Introduction
Patellofemoral instability (PFI) is a common disorder in children and adolescents, with an incidence ranging from 5.8 to 29 per 100,000 individuals aged 10 to 17 years.1 Surgical patellar stabilization poses challenges in skeletally immature patients owing to anatomical peculiarities at this stage, resulting in the absence of an established standard reconstruction technique. While various techniques have been described, not all achieve adequate reproduction of the anatomy of the medial stabilizers. Non-anatomic reconstructions may increase forces in the patellofemoral joint beyond normal levels, failing to fully restore normal knee kinetics.2
Recently, significant interest has emerged in the medial patellofemoral complex (MPFC).3,4,5 The term MPFC is used to describe the primary soft tissue stabilizer of the patella, consisting of fibers attached to the patella (medial patellofemoral ligament, or MPFL) and the quadriceps tendon (medial quadriceps tendon femoral ligament, or MQTFL), restricting lateral translation of the patella at various knee flexion angles.
The objective of this article was to describe the surgical technique used by the authors to reconstruct the medial patellofemoral complex with allografts in skeletally immature patients with patellofemoral instability.
Surgical technique
Indications:
The current indications for MPFC reconstruction are as follows:
First episode of patellar dislocation associated with a displaced osteochondral fracture.
Recurrent patellofemoral instability.
Habitual or obligatory patellofemoral instability.
Fixed lateral patellofemoral instability.
Procedure description:
Patient positioning and anesthesia:
The patient is placed in the supine position.
Spinal anesthesia is administered along with a pneumatic tourniquet.
Asepsis and antisepsis of the area are performed, and surgical drapes are placed according to the required technique.
Exsanguination of the affected limb is achieved using an Esmarch bandage, and a tourniquet is applied at 250 mmHg.
The superomedial patellar and femoral approaches, as well as arthroscopic portals, are delineated using a sterile marking pen (Figure 1).
Diagnostic arthroscopy:
Classic anterolateral and anteromedial arthroscopic portals are created, and diagnostic arthroscopy is performed to identify loose bodies and evaluate patellofemoral chondral surfaces. Any osteochondral or chondral injuries are addressed at this point.
Allograft preparation:
Preferable sources for allografts are the semitendinosus or peroneus longus. The tibialis anterior or posterior can also be used but typically requires graft sizing to ensure that it does not exceed a thickness of 6 mm.
Ensure that the allograft has a minimum length of 240 mm.
After thawing, wash the allograft with an antibiotic-saline mixture containing 1 g of vancomycin in 1 liter of normal saline. Apply tension to the allograft using the graft preparation board, and place a whip stitch on each side of the graft using a #1 Vicryl suture.
Superomedial patellar approach:
A 3 cm incision is made at the superomedial pole of the patella.
Dissection is carried out to visualize the medial border of the quadriceps tendon.
The plane between the medial retinaculum and the joint capsule is identified, taking care to avoid capsule damage.
Femoral fixation:
A C-arm is used to precisely identify the radiographic reference point in the epiphyseal region just distal to the growth plate.6,7
-
A guidewire is introduced in a proximal-to-distal (20 degrees) and posterior-to-anterior direction. A 7 mm diameter drill bit is used at low speed to create the femoral tunnel8 (Figure 2).
-
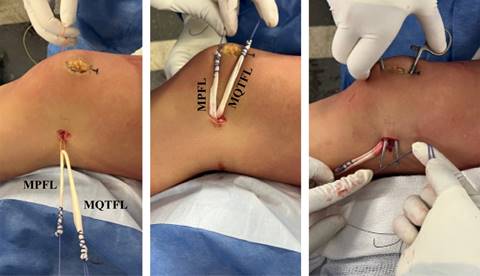
The graft is secured in the femoral tunnel using a 7 mm bioabsorbable interference screw. It is recommended to fix the graft with the proximal end slightly longer than the distal end for proper attachment to the quadriceps tendon (Figure 3).
The appropriate graft fixation is confirmed by longitudinal tension placed upon the graft.
Patellar fixation:
Using a hemostat, both ends of the graft are passed through the plane between the capsule and medial retinaculum. During medial exposure of the patella, care is taken to avoid an arthrotomy by leaving the synovial lining attachment.9,10
A rongeur is used to decorticate the medial patella and the superficial surface.
-
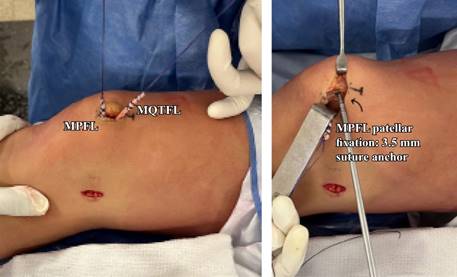
A 3.5 mm suture anchor is placed at the junction of the proximal one-third and distal two-thirds of the palpable osseous patella (Figure 4). A single suture anchor is used instead of an interosseous tunnel or double tunnels to avoid creating a large defect that may increase the risk of patellar fracture.
The patella is then centralized in the trochlea with the knee flexed at 30 to 40 degrees, and the graft length is adjusted and secured in the patella.
An additional #1 Vicryl suture is passed through the patella and allograft tendon for reinforcement.
Knee extension is used to verify that the patella can be manually displaced one quadrant laterally, ensuring correction of instability without excessive pressure on the patellofemoral joint.
Quadriceps tendon fixation:
-
A partial-thickness hole is created 10-15 mm from the superior pole of the patella (Figure 5).
The upper end of the allograft is passed through this hole and self-secured with a FiberWire suture.
Patellar mobility is verified using the Glide test in extension, and excess graft is removed.
The vastus medialis oblique (VMO) is advanced and sutured to the medial edge of the patella using #1 Vicryl sutures.
The area is thoroughly irrigated with saline, and the arthroscope is reintroduced to ensure proper patellar tracking. Following irrigation, a standard closure is performed.
Postoperative protocol:
Postoperatively, the patient is instructed to use crutches and wear a knee immobilizer for two weeks. Weight-bearing is allowed as tolerated with the leg locked in extension until adequate quadriceps control is achieved. Full range of motion exercises are allowed immediately.
Return to sports and high-impact activities is typically authorized after six months, subject to clinical and radiographic assessments, which may vary based on concomitant procedures. This clearance is granted upon achieving a pain-free status, full range of motion, absence of effusion, no objective patellofemoral instability upon examination, near symmetric strength (85% limb symmetry), and excellent dynamic stability, observed as the patient confidently performs sport-specific drills without hesitation.
Standing alignment radiographs are generally conducted at the 1-year follow-up to assess for potential growth disturbances.
Discussion
This article provides insights into the technique employed by the author for reconstructing the MPFC in skeletally immature patients with patellofemoral instability. The surgical approach described utilizes an allograft to reconstruct the medial patellofemoral complex (MPFL and MQTFL), with femoral fixation guided by intraoperative fluoroscopy to avoid injuring the distal femoral physis. The advantages and disadvantages of this procedure are outlined in Table 1.
Table 1: Advantages and disadvantages of the medial patellofemoral complex reconstruction technique with allograft.
| Advantages | Disadvantages |
|---|---|
| Reproduces anatomy | Requires intraoperative fluoroscopy |
| Preserves femoral physis | Availability and cost of allograft |
| Provides static and dynamic stabilization | |
| Greater graft divergence > stability | |
| Allograft < morbidity/surgical time than autograft |
Why choose to reconstruct the MPFC instead of repair? Evidence indicates that the failure rate for repair is three times higher than for reconstruction.11 Repair or imbrications rely on normal tissue, which is often compromised in patients with patellofemoral instability. Therefore, reconstructing the torn anatomy using robust sources such as the semitendinosus, or peroneous longus tendon is preferable, given their superior strength compared to the native MPFC.
Why non-anatomic procedures are not recommended in the pediatric-adolescent population with PFI? Because anatomic reconstruction yields superior outcomes in preventing recurrent instability. Additionally, nonanatomic Insall-type procedures may increase the patellofemoral joint reaction forces beyond normal without fully restoring the effective moment arms. In contrast, anatomic reconstructions seem to restore the effective moment arm without causing excessive joint reaction forces.2
Why choose to reconstruct the entire complex instead of the MPFL? While various techniques and outcomes of traditional medial patellofemoral ligament (MPFL) reconstruction have been described, fewer reports focus on the anatomical reconstruction of the entire medial patellofemoral complex (MPFC) to recreate both fascicles. The decision to opt for the reconstruction of the entire complex, rather than solely the MPFL, is based on several considerations:
Anatomy replication: reconstruction of the MPFC allows for a better reproduction of anatomy.
Function of medial patellar stabilizers: biomechanical studies suggest that while the MPFL is the primary restraint to lateral translation in the early degrees of knee flexion, the MQTFL is responsible for preventing lateral translation in extension.12 Reconstructing both arms of the complex helps control patellar stability in the trochlea more effectively.
Patellar size in pediatric patients: in very young patients, the reduced size of the patella may pose challenges in placing two fixation points on it. MPFC reconstruction adequately addresses this limitation.
Advantages of greater divergence in fixation points: reconstructing both MPFL and MQTFL may allow for greater divergence between fixation points, contributing to increased stability.
What is the rationale for allograft use?
The utilization of allograft in patellar instability surgery offers notable advantages:
While the use of allografts in anterior cruciate ligament (ACL) surgery has shown inferior results and a higher rate of graft failure in the pediatric-adolescent population,15 it is crucial to note that comparisons between ACL and MPFL may be limited due to differences in anatomy and function. The MPFL is a thin, extra articular structure which acts as a checkrein in early knee flexion only in the early stages of knee flexion, with a significantly lower tensile strength compared to the native ACL. Extrapolating ACL reconstruction theory may not be appropriate for MPFL reconstruction.16
Limited series have evaluated outcomes with allografts in skeletally immature patients. Allahabadi and Pandya17 reported the outcomes of 20 patients (24 knees) with an average age of 15.7 years. They underwent reconstruction of the medial patellofemoral ligament (MPFL) using allografts, with a mean follow-up of 5.2 ± 1.7 years (range: 2.2 to 8.1). Only nine knees had open physes, and no clinically significant growth disturbances were observed after surgery. Four knees (16.7%) experienced complications: 3 (12.5%) had recurrent instability, of which two required subsequent surgery, and one suffered a patellar fracture after a fall, necessitating open reduction and internal fixation. Husen et al.18 evaluated 69 patients with an average age of 14.7 ± 1.8 years (range: 8.5-16.9 years). Within the average follow-up period of 37.9 ± 12.1 months (range: 24-85 months post-surgery), 12 patients experienced clinical failures requiring reintervention. Eleven patients had recurrent patellar dislocation, and one patient suffered a transverse patellar fracture requiring surgical fixation. No clinically significant injuries to the distal femoral physes were observed. At the final follow-up, patients had an average Lysholm score (1-100) of 96.5 ± 6.7, a Kujala score (1-100) of 96.5 ± 7.4, and a Tegner activity scale score (1-10) of 4.9 ± 1.3. In total, 57 out of 63 patients (90.5%) who participated in sports before the injury returned to the same or a higher level of competition.
The author of this technical note is currently evaluating 25 patients treated with allograft reconstructions between 2017 and 2022. The average age at the time of surgery was 14 years (range: 3-18 years), and 78% of the patients were female. Average follow-up was 25 months (range: 12-56 months). The median Pedi-IKDC, Kujala, and Lysholm scores were 90.24, 92.44, and 94.19 points, respectively. Only one patient reported an episode of patellofemoral instability, but it did not require surgical revision. No other complications were reported (Table 2).
Table 2: Summarizes key point to avoid complications.
| To avoid damaging the physis, epiphyseal femoral fixation should be performed under fluoroscopic control |
| Consider the undulating shape of the distal femoral physis during femoral fixation |
| Avoid fixation with transverse tunnels in the patella (may cause a fracture) |
| Tension both arms of the graft with the knee flexed at 30-40 degrees |
| After graft fixation, ensure that the patella can move one quadrant laterally with the knee extended |
Conclusion
In summary, this article presents an innovative surgical technique for reconstructing the medial patellofemoral complex in pediatric patients with open physes. The importance of intraoperative fluoroscopy and precise knowledge of distal femoral physis anatomy is emphasized to avoid complications related to physeal injuries. This technique offers a comprehensive approach to addressing patellofemoral instability in skeletally immature patients, with ongoing evaluation necessary to establish its long-term effectiveness and safety.











 nueva página del texto (beta)
nueva página del texto (beta)