Case presentation
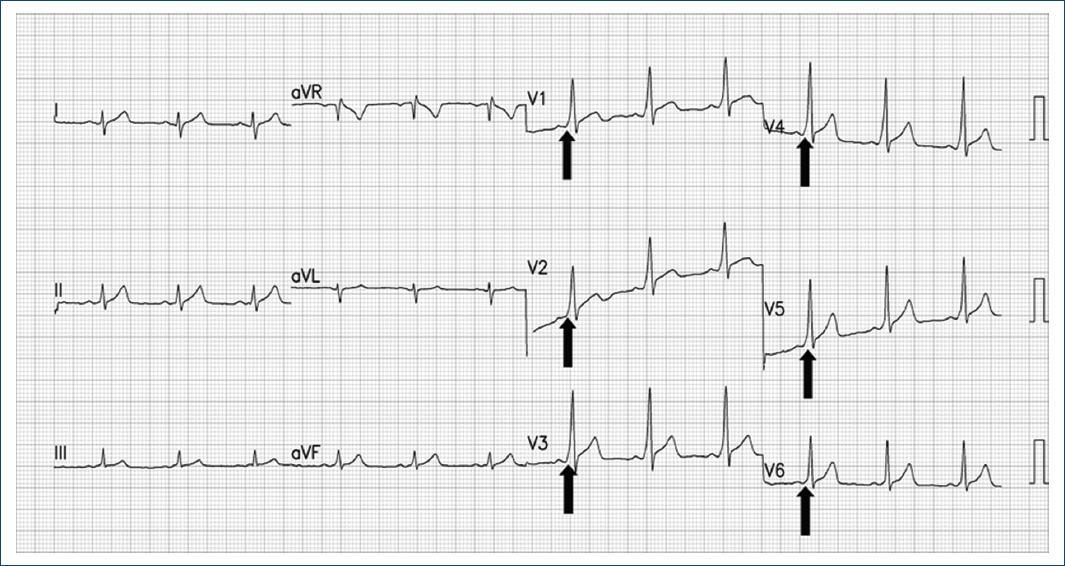
A 36-year-old male from Mexico City, without relevant medical background, attended the emergency department of the Ignacio Chavez National Institute of Cardiology with a sudden onset episode of palpitations and dyspnea triggered by physical exertion. His heart rate was 225bpm, blood pressure 126/76mmHg, and respiratory rate 24/min. On physical evaluation, he was anxious, oriented, hydrated, without jugular venous distention or crackling rales in the lung fields, precordial area with arrhythmic heart sounds, without murmurs, third or fourth heart sound or pericardial rub, abdomen with normoactive peristalsis, not painful at palpation, and without peripheral edema. The initial electrocardiogram (ECG) identified a wide complex, irregular tachycardia, compatible with pre-excited atrial fibrillation (Fig. 1). Treatment with 120-J synchronized cardioversion with a biphasic defibrillator was performed, obtaining an ECG with sinus rhythm and ventricular pre-excitation pattern (Fig. 2). Chest X-rays, routine laboratory tests and echocardiogram were performed, all of which were unremarkable. The patient underwent an electrophysiological study, in which a left lateral accessory pathway was found, achieving successful conventional ablation. The patient was discharged without complications with a follow-up plan in the outpatient clinic.
Discussion
Wolff-Parkinson-White (WPW) syndrome is a ventricular pre-excitation disorder that arises from abnormal cardiac electrical conduction through an accessory pathway (Kent bundle), with a global prevalence of 0.1-0.3%1, a predilection in male gender, and frequently presenting toward the third decade of life2. The most common arrhythmias related with WPW syndrome are narrow QRS complex tachycardias, including atrioventricular (AV) reentry tachycardia, atrial fibrillation, and atrial flutter2. Typically, this syndrome has a benign course, with an incidence of sudden death of 0.5-2 cases per 1000 patients3, in which pre-excited atrial fibrillation that degenerates into ventricular fibrillation the main mechanism identified to date4. The vulnerability to this complication owes to the fact that AV conduction through the accessory pathway lacks the physiologic rate-decreasing property provided by the AV node, therefore, in a concomitant setting of atrial fibrillation, where atrial depolarization can produce rates of 300 beats/min, high ventricular depolarization rates could lead to degeneration into ventricular fibrillation5.
When faced with an irregular RR, wide, QRS complex tachycardia, the clinician should always include pre-excited atrial fibrillation as the first diagnostic possibility6. Considering an accessory pathway has prognostic and therapeutic implications in such symptomatic arrhythmia episodes. The second option could be a ventricular tachycardia; nonetheless, the RR intervals are less irregular than in pre-excited AF6. Making an accurate diagnostic of pre-excited atrial fibrillation promotes an appropriate and timely short-term management that includes ablation of the accessory pathway, and therefore reduction of the risk of sudden cardiovascular death with future episodes2.
The first two were present in our patient, but fortunately, a correct diagnosis and treatment was established7. The first two of were present in our patient, but fortunately, a correct diagnose and treatment was established.
The implementation of appropriate therapeutic interventions during the acute phase of pre-excited atrial fibrillation, and ensuring a definitive ablation strategy is an important issue5. The drugs that are usually used in the treatment symptomatic tachyarrhythmias, such as adenosine, β-blockers, digoxin, calcium antagonists, or amiodarone, are not recommended to treat this specific arrhythmia4. Slowing the AV node conduction might practically render the accessory pathway the only conduction structure, increasing the risk of hemodynamic collapse, ventricular fibrillation, or death4. Synchronized electrical cardioversion is considered the first-line treatment, even though some authors consider the use of ibutilide or procainamide as an alternative pharmacologic approach in hemodynamically stable patients4. Radiofrequency catheter ablation is the cornerstone of definitive treatment, since it offers the possibility of cure with success rates of up to 98.5% with low percentage of complications8. Once patients undergo this intervention, they have the same mortality rate as the general population9.
Unfortunately, to date, physicians still have low skills in recognizing pre-excited atrial fibrillation electrocardiographic pattern, as demonstrated by Koźluk et al.10, in which a hypothetical case like the one related in this paper was assessed by emergency medical physicians, and < 10% of participants made an accurate diagnose10. Enhanced recognition of this complex ECG phenomenon by health providers, is critical to improve the prognosis of patients, and for the reasons explained before, should be a priority in terms of medical education training.











 nueva página del texto (beta)
nueva página del texto (beta)