INTRODUCTION
In December 2019, a new respiratory disease called coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome (SARS-CoV-2) virus appeared in Wuhan, China, and rapidly spread worldwide1. By August 7, 18,902,735 cases of COVID-19 had been diagnosed across the world, and 709,511 patients with COVID-19 had died2. The Chinese Center for Disease Control and Prevention reported 14% and 5% of severe and critical cases, respectively3. Compared with other respiratory viruses, the case fatality rate appears to be lower than SARS and the Middle East respiratory syndrome, but higher than influenza4. Mild forms of COVID-19 represent the vast majority of cases. Since the risk of unfavorable course of this group of patients is usually low, additional evaluation is generally unnecessary, and cases can be managed in the outpatient setting. However, a minority of these patients with mild disease will subsequently present clinical worsening and may require close monitoring, additional testing, and hospital admission5. Tools designed to identify this subgroup of patients are lacking.
Several scores have been proposed to detect patients at risk of clinical deterioration and death in different clinical scenarios. The quick Sequential Organ Failure Assessment (qSOFA) criteria, which consist of respiratory rate (RR), Glasgow Coma Scale, and systolic blood pressure, is a useful tool to predict in-hospital mortality in the general ward6,7. The National Early Warning Score (NEWS) consists of seven parameters and was built to improve the early detection of clinical deterioration of critically ill patients8. NEWS has equivalent or superior accuracy compared with qSOFA to predict clinical deterioration in infected patients outside the intensive care unit (ICU)9,10. During the pandemic, the patient's age was added to the score as a new parameter based on the first observations made in China, which pointed that age is an important prognostic factor in this disease. The CURB-65 was developed for the evaluation of patients with community-acquired pneumonia (CAP) and includes new-onset confusion, urea levels, RR, blood pressure mmHg, and age11. It has been validated to predict 30-day mortality in CAP12. Patients with a low score risk (0-1) can be managed as outpatients since they are considered to have low-risk pneumonia13,14.
To date, there are no validated scores to predict the evolution of mild forms of COVID-19. Early recognition of patients who could be managed in the outpatient setting is important to avoid health-care system saturation. Furthermore, the identification of those patients who will require close monitoring is crucial. The utilization of scores as qSOFA, NEWS2, and CURB-65, which have proven to be useful in different clinical scenarios, appears as an interesting option.
Given that in the initial phase, COVID-19 mainly affects the respiratory system with minor damage to other organs, we hypothesized that an index composed only by respiratory parameters could detect patients at risk of clinical worsening with more precision15. As a consequence, we studied the blood oxygen saturation/RR index (sat/RR). This adaptation of the ROX index applied to patient's breathing room air was chosen because of its simplicity to measure them, and the replicability between different observers. Our study aimed to analyze the accuracy of sat/RR, NEWS2, CURB65, and qSOFA scores to predict the development of supplemental oxygen requirement and prolonged hospital stay in patients with mild COVID-19.
METHODS
We conducted a prospective cohort study in Fernandez Hospital, an academic medical center located in Buenos Aires, Argentina, between April 24 and June 2. During that period, every patient admitted to the hospital was included. The criteria for being admitted to the hospital were the presence of COVID-19 pneumonia and COVID-19 infection with comorbidities and risk factors, with or without pneumonia. SARS-CoV-2 infection was defined as a positive RT-PCR assay in a nasopharyngeal swab. The mildness of the disease was defined at admission, based on pulse oximetry greater than 92% and a RR lower than 30 breaths per minute with no supplemental oxygen requirement. There were no exclusion criteria.
The diagnosis of pneumonia was defined as the presence of clinical signs and symptoms compatible with lower airway infection (cough, dyspnea, and fever) with image confirmation. The techniques used included chest X-ray, chest ultrasound, and/or chest CT scan.
Data were collected in a structured form during the patients' admission, including demographic and epidemiological information, comorbidities (diabetes, obesity, hypertension, congestive heart failure, coronary disease, HIV infection, chronic kidney disease, alcohol abuse, smoking history, chronic obstructive pulmonary disease, asthma, and tuberculosis), signs and symptoms at disease onset, vital signs (blood pressure, heart and RR, temperature, and blood oxygen saturation by pulse oximetry), qSOFA, CURB65, NEWS2, sat/RR scores, blood test, and chest image. A member of the data management team, reviewed by a second member of the same team, loaded data submitted by physicians on the paper form to a digital database.
Patients were followed until hospital discharge, ICU admission, or death. The primary outcome was the accuracy of sat/RR, NEWS2, CURB65, and qSOFA to predict the development of supplemental oxygen requirement. The secondary outcome was the accuracy of these scores to predict prolonged hospitalization (defined as greater than 10 days since admission).
Statistical analysis
Comparisons between groups were made with a t-test or Mann–Whitney test, depending on the presence or not of normal distribution. When differences between groups were statistically significant, the discriminatory capacity of the score for that outcome was analyzed with the receiver operating curve (ROC). The area under the curve (AUC) and their 95% CI were informed. A cutoff point was defined according to the values of the ROC curve, and univariate and multivariate logistic regression was performed. ORs and their 95% CI were reported. We analyzed the correlation between Sat/RR index and C-reactive protein (CRP) at admission using Spearman's method. The manuscript was written according to the STROBE initiative for the communication of observational studies. The Institutional Ethics Committee of our hospital reviewed and approved the study.
RESULTS
We included 271 patients. The general characteristics of the cohort are shown in Table 1. The mean (SD) of age was 42 (16) years; 46.83% of patients were female, and 48% had the diagnosis of pneumonia at admission. Regarding comorbidities, 43.25% had at least one condition, with obesity as the most frequent (18.7%), followed by hypertension (12.7%) and diabetes (10.7%). The median (IQR) since the beginning of symptoms was 4 days (2-7). The most prevalent symptom was cough (57.14%), followed by fever (55.16%) and headache (53.7%). As the cohort included only patients with mild forms of COVID-19, no patients had low oxygen saturation at admission. We analyzed the behavior of four severity scores: sat/RR index, NEWS2, CURB65, and qSOFA. At admission, the mean (SD) of the sat/RR index was 5.19 (1.05); the median (IQR) of NEWS2 score was 2 (1-4); the median (IQR) of CURB65 was 1 (1-2), and the median (IQR) of the qSOFA was 0 (0-1). In their evolution, 30 patients (11.07%) received supplemental oxygen, 9 (3.57%) required ICU admission, and 107 (38%) required prolonged hospitalization (longer than 10 days). No patient died during the follow-up. The median (IQR) days of hospitalization was 9 (5-11).
Table 1 General characteristics of the study population admitted to Hospital Fernández between April 24 and June 2
| Variable | n = 271 | Respiratory failure (n = 30) | Prolonged length of stay (n = 107) |
|---|---|---|---|
| Sex, female n (%) | 128 (47.23%) | 15 (50%) | 49 (45.79%) |
| Age, mean (SD) | 43.18 (16.9) | 54.4 (12.5) | 49.0 (16.9) |
| Comorbidities | |||
| At least 1 comorbidity, n (%) | 120 (44.25%) | 19 (63.33%) | 59 (55.14%) |
| Diabetes, n (%) | 33 (12.18%) | 8 (38.09%) | 21 (19.63%) |
| Obesity, n (%) | 55 (20.37%) | 7 (33.33%) | 27 (25.23%) |
| HIV, n (%) | 3 (1,19%) | 1 (4.76%) | 3 (2.8%) |
| Chronic kidney disease, n (%) | 4 (1.48%) | 1 (3.33%) | 4 (3.74%) |
| Asthma, n (%) | 15 (5,95%) | 0 | 6 (5.61%) |
| Arterial hypertension, n (%) | 39 (14.39%) | 8 (26.67%) | 26 (24.30%) |
| COPD, n (%) | 1 (0,37%) | 0 | 1 (0.93%) |
| Smoking history, n (%) | 28 (10.33%) | 5 (16.67%) | 10 (9.35%) |
| Hepatic disease, n (%) | 2 (0.74%) | 1 (3.33%) | 2 (1.87%) |
| Symptoms | |||
| Cough, n (%) | 158 (58.30%) | 21 (70%) | 66 (61.68%) |
| Fever, n (%) | 154 (56.83%) | 22 (73.33) | 67 (62.62%) |
| Headache, n (%) | 143 (52,77%) | 14 (46.67%) | 46 (42.99%) |
| Asthenia n (%) | 116 (42.80%) | 11 (36.67%) | 43 (40.19%) |
| Anosmia/dysgeusia, n (%) | 89 (33.84%) | 7 (23.33%) | 27 (26.21%) |
| Myalgia, n (%) | 89 (32.84%) | 11 (36.67%) | 30 (28.04%) |
| Sore throat, n (%) | 86 (31.73%) | 8 (26.67%) | 27 (25.23%) |
| Dyspnea, n (%) | 75 (27.68%) | 16 (53.33%) | 41 (38.32%) |
| Diarrhea, n (%) | 41 (15.13%) | 5 (16.67%) | 17 (15.89%) |
| Vomits, n (%) | 15 (5,54%) | 0 | 6 (5.61%) |
| Variable | n = 271 | Respiratory failure (n = 30) | Prolonged length of stay (n = 107) |
| Physical exam | |||
| Systolic blood pressure, mean (SD) | 120 (17.46) | 123.4 (13.7) | 123.0 (13.7) |
| Diastolic blood pressure, mean (SD) | 75.13 (10.28) | 75.16 (9.1) | 75.67 (10.0) |
| Heart rate, mean (DS) | 90.33 (13.85) | 97 (14.8) | 92.2 (14.9) |
| Respiratory rate, mean (SD) | 19.41 (3.75) | 22.3 (4.2) | 20.6 (3.7) |
| Temperature, mean (SD) | 36,7 (0,95) | 37.3 (1.2) | 36.9 (1.0) |
| Blood oxygen saturation, mean (SD) | 96.8 (1.38) | 96 (1.4) | 96.2 (1.4) |
| Biomarkers | |||
| CRP on admission, median (IQR) | 2,6 (0.71-5.7) | 7.9 (4.7-14.1) | 4.3 (2.3-8.38) |
| LDH on admission, median (IQR) | 238.5 (195-294) | 333.0 (251.5-410.5) | 254.5 (206-335) |
| Ferritin at 4th day, median (IQR) | 380 (138-687) | 698.8 (375.0-803.0) | 460.7 (218-919) |
| D-dimer at 4th day, median (IQR) | 251.5 (224-354) | 368.0 (265.0-642.0) | 414.9 (105-1900) |
| Absolute lymphocytes count, (SD) | 1606 (781.1) | 1360.7 (716.8) | 1527.3 (692.0) |
| Clinical evolution | |||
| Supplemental oxygen requirement (%) | 30 (11.07) | ||
| Assisted mechanical ventilation, n (%) | 4 (1.75%) | ||
| Extended hospitalization, n (%) | 107 (39.48%) | ||
| Hospital length (days), median (IQR) | 9 (5-11) | ||
| Death, n (%) | 0 | ||
COPD: Chronic Obstructive Pulmonary Disease; CRP: C-reactive protein; HIV: Human Immunodeficiency Virus; LDH: lactate dehydrogenase.
We compared the values of these four scores between the groups of patients that required supplemental oxygen with those who did not. The first group had significantly higher values of NEWS2 score and qSOFA score, and significantly lower values of Sat/RR index (Table 2). When we compared patients that required a prolonged hospitalization from those who did not, the first group had significantly higher values of NEWS2 score and significantly lower values of Sat/RR index (Table 3).
Table 2 Comparison of scores values regarding the outcome supplemental oxygen requirement
| Variable | No supplemental oxygen requirement | Supplemental oxygen requirement | p-value |
|---|---|---|---|
| NEWS2m, median (iqr) | 2 (1-4) | 5 (2.5-5.5) | < 0.0001 |
| CURB65, median (iqr) | 1 (1-1) | 1 (1-2) | 0.7324 |
| qSOFA, median (iqr) | 0 (0-1) | 1 (0-1) | 0.0004 |
| Sat/RR, mean (SD) | 5.27 (1.03) | 4.51 (1.09) | 0.0001 |
Table 3 Comparison of scores values regarding the outcome prolonged hospitalization
| Variable | No prolonged hospital stay | Prolonged hospital stay | p-value |
|---|---|---|---|
| NEWS2m, median (iqr) | 2 (1-3) | 3 (2-4) | 0.0002 |
| CURB65, median (iqr) | 1 (1-1) | 1 (1-2) | 0.0418 |
| qSOFA, median (iqr) | 0 (0-1) | 0 (0-1) | 0.0921 |
| Sat/RR, mean (SD) | 5.42 (1.09) | 4.83 (0.88) | <0.0001 |
We analyzed the ability to discriminate the occurrence of both outcomes with the ROC curve in those scores that showed significantly different values between groups in the above-mentioned comparison. The AUC of the Sat/RR index to discriminate the requirement of supplemental oxygen in the evolution was 0.72 (95%CI 0.61-0.84) (Fig. 1). A cutoff point of 4.5 showed a sensitivity of 79.2% and a specificity of 57.1%. The same cutoff point showed an OR of 4.61 (95% CI 2.1-10.13). After adjusting to age, obesity, and diabetes, we obtained an OR of 4.77 (95% CI 2.04-11.15). We analyzed the ROC curve of the NEWS2 and the qSOFA score for the same outcome. The AUCs were 0.75 (95% CI 0.65-0.85) and 0.66 (95% CI 0.57-0.76), respectively.
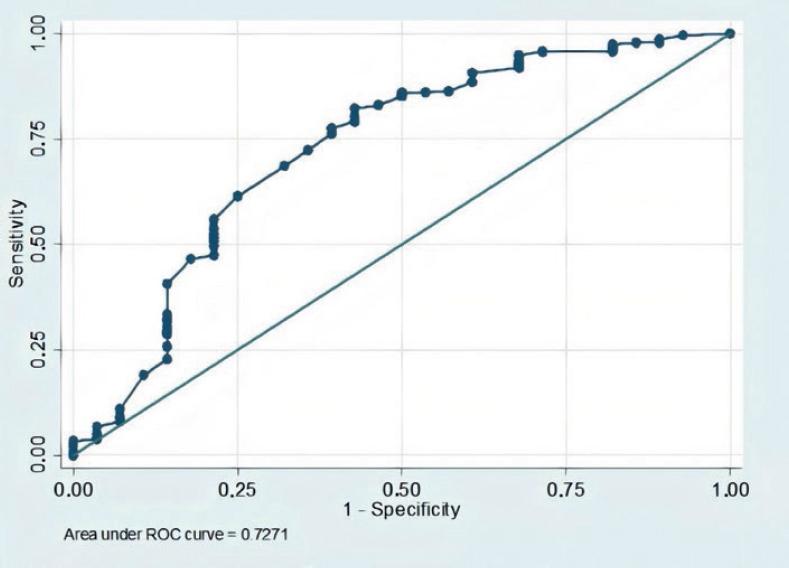
Figure 1 Blood oxygen saturation/respiratory rate index ROC curve for the outcome supplemental oxygen requirement.
The ability of the Sat/RR index to discriminate the requirement of prolonged hospitalization showed an AUC of 0.67 (95% CI 0.60-0.73) (Fig. 2). A cutoff point of 4.5 showed a sensitivity of 82.5% and a specificity of 35.5%. The same cutoff point showed an OR of 2.46 (95% CI 1.4-4.28). After adjusting for age, obesity, and diabetes, we obtained an OR of 2.22 (95% CI 1.23-4.01). We analyzed the ROC curve of the NEWS2 score for the same outcome. The AUC was 0.63 (95% CI 0.56-0.70).
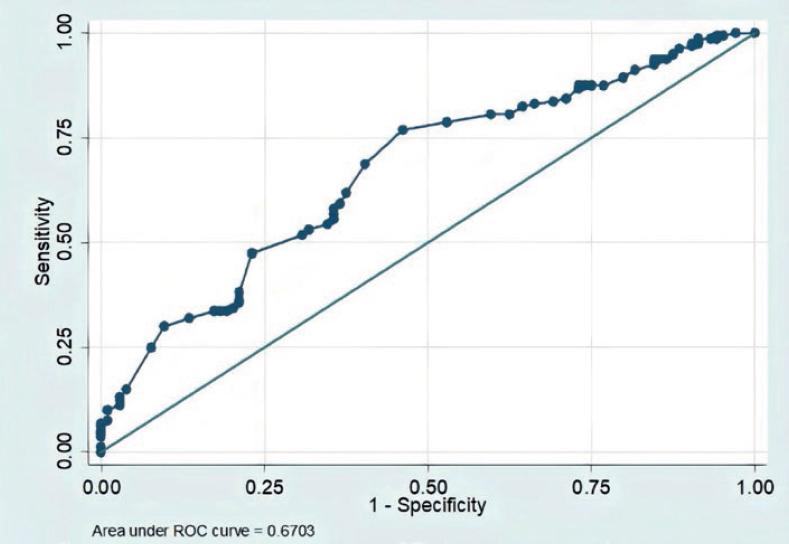
Figure 2 Blood oxygen saturation/respiratory rate index ROC curve for the outcome prolonged hospitalization.
Those patients with prolonged length of stay presented a mean (SD) of 5.63 days (2.77) since the onset of symptoms at hospital admission compared with a mean (SD) of 4.4 (2.78) from those who did not, with a significant p-value (p = 0.007). Likewise, patients who developed supplemental oxygen requirements had a mean (SD) of 6.68 (2.98) days from the onset of the symptoms at admission against 4.71 (2.73) from those who did not, with a significant relationship (p = 0.009).
Regarding the correlation of Sat/RR with RCP at admission, we found an r-value of -0.44 (p < 0.001).
DISCUSSION
Our study shows that sat/RR index and NEWS2 are useful tools to predict the unfavorable evolution of patients with mild forms of COVID-19. We also found a correlation between days since the onset of symptoms at admission and outcomes.
In our current situation, rapid and accurate identification of patients at risk of having an unfavorable evolution is important since it could help to provide close monitoring and early medical attention to those patients who require it, and manage the cases with a good prognosis in the outpatient setting.
Many studies have proven the prognostic value of either epidemiological or biological factors. In regard to epidemiology, age and some comorbidities as arterial hypertension, diabetes, obesity, malignancy, and pulmonary disease have shown to be associated with poor outcomes16-18. Similarly, the alteration of some biological markers such as the elevation of CRP, interleukin-6, lactate dehydrogenase, and D-dimer, or the presence of lymphocytopenia or thrombocytopenia has shown a correlation with an unfavorable evolution19-21. Likewise, we found a good correlation between Sat/RR index and RCP levels at admission, showing that the index varies in relationship with the degree of inflammation.
Although the prognostic value of all the previously mentioned variables has been well documented, information about them is scarce in mild COVID-19 cases. Cases that initially present as mild COVID-19 represent a clinical scenario that has received less attention from researchers than the severe forms of the disease. As a consequence, our ability to predict the clinical course of these patients is limited.
The clinical spectrum of mild COVID-19 has a wide range of symptoms. An observational study carried out in Europe that included 1420 patients with mild-moderate COVID-19 showed that the most prevalent symptoms were headache, anosmia, nasal obstruction, cough, myalgia, rhinorrhea, dysgeusia, and sore throat. Most of these patients do not require hospital admission since they can be managed at their homes. According to WHO, as long as the case is mild or moderate without risk factors for severe disease, the household is suitable for isolation. If monitoring for signs of deterioration is feasible, home care could be carried out22. However, the utilization of a simple prognostic score built with variables obtained in the physical exam could be very useful to complete the prognostic information provided by the previously mentioned demographic and clinical data. This background supported our intention to study the qSOFA, CURB65, and NEWS2 scores in mild COVID-19. Furthermore, it highlights the importance of the identification of SatO2/RR index as a simple prognostic tool. We included in that index only variables that evaluate the respiratory system because it is the mainly affected system in the initial phase of the disease. On the other side, systemic compromise and organ failure usually develops in patients with severe and advanced disease, generally admitted in ICU1. The selection of these variables is supported by studies that show that RR and blood oxygen saturation (SatO2) are more frequently affected than other vital signs23,24. Moreover, there are reported cases in which patients show no change in physical exam parameters except for an increased RR and low blood oxygen saturation. This clinical picture has been called silent pneumonia or silent hypoxemia25. As the case report mentions, the patients' vital signs were all normal except those which this index takes into account.
When we reviewed the available literature, we found an antecedent to the SatO2/RR index, the ROX index26,27. That index is composed of three variables: SatO2, RR, and the fraction of inspired oxygen (FiO2). It is used in patients receiving oxygen by high-flow nasal cannula as a tool to predict its failure and determine if early intubation is needed. The sat/RR index is simpler but can be applied only in patients without supplemental oxygen, as occurs in mild COVID-19.
Our study has points that stand out. First, it focuses on patients with mild COVID-19, a frequent clinical scenario in which there are still many gaps to reveal. Second, a useful and simple tool to evaluate these patients is proposed. Third, the study has a prospective cohort design, minimizing the possibility of selection bias. Fourth, the use of a jointed index may detect patients at risk who have both RR and SaO2 in normal ranges, and otherwise, would not be correctly assessed. However, it is not exempted from limitations. First, the fact that important outcomes such as death or ICU admission were scarce made their evaluation difficult. Second, even though the patients were followed up to hospital discharge and no patient was lost, a subsequent follow-up was not done, making it impossible to know whether readmission occurred. Third, numerous factors influence pulse oximetry results such as altitude, age, and obesity among others, deeming it not accurate in such scenarios. Finally, this study was conducted in a single center, which attempts against its external validity.
We consider that the sat/RR index has a good capacity to discriminate those patients at risk of presenting clinical worsening from those who will not. That capacity is similar to one of the most used scores (NEWS2) with the advantage of being simpler. As a consequence, we believe this index could be a meaningful contribution to the management of mild COVID-19 patients. Nevertheless, these findings should be confirmed with new studies, ideally with a multicenter design.











 nueva página del texto (beta)
nueva página del texto (beta)


