Introduction
Elastofibroma dorsi (ED) is a benign lesion of unknown pathogenesis that is most often located in the subscapular or pericapsular region but has also been reported in rare regions such as the deltoid, ischial, olecranon, gluteus maximus muscle, stomach, mediastinum, omentum, and tricuspid valve1,2. Although ED is usually slow-growing and asymptomatic, the diagnosis of ED is important because it may mimic malignant tumors of the thoracic wall1. Some patients may experience back pain and limited shoulder mobility1,3. ED etiology is thought to include tissue responses to trauma or vascular damage, ultimately leading to the formation of a mass characterized by infiltration of adipocytes and deposition of abnormal collagen and elastic fibers.
The common approach for ED is surgical excision when the tumor is < 5 cm or symptomatic4,5. However, due to the lack of a comprehensive series examining the diagnosis and treatment of ED, opinions vary on how to manage the disease. In this study, we present and discuss the clinical, radiological, and surgical findings of ED patients who underwent surgery at our clinic in light of current literature.
Material and methods
The study was approved by the Clinical Studies Ethics Committee of Tokat Gaziosmanpasa University Faculty of Medicine (Approval No. 22-KAEK-097), and all steps were carried out in compliance with the Declaration of Helsinki. Twenty patients who were diagnosed with ED at Tokat State Hospital and underwent surgery at our clinic between 2007 and 2022 were included in the study. Data from these patients were retrospectively evaluated in relation to demographic information, profession, complaints, presence of local recurrences, and follow-up and post-operative observations.
Patients with signs of swelling in the subscapular region underwent a physical examination followed by a magnetic resonance image (MRI) to evaluate the tumors position and its relationship with surrounding tissue (Fig. 1A and B). No diagnostic biopsies were performed before surgery. Any post-operative recurrences or other anomalies were evaluated using ultrasonography.
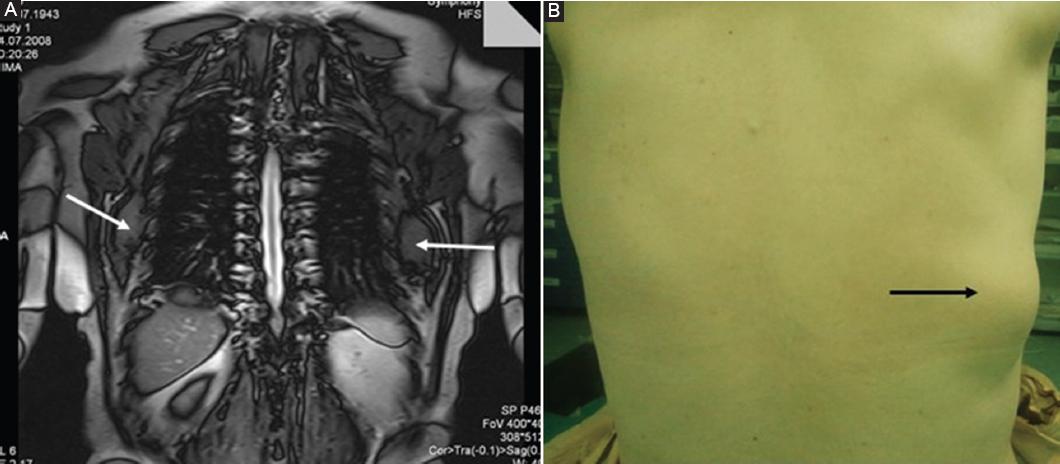
Figure 1 A: T1-weighted coronal magnetic resonance image of ED in a case with bilateral involvement (white arrows). B: view of ED in the lower corner of the scapula (clearly visual with anterior flexion of arm black arrow).
All patients underwent marginal resections of their tumors under general anesthesia. In the prone position, an incision was made along the border of the scapula, and the mass was meticulously resected from the thoracic cage and subscapular area by blunt and sharp dissection. Bilateral cases were operated on in a single session. Immobilization of the shoulder, hemovac drainage, and garments (elastic bondage) were used in all patients. Hemovac drains were removed on the 3rd post-operative day.
For the evaluation of pre-operative and post-operative pain, the Numerical Rating Scale (NRS) was used. NRS is an assessment in which patients rate their pain on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain. This scale is applied by the patient verbally or in writing.
Results
Sixteen of the study patients (80%) were female, and 4 (20%) were male. Swelling and back pain were the main complaints in 80% of patients, and a visual mass was observed in all patients in the subscapular region during anterior flexion of the arm (Fig. 1B). Limited shoulder mobility was observed in twelve patients (30%), and four (20%) were asymptomatic. An opening snap was observed in two patients (10%). The mean age was 61 years (with an overall age range of 41-74). Bilateral tumors were present in ten patients (50%), and unilateral lesions were more common on the right side (60%) (Table 1). Excisional surgery was performed on all patients, and tumors were completely removed (Figs. 2A and B).
Table 1 Clinic details of 20 patients operated on for elastofibroma dorsi
| AGE | G | BP | Swelling | OP | LSM | Site | Profession | NRS (Pre-post) |
|---|---|---|---|---|---|---|---|---|
| 74 | F | + | + | + | + | B | Housewife | 6-2 |
| 41 | M | + | - | - | - | R-U | Policeman | 4-0 |
| 68 | F | + | + | - | + | B | Housewife | 5-1 |
| 60 | F | + | + | - | + | B | Housewife | 7-2 |
| 50 | F | + | + | - | - | B | Lawyer | 4-0 |
| 54 | F | + | + | - | + | R-U | Tailer | 5-1 |
| 60 | M | + | + | - | + | B | Officer | 4-0 |
| 62 | F | + | + | - | + | B | Housewife | 7-2 |
| 59 | M | - | + | - | - | L-U | Officer | 0-0 |
| 66 | F | + | + | - | + | R-U | Engineer | 4-0 |
| 64 | F | + | + | + | + | L-U | Teacher | 5-1 |
| 66 | F | - | + | - | - | B | Housewife | 0-0 |
| 64 | F | + | - | - | + | R-U | Housewife | 7-2 |
| 66 | F | - | - | - | - | R-U | Housewife | 0-0 |
| 57 | M | + | + | - | + | L-U | Barber | 4-0 |
| 55 | F | - | - | - | - | L-U | Nurse | 0-0 |
| 64 | F | + | + | - | - | B | Housewife | 8-1 |
| 64 | F | + | + | - | + | B | Housewife | 6-1 |
| 60 | F | + | + | - | - | R-U | Housewife | 7-1 |
| 66 | F | + | + | - | + | B | Housewife | 8-2 |
BP: back pain; OP: opening snap; LSM: limited shoulder mobility; R: right; L: left; B: bilateral; U: unilateral; NRS: numerical rating scale (preoperative-post-operative).
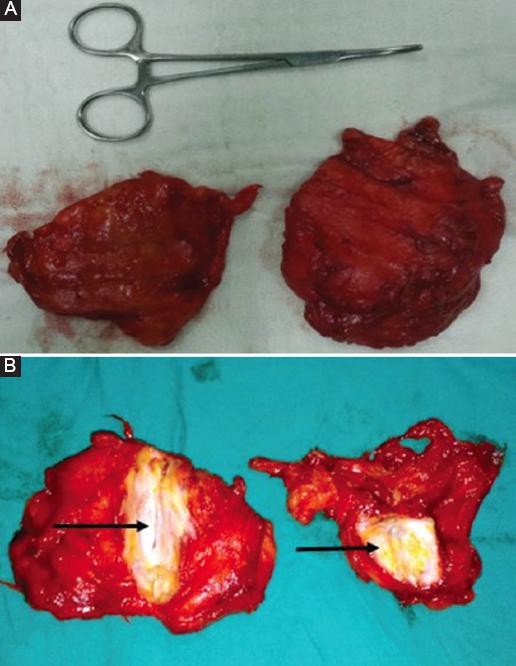
Figure 2 A: macroscopic view of bilaterally excised ED tumor; rubbery solid mass with undefined borders. B: cut surface of tumor; white-gray rubbery tissue containing yellow fatty islands (black arrows).
Although the follow-up period was lengthy (6-53 months, mean of 26.6 months), no recurrences were observed. Two (10%) patients required simple needle aspiration of post-operative seroma, and 1 patient (5%) needed evacuation due to infection.
Discussion
ED was first described in 1959 by Jarvi and Saxen and has since been reported in 19616,7. ED is a rare and benign soft-tissue tumor that typically occurs between the latissimus dorsi and serratus anterior muscle groups in the subscapular region. The tumor is firmly attached to the thoracic wall between the sixth rib and the eighth8. It is controversial whether ED is a true tumor, and its etiology is considered to be multifactorial. Recent studies suggest that the incidence of ED may be higher in individuals who engage in physical work that involves trauma to this area, but it has been reported in such regions as mediastinum and omentum, seemingly contradicting this theory1. Genetic anomalies, including mutations in the Xq12-q22 region and chromosome 19, may play a role in the development of ED, as some have suggested9. As was true in our study, ED is known to be more common in females, especially those over 55 years of age10. In elderly females, reactive fibromatosis and secondary degeneration of elastic fibers due to vascular insufficiency have been proposed as another theory for etiology, but it has also been reported in young individuals11.
ED is typically asymptomatic. However, when symptoms do occur, patients can experience swelling and pain in the subscapular region and limited shoulder mobility, such as friction, stiffness, and an opening snap. Due to the diverse symptomatology of ED, as a differential diagnosis, cervical lesions and rotator cuff tears must be kept in mind12. In our study, visual mass from anterior flexion of the arm and back pain in the subscapular region were the main symptoms. The suggested association between ED and physical activity, along with more frequent involvement of the dominant limb, may explain the observation that ED arises more often on the right side. ED has commonly been reported as unilateral. However, half of the patients in our study had bilateral involvement, and there have also been reports of bilateral involvement up to 66% due to the asynchronous development of tumors13.
The diagnosis of ED is usually based on clinical examination and radiological imaging. The mass can be more easily palpated when the arm is flexed anteriorly13,14. MRI is the preferred imaging modality as it can accurately determine the size of the tumor, its borders, and its relationship with the surrounding tissue8,15. In a typical ED MRI, the interposed areas of decreased signal intensity also appear as low signal intensity on T2-weighted sequences16.
The data regarding the value of diagnostic biopsies are not conclusive. Although some authors suggest that a fine needle or open biopsy may be useful in supporting the diagnosis, others argue that a basic clinical examination and radiological findings are sufficient13. In our study, patients were diagnosed based on physical examinations and typical MRI results, with no indication of suspected malignancy. Therefore, no biopsies were performed, as a complete resection of the tumors was proposed as the treatment approach. Some authors have also suggested surgery in asymptomatic patients to confirm the diagnosis or address possible malignant pathology17,18. All our asymptomatic patients (20%) refused follow-up and preferred surgery because of fear of cancer and cosmetic reasons. NRS is reliable in evaluating pain improvements in elderly patients19.
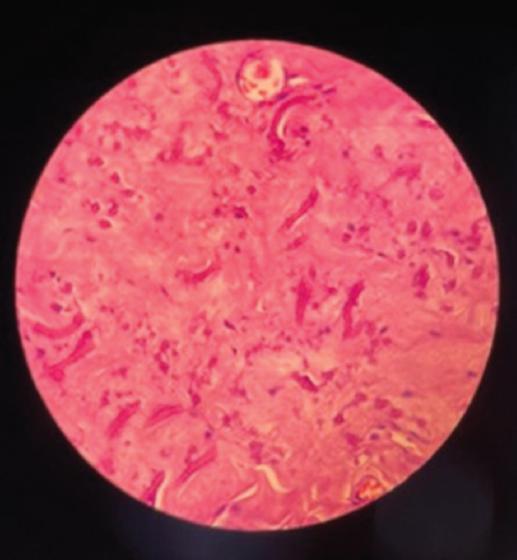
The macroscopic appearance of tumors is typically poorly defined as a non-encapsulated mass with a rubbery consistency and a cut-surface containing white and yellow areas due to fibrous and fatty tissue. Histological examination has demonstrated it to be a collagenous tissue mixed with eosinophilic fragmented elastic fibers (Fig. 3).
Seromas and hematomas are the most common post-operative problems after ED resection, as they result from the dead space introduced during surgery and damaged adherent surrounding tissue while separating from the mass5. Measures such as bleeding control, placement of appropriate drains without suturing the skin, shoulder immobilization, and bandaging after the procedure can minimize these problems. Our post-operative complication rates were 10% for seroma and 5% for infection, which is in accordance with statistics from the literature1. In different series, seroma has been reported at 10-40%, which is probably due to tumor size leading to dead space5,8. Some authors suggest talc insufflation when drainage is over 50 cc. and persistence after 3 days5. Overall, our findings suggest that surgical resection is a safe and appropriate therapeutic approach for ED following a diagnosis based on physical examination and MRI.
Conclusion
ED is a subscapular pathology that pre-dominantly affects elderly females. While the diagnosis can be made based on clinical and radiological data, a biopsy or surgical excision may be advised if there is a suspicion of malignancy. Our findings suggest that marginal resection of the tumor is a safe treatment option with minimal morbidity that may be best suited for symptomatic patients or when malignancy is suspected.











 nueva página del texto (beta)
nueva página del texto (beta)