Introduction
Vascular compression of the duodenum was first described by Rokitansky, in 1842, the first successful surgical procedure (duodenojejunostomy) was performed by Stavely, in 19081,2.
Superior mesenteric artery (SMA) syndrome, also known as Wilkie’s syndrome, is a rare cause of small bowel obstruction. Its exact incidence is unknown. It is caused by a reduction of the aortomesenteric angle3. There are several predisposing factors for this condition being weight loss the most significant one and other causes include the abdominal compression by a girdle or plaster cast or it can be idiopathic4. Most of the time, the diagnosis is a challenge but should be suspected based on clinical presentation and patient’s history. Conservative treatment has a place in managing such cases, especially acute ones. Failure of conservative management warrants surgical intervention3.
Clinical case
The patient is a 36-year-old female with a medical history of diabetes mellitus type 2 of a recent diagnosis. She began complaining of nausea, bilious vomiting, and a recent weight loss of 12 kg in the past 3 months. An esophagogastroduodenoscopy showed a dilated stomach but no evidence of gastric outlet obstruction. However, the study demonstrated an extrinsic partial obstruction of the third part of the duodenum (Fig. 1), with important dilation proximally. Thereafter, the patient underwent contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis that revealed a dilated stomach and duodenum up to the level of the third part, and a sudden narrowing just anterior to the abdominal aorta and posterior to the SMA; also, a significant reduction of the aortomesenteric angle and distance was seen (Fig. 2), being of 13° and 6 mm, respectively. With these clinical and radiologic findings, the diagnosis of SMA syndrome was made. The patient was admitted and started on IV hydration and gastric decompression through a nasogastric tube and total parenteral nutrition. The patient did not improve with conservative treatment so a surgical procedure was planned.
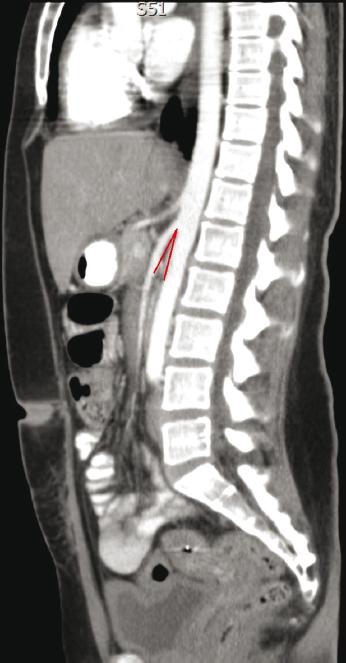
Figure 2 Double contrast-enhanced computed tomography scan where an aortomesenteric angle of 13° is observed.
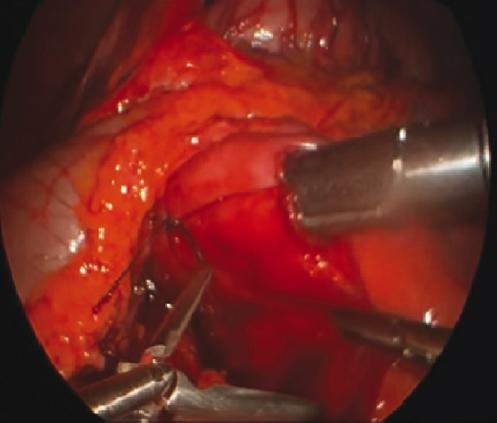
The patient was taken to the operating room for a laparoscopic duodenojejunostomy. The proximal duodenum was dilated while the jejunum appeared to be normal. A Kocher maneuver was performed, revealing no pancreatic or duodenal masses. The ligament of Treitz was identified, and a portion of jejunum approximately 20 cm distal to the ligament of Treitz was found to easily reach the duodenum. A silk suture was placed between the duodenum and jejunum, acting as a bridge of these two portions of the bowel. A duodenotomy was made in the lateral aspect of the second portion of the duodenum avoiding the ampulla. An antimesenteric jejunotomy is made in a similar way with electrocautery and then a 60 mm laparoscopic linear stapling device was used to create a side-to-side anastomosis (duodenojejunostomy) (Fig. 3). The common enterotomy was closed using a running 2-0 PDS suture in a single layer. A reinforcement suture was placed at the apex of the anastomosis. Intraoperative endoscopy was performed to evaluate the anastomosis and then air leak test was negative. There was no need for placing drains or nasogastric tube. The patient did well following surgery, she was gradually advanced to a soft diet and was discharged home on post-operative day 5 without complications.
Discussion
SMA syndrome is a rare condition whose incidence ranges from 0.0024% to 0.34% for the general population5. In this entity, the third part of the duodenum is compressed by SMA at its origin and abdominal aorta due to decreased angulation predisposing to partial or complete obstruction6.
Anatomically, the normal range of aortomesenteric angle varies between 25° and 60° and aortomesenteric distance ranges between 10 mm and 28 mm, in this case, the measurements were 13° and 6 mm, respectively. The third part of the duodenum lies just posteroinferior in relation to SMA. Any loss in retroperitoneal fat might reduce that angle and leads to Wilkie’s syndrome7,8.
Several factors may alter the aortomesenteric angle. The most common is significant weight loss, which leads to loss of retroperitoneal fat, which, in turn, leads to obstruction. SMA syndrome is commonly associated with severe chronic debilitating illnesses, such as cancer, malabsorption syndromes, AIDS, trauma, burns, and even surgery, especially those that distort anatomy9.
The most commonly affected patients are females aged between 10 and 40 years10. Patients might present with acute symptoms of bowel obstruction as in this case or more commonly with chronic symptoms as recurrent abdominal distention, abdominal pain, postprandial fullness, or early satiety. When lying supine, pain can be aggravated, that is, why patients typically assume the knee-chest position after eating, which widens the aortomesenteric angle, relieving their partial duodenal obstruction temporarily, and allowing the passage of gastric contents through the narrowed area11.
Due to its insidious onset, SMA syndrome diagnosis is a true challenge. Based on patient’s medical history, clinical presentation, and supported by imaging tests, we could get to the right diagnosis. Barium studies might show duodenal and even gastric dilatation with slow gastroduodenojejunal transit. Endoscopy might show an extrinsic compression and narrowing at the level of the third part of the duodenum. Contrast-enhanced CT or magnetic resonance angiography allows adequate visualization of the vascular compression of the duodenum and precise measurement of the aortomesenteric angle and distance, which is a very valuable information for diagnosis and for planning a surgical treatment12.
Conservative treatment is recommended as initial therapy of the SMA syndrome13. The use of total parenteral nutrition or an aggressive nutrition regimen through tube feeding usually a nasoyeyunal tube may help; these strategies are aimed at increasing the volume of the retroperitoneal fat pad widening the aortomesenteric angle, and in this way, providing relief of the symptoms14.
If conservative treatment fails, a surgical procedure to bypass the obstruction should be considered. The procedure of choice, with a success rate of up to 90%, is duodenojejunostomy15. Another option and relatively simpler operation can be called Strong’s procedure, which involves a section of the ligament of Treitz with mobilization of the duodenum. Gastrojejunostomy has been reported in literature as another treatment option, because of the increased post-operative complication rate such as blind loop syndrome and recurrence of symptoms, it is the rarely used10.
Conclusions
Wilkie’s syndrome is a rare cause of bowel obstruction that always should be kept in mind. The history of persistent vomiting and weight loss is characteristic in this entity. Panendoscopy is useful to rule out other causes of mechanical duodenal obstruction. The double contrast-enhanced CT scan is a considerable useful tool for planning the surgical treatment.
Laparoscopic duodenojejunostomy is a practical option to treat Wilkie’s syndrome. It provides definitive treatment with the advantages and benefits of minimally invasive surgery.











 nueva página del texto (beta)
nueva página del texto (beta)