older patients receive more antibiotics and if prophylaxis is necessary in this group of patients.
In conclusion, our series demonstrates that in patients aged 65 and older ERCP is a safe procedure; the incidence of complications is similar to the reported for the younger subjects. Even though the use of antibiotic prophylaxis is wider in the older population, there is no evidence that this practice is the causal effect of the same incidence of infectious complications in the younger group, so its use should be individualized accordingly to comorbidity and clinical circumstances of the patient. Our results support the existing evidence that a patient must not be excluded of the benefits of ERCP based on their age.
REFERENCES
1. Oi I, Kobayashi S, Kondo T. Endoscopio pancreatocholangiography. Endoscopy 1970; 2: 103–6. [ Links ]
2. Kawai K, Akasaka Y, Murakami K, et al. Endoscopio sphincterotomy of the ampulla's Vater. Gastrointest Endosc 1974; 20: 148–51. [ Links ]
3. Siddique I, Galati J, Ankoma–Sey V, et al. The role of choledoscopy in the diagnosis and management of biliary tract diseases. Gastrointest Endosc 1999; 50: 67–73. [ Links ]
4. Cotton PB. Evaluating ERCP is important but difficult. Gut 2002; 51: 287–9. [ Links ]
5. Lockhart SP, Schofield PM, Gribble RJN, et al. Upper gastrointestinal endoscopy in the elderly. BMJ 1985; 290: 283. [ Links ]
6. Brussaard CC, Vandewoude MFJ. A prospective analysis of elective upper gastrointestinal endoscopy in the elderly. Gastrointest Endosc 1988; 34: 118–21. [ Links ]
7. De la Mora G, Marcon NE. Endoscopy in the elderly. Best Pract Res Clin Gastroenterol 2001; 15: 999–1012. [ Links ]
8. MacMahon M, Walsh TN, Brennan P, et al. Endoscopio retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology 1993; 39: 28–32. [ Links ]
9. Seinelä L, Ahvenainen J, Rönneikkö J, et al. Reasons for and outcome of upper gastrointestinal endoscopy in patients aged 85 years or more: retrospective study. BMJ 1998; 317: 575–80. [ Links ]
10. Scapa E, Berant A, Leibovitz A, et al. Endoscopic retrograde cholangiopancreatography in octagenarians. J Clin Gastroenterol 1996; 22: 21–2. [ Links ]
11. Cooper BT, Neumann CS. Upper gastrointestinal endoscopy in patients aged 80 years or more. Age Ageing 1986; 15: 343–9. [ Links ]
12. Safe AF, Owens D. Upper gastrointestinal endoscopy in octogenarians. Br J Clin Pract 1991; 45: 99–101. [ Links ]
13. Sugiyama M, Atomi Y. Endoscopic sphinterotomy for bile duct stones in patients 90 years of aged and older. Gastrointest Endosc 2000; 52: 187–91. [ Links ]
14. Elizondo J, Gallo S, Valdovinos MA, et al. Retrospective evaluation of 500 endoscopic cholangiopancreatographies performed at the Instituto Nacional de la Nutrición Salvador Zubirán. Rev Gastroenterol Mex 1989; 54: 19–26. [ Links ]
15. Loperfido S, Angelini G, Benedetti G. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc 1998; 48: 1–10. [ Links ]
16. Cotton PB. Outcomes of endoscopy procedures: Struggling towards definitions. Gastrointest Endosc 1994; 40: 514–18. [ Links ]
17. Freeman ML, Nelson DB, Sherman S. Complications of endoscopic biliarysphincterotomy. N Engl J Med 1996; 335: 909–18. [ Links ]
18. Tanner AR. ERCP: Present practice in a single region. Suggested standards for monitoring performance. Eur J Gastroenterol Hepatol 1996; 8: 145–8. [ Links ]
19. Margulies C, Siquiera ES, Silverman WB. The effect of endoscopic sphincterotomy on acute and chronic complications of biliary endoprostheses. Gastrointest Endosc 1999; 49: 716–19. [ Links ]
20. Maxton DG, Tweedle DR, Martin DF. Retained common bile duct stones after endoscopic sphinterotomy: temporary and long–term treatment with biliary stenting. Gut 1995; 36: 446–9. [ Links ]
21. Ashton CE, McNabb WR, Wilkinson ML, et al. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Aging 1998; 27: 683–8. [ Links ]
22. Subhani JM, Kibbler C, Dooley JS. Review article: Antibiotic prophylaxis for endoscopic retrograde cholangiopancreatography (ERCP). Aliment Pharmacol Ther 1999; 13: 103–16. [ Links ]
23. Cotton PB, Lehman G, Vennes J. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastroenterol Endosc 1991; 37: 383–93. [ Links ]
24. Ingoldby CJH, El–Saadi J, Hall RI. Late results of endoscopic sphincterotomy for bile duct stones in elderly patients and gallbladder in situ. Gut 1989; 30: 1129–31. [ Links ]
25. Crocker JR, Williams SG, Charlton M. Endoscopic therapy for bile duct stones in geriatric population. Post Med J 1992; 68: 457–60. [ Links ]
26. Masci E, Toti G, Mariani A. Complications of diagnostic and therapeutic ERCP: A prospective multicenter study. Am J Gastroenterol 2001; 96: 417–23. [ Links ]
27. Ho KY, Montes H, Sossenheimer MJ. Features that may predict hospital admission following outpatient therapeutic ERCP. Gastrointest Endosc 1999; 49: 587–92. [ Links ]
28. Fleischer DE. Better definition of endoscopic complications and other negative outcomes. Gastrointest Endosc 1994; 40: 511–14. [ Links ]
29. Mitchell RMS, O'Connor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol 2003; 36: 72–4. [ Links ]
30. Deans GT, Sedman P, Martín D, et al. Are complications of endoscopic sphincterotomy age related? Gut 1997; 41: 545–8. [ Links ]
31. Shemesh E, Czerniak A, Shneabaum S. Early endoscopic sphincterectomy in the management of acute gallstone pancreatitis in elderly patients. JAGS 1990; 38: 893–6. [ Links ]
32. Mehta SN, Pavone E, Barkun JS, et al. Predictors of post–ERCP complications in patients with suspected choledocholithiasis. Endoscopy 1998; 30: 457–63. [ Links ]
33. Montaño–Loza A, Valdovinos F, Valdovinos MA. Profilaxis antimicrobiana en colangiopancreatografia retrógrada endoscópica. Rev Gastroenterol Mex 2002; 67 (Suppl. 1): 132–3. [ Links ]
34. Dajani AS, Taubert KA, Wilson W. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. JAMA 1997; 277: 1794–1801. [ Links ]
35. Meijer WS, Schmitz PI, Jeekel J. Meta–analysis of randomized, controlled clinical trials of antibiotic prophylaxis in biliary tract surgery. Br J Surg 1990; 77: 283–90. [ Links ]














