Brief communications
Evaluation of Anti-Citrullinated and Anti-Carbamylated Antibodies in Mexicans with Rheumatoid Arthritis and At-Risk Individuals
-
Publication dates-
December 21, 2024
, 2024
- Article in PDF
- Article in XML
- Automatic translation
- Send this article by e-mail
- Share this article +
ABSTRACT
Background:
Rheumatoid arthritis (RA) diagnosis is a challenge in the initial phases of the disease when clinical symptoms are only starting to develop. Early diagnosis and treatment can promote long-term remission, reduce disability, and improve cardiovascular outcomes. Autoantibodies can help in the diagnosis and identification of RA patients in the early phases of the disease, but scarce information has been reported for the Mexican population.
Objective:
To study anti-citrullinated peptide antibodies (anti-CCP) and anti-carbamylated protein antibodies (anti-CarP) in Mexican patients with RA and individuals at high risk of developing the disease.
Methods:
Serum samples from long-standing and early RA patients, first-degree relatives (FstD) of RA patients, and healthy individuals were analyzed for anti-CCP and anti-CarP using enzyme-linked immunosorbent assay.
Results:
Anti-CCP and anti-CarP levels were higher in the RA groups than in the FstD and healthy groups. The odds ratio (OR) for anti-CCP for RA groups was 29.7 (95% confidence interval [CI] 14.2-61.9), significantly higher than the OR for anti-CarP 11.07 (95% CI 5.4-22.8). The sensitivity of anti-CCP was 85% (95% CI 76-93) higher than for anti-CarP (42.1%, 95% CI 31-54). The specificity of anti-CarP was 93.8% (95% CI 90-97) and the specificity of anti-CCP was 83.4% (95% CI 78-88). Using both tests in parallel increased sensitivity to 91%, while a sequential approach increased sensitivity to 98%.
Conclusion:
Anti-CCP outperformed anti-CarP in Mexican RA patients, demonstrating greater sensitivity, while anti-CarP showed higher specificity. Combining these tests, either simultaneously or sequentially, could enhance diagnostic accuracy. (Rev Invest Clin. 2024;76(6):243-52)
Keywords::
Anti-citrullinated peptide antibodies, Anti-carbamylated protein antibody, Diagnostic value, Mexican population, Rheumatoid arthritis
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory disease that affects joints and several systems and organs. Its etiology is multifactorial involving genetic and environmental factors, with smoking being a prominent contributor1. Based on symptom duration RA can be clinically classified in early RA (if symptoms are present in < 6 months), and established RA (if symptoms are present for more than 6 months)2,3 In this clinical classification, laboratory tests are used to improve the RA diagnosis.
-
1Determining in which pre-arthritis stage HLA-shared epitope alleles and smoking exert their effect on the development of rheumatoid arthritis.Ann Rheum Dis., 2022
-
2Diagnosis and classification of rheumatoid arthritis.J Autoimmun., 2014
-
3Rheumatoid arthritis. In: StatPearls., 2022
Before 2009 the rheumatoid factor (RF) test was the main laboratory test used as an aid in RA diagnosis. However, RF is present also in other rheumatic diseases and in healthy individuals4 limiting it as a discriminatory test. In 2010 the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) introduced modifications to classification criteria for the diagnosis of RA. The anti-citrullinated peptide antibody (anti-CCP) laboratory test was included in these new criteria5. Despite its inclusion, studies have reported variability in the performance of commercially available anti-CCP tests across different populations and studies6. For example, in a meta-analysis of 86 studies, the pooled sensitivity was 67% and the specificity was 95%7, whereas another systematic review including 151 studies reported a sensitivity of 57% and specificity of 96%8. In both analyses, the anti-CCP test had greater specificity than RF for early and established RA7,8. In Mexico, in a study that compared 145 patients with RA with healthy controls, the second-generation anti-CCP test had a sensitivity of 66% and specificity of 94%9. When used together RF and anti-CCP tests have limited diagnostic accuracy and are only able to detect 50-70% of RA cases.
-
4IgG rheumatoid factor.Relationship to seropositive rheumatoid arthritis and absence in seronegative disorders. Arthritis Rheum., 1979
-
52010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative.Arthritis Rheum., 2010
-
6Standardisation of ACPA tests: evaluation of a new candidate reference preparation.Ann Rheumat Dis., 2022
-
7Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis.Ann Intern Med., 2007
-
8Systematic review: accuracy of anti-citrullinated peptide antibodies for diagnosing rheumatoid arthritis.Ann Intern Med., 2010
-
7Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis.Ann Intern Med., 2007
-
8Systematic review: accuracy of anti-citrullinated peptide antibodies for diagnosing rheumatoid arthritis.Ann Intern Med., 2010
-
9Comparison of two assays to determine anti-citrullinated peptide antibodies in rheumatoid arthritis in relation to other chronic inflammatory rheumatic diseases: assaying anti-modified citrullinated vimentin antibodies adds value to second-generation anti-citrullinated cyclic peptides testing.Biomed Res Int., 2014
On the other hand, in 2011 the anti-carbamylated protein antibody (anti-CarP) was proposed as a novel biomarker for RA diagnosis10. Although anti-CarP and anti-CCP coexist in RA, they are distinct antibodies11. Like anti-CCP, anti-CarP is produced in response to post-translationally modified proteins. While citrullination involves the conversion of arginine to citrulline for anti-CCP formation, carbamylation involves the conversion of lysine to homocitrulline, which alters protein folding and contributes to anti-CarP formation11-13. These biochemical similarities have been associated with cross-reactivity even in subjects without RA14,15. Despite this fact, anti-CarP antibodies have shown potential to aid in RA diagnosis. Indeed these antibodies were measured in subjects with arthralgia who were followed over time, and there was an association with the development of RA16. Studies performed in Swedish patients indicate a specificity of 97% and sensitivity of 42% for the anti-CarP test17.
-
10Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage.Proc Natl Acad Sci USA., 2011
-
11Clinical and etiological meaning of anti-carbamylated protein antibodies in rheumatoid arthritis.Immunol Med., 2018
-
11Clinical and etiological meaning of anti-carbamylated protein antibodies in rheumatoid arthritis.Immunol Med., 2018
-
13Protein carbamylation links inflammation, smoking, uremia and atherogenesis.Nat Med., 2007
-
14Cross-reactivity of anti-modified protein antibodies is also present in predisease and individuals without rheumatoid arthritis.Ann Rheum Dis., 2022
-
15The value of anti-CarP and anti-PAD4 as markers of rheumatoid arthritis in ACPA/RF negative rheumatoid arthritis patients.Ther Adv Musculoskelet Dis., 2021
-
16Anti-carbamylated protein antibodies are present in arthralgia patients and predict the development of rheumatoid arthritis.Arthritis Rheum., 2013
-
17Anti-carbamylated protein antibodies in the pre-symptomatic phase of rheumatoid arthritis, their relationship with multiple anti-citrulline peptide antibodies and association with radiological damage.Arthritis Res Ther., 2015
To our knowledge, very few studies on anti-CarP in a Mexican population have been reported, and neither has an evaluation of the use of both anti-CCP and anti-CarP for the identification of early and long-standing RA (lsRA). The aim of the present study was to evaluate anti-CCP and anti-CarP antibodies in Mexican patients with RA and individuals at high risk to develop the disease.
PATIENTS AND METHODS
Study design and sample size calculation
This cross-sectional study included four independent sample groups (total n = 287): long-standing RA patients (lsRA), n = 58; early RA (eRA), n = 18; first-degree relatives of RA patients (FstD), n = 157; and healthy individuals, n = 54. Participants were recruited at a private rheumatology research center in Guadalajara, Mexico, and a secondary-care, outpatient rheumatology clinic in Zacatecas, Mexico, between July 2013 and October 2014. Sample size power was calculated post-hoc using G × Power18 with parameter values of a medium effect size of 0.25 and ∞ value of 0.05, considering an analysis of variance statistics to be applied to the data obtained from the four groups of study. The estimated power analysis (1-β) was 95%, showing that the collected sample size of 287 was appropriate.
-
18Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses.Behav Res Methods., 2009
Studied subjects
Adult-onset RA patients were classified according to the ACR/EULAR5. In our study, RA patients were labeled as lsRA (disease duration longer than 2 years), early RA (eRA, disease duration of < 1 year). Sociodemographic data and RF titers for all subjects were obtained from clinical charts. The recruitment and inclusion process for first-degree relatives (FstD) has been described previously19. In brief, RA patients were asked to invite FstD not having RA or any other rheumatic disease to participate in the study. These relatives underwent a clinical history, and joint assessment performed by two board-certified rheumatologists, to determine the absence of any current or past relevant diseases including any rheumatic diseases. The group labeled as apparently healthy controls was recruited at the Zacatecas outpatient clinic.
-
52010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative.Arthritis Rheum., 2010
-
19Autoantibodies in prediction of the development of rheumatoid arthritis among healthy relatives of patients with the disease.Arthritis Rheumatol., 2015
Ethics
All participants provided written informed consent to participation in the study, in compliance with the requirements of the National Scientific and Ethics Committee at "Instituto Mexicano del Seguro Social" which is also a COFEPRIS-approved committee. Register number R2013-785-009. All procedures were carried out according to current national and international best practices and guidelines in ethics and research involving human subjects.
Collection and processing of serum samples
Two peripheral venous blood samples were collected from each patient in Vacutainer tubes free of anticoagulant (Venous blood collection tube with Red BD Hemogard™, BD Vacutainer®, New Jersey, USA). Each tube of fresh blood was incubated for 30 min at room temperature (RT) and then centrifuged for 5 min at 1600 g to separate the serum, which was aliquoted into three 1.5-mL Eppendorf tubes (Eppendorf Safe-Lock Tubes™, Eppendorf, Hamburg, DE). Serum samples were stored at −20°C until use.
Detection of anti-CCP antibodies by enzyme-linked immunosorbent assays
The enzyme-linked immunosorbent assay (ELISA) kit approved by ACR/EULAR (Immunoscan CCplus® RA-96Plus, Eurodiagnostica, Sweden), was used in accordance with the manufacturer´s instructions to detect anti-CCP. All reagents were used at RT. One hundred μL of 1/50 diluted serum samples were added to each well plate including the standard dilutions provided in the kit. The plates were then washed 3 times with the washing buffer supplied in the kit, and then 100 μL of the conjugate solution was added to each well. The plates were then incubated for 30 min at RT and washed again as described above. A substrate solution consisting of 100 μL of 3,3’5,5’ tetramethyl-benzidine was then added to each well and the plates were incubated in the dark for 30 min at RT before the addition of 100 μL of the "stop solution" provided in the kit. The plates were read at 450 nm in a Multiskan Ascent 96/384 plate reader (MTX Systems, USA). Linear regression analysis was performed using optical density (OD) values derived from standard curve points to determine the concentration of each sample based on its OD value minus the value of the blank, in accordance with the manufacturer´s instructions. Values > 25 U/mL were considered positive.
Standardization and evaluation of anti-CarP positivity
The protocol used for the carbamylation of fetal bovine serum (FBS) was previously described by Shi et al.10 A total of 4 mg/mL of FBS (Bodinco, Alkmaar, NL, USA) was used to prepare the carbamylated FBS. FBS was diluted in H2O and mixed with 1 M solution of potassium cyanate (Sigma-Aldrich, St. Louis, MO, USA) at a final concentration of 4 mg/mL for 12 h at 37°C, then the preparation was dialyzed in H2O. Finally, the presence of carbamylated residues in the preparation was assessed through mass spectrometry. The carbamylated FBS control was kindly provided by Dr. Leendert A. Trouw.
-
10Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage.Proc Natl Acad Sci USA., 2011
An ELISA buffer kit (Peprotech, USA) was used to standardize the indirect semi-quantitative ELISA technique for the detection of anti-CarP in the samples. Modifications to the protocol described by Shi et al.10 were made as follows: High-affinity 96-well plates (EIA/RIA, Costar®, Corning Inc., NY, USA) were coated for 14-16 h at 4°C using 50 μL of FCS per well and carbamylated FCS at 5 μg/mL diluted in filter-sterilized 0.1 M pH 9.6 carbonate buffer. Three washes were then performed with phosphate-buffered saline (PBS)-1% Tween-20 buffer, then the plates were blocked for 6 h with 100 μL/well of PBS-1% bovine serum albumin buffer at 4°C, followed by three washes with the same solution. Serum samples diluted 1/100 in PBS-Tween-20 were then added (50 μL/well, plated in duplicate) and the plates were incubated for 14-16 h at 4°C. A standard curve was derived using several dilutions (1/100, 1/250, 1/350, 1/400, 1/450, 1/550, 1/600, and 1/650) of a pool of sera (previously identified as having high reactivity to carbamylated FCS was used for validation purposes). After a 3-h incubation, the plates were washed 3 times as described above, then 50 μL/well of rabbit anti-human H and L horseradish peroxidase secondary antibody (Abcam®, USA) diluted 1/20,000 in PBS was added and the plates and incubated for 3.5 h at 4°C. After three washes the plates were incubated for 30 min with 2,2´-azine-di (3-ethyl-benzothiazolin) sulfonate. OD values for each sample were obtained at 450 nm using a Multiskan Ascent 96/384 reader (MTX Systems, USA). The antibody concentrations in the samples were calculated by comparing the OD values derived from the samples with the standard curve. An anti-CarP positivity cut-off point of 256 AU/mL was utilized as previously described by Brink et al.17 in addition to the mean plus two standard deviations of the healthy controls (cut-off = 293.2).
-
10Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage.Proc Natl Acad Sci USA., 2011
-
17Anti-carbamylated protein antibodies in the pre-symptomatic phase of rheumatoid arthritis, their relationship with multiple anti-citrulline peptide antibodies and association with radiological damage.Arthritis Res Ther., 2015
Statistical analysis
Statistical analyses were conducted using the R program20 and the FSA, epiR, and fsmb packages, a p < 0.01 was considered statistically significant in all tests. Because most of the data were not normally distributed as determined through the Shapiro–Wilk and Kolmogorov tests, differences between the groups were evaluated through the non-parametric Kruskal–Wallis test. When significant differences between the groups were observed, each comparison was assessed through Dunn´s multiple comparisons post-hoc test. Differences in proportions between the groups were assessed through the X2 test with Yates’ continuity correction. Based on the possibility that an underlying immune mechanism could be responsible for autoantibody production, we performed correlational analysis with the non-parametric Spearman correlation test and calculated agreement according to the kappa statistic. The kappa test agreement values were interpreted as follows: 0.00-0.20, none; 0.21-0.39, minimal; 0.48-0.59, weak; 0.60-0.79, moderate; 0.80-0.90, strong; > 0.90 almost perfect21. In addition, the Bland-Altman analysis was performed to check the agreement of the two tests with the "bland.altman.plot" function from the BlandAltmanLeh R-package. In this analysis anti-CCP and anti-CarP values were log-transformed to show the differences (anti-CCP-anti-CarP) based on the mean of the two tests ([anti-CCP + anti-CarP]/2) to be plotted in a graphical manner22. In the previous and subsequent statistical analyses, the RF variable was excluded due to a lack of complete data. Association´s indicative of the presence of disease was assessed through the crude odds ratio (OR). The Mantel-Haenszel OR was calculated to control for confounding variables grouped by strata. For age strata Haldane-Anscombe correction23,24 was applied by adding 0.5 to cells with zeroes. Diagnostic importance values were calculated based on sensitivity and specificity, which were also used to determine parallel and serial test scenarios, assuming independence between anti-CCP and anti-CarP tests25 as follows:
-
20R: a language and environment for statistical computing, 2016
-
21Interrater reliability: the kappa statistic.Biochem Med, 2012
-
22Understanding bland Altman analysis.Biochem Med., 2015
-
23The estimation and significance of the logarithm of a ratio of frequencies.Ann Hum Genet., 1956
-
24On estimating binomial response relations.Biometrika., 1956
-
25Veterinary Epidemiology, 2005
–. Serial sensitivity = anti-CCP sensitivity × anti-CarP sensitivity
–. Parallel sensitivity = 1-(1-anti-CCP sensitivity) × (1-anti-CarP sensitivity)
–. Serial specificity = 1-(1-anti-CCP specificity) × (1-anti-CarP specificity)
–. Parallel specificity = anti-CCP specificity × anti-CarP specificity
RESULTS
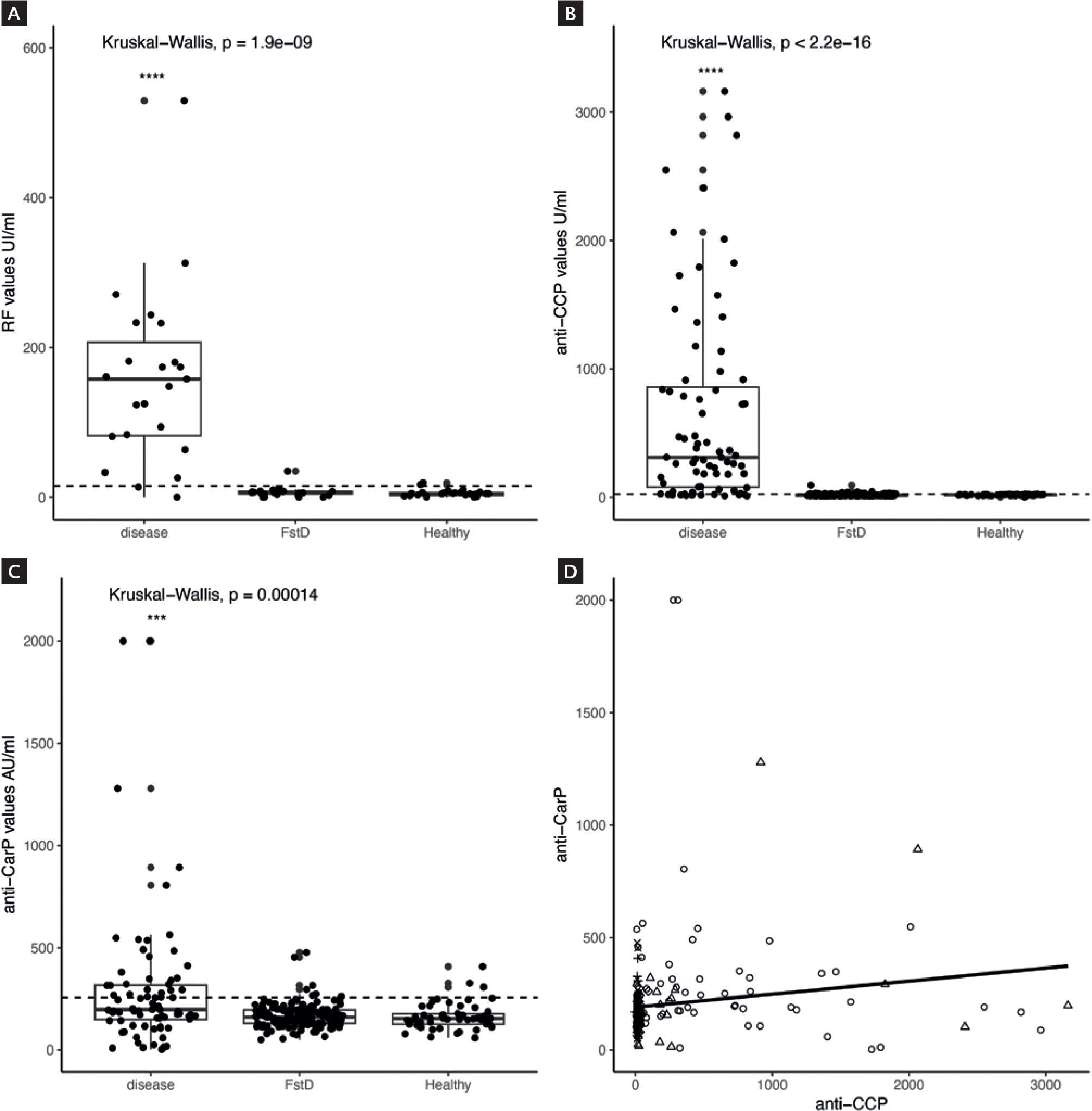
Anti-CCP and anti-CarP tests are independent
The baseline characteristics of the groups are summarized in Table 1. There were statistically significant differences (p < 0.01) in age and gender between the groups, and these potential confounding variables were considered in the subsequent statistical analyses. RF, anti-CCP, and anti-CarP levels were higher in the combined RA group (eRA plus RA) than in the healthy control group and the FstD group (p < 0.01; Fig. 1A-C). In Dunn´s post-hoc testing, there were no significant differences between the FstD group and the healthy control group (p > 0.01; Fig. 1A-C). In Spearman correlation analysis the association between anti-CCP and anti-CarP was weak (rs = 0.17; Fig. 1D). The lack of correlation prompted us to assess whether there was concordance between the tests (Table 2). A total of 32 individuals were both anti-CCP-positive and anti-CarP-positive (double positive), and 174 were both anti-CCP-negative and anti-CarP-negative (double negative). The agreement for the two tests was 0.72 and the kappa statistic was 0.28, indicating minimal agreement. This result was further confirmed through the Bland-Altman plot which showed measures scattered outside the confidence limits (Fig. 2). Thus, correlation analysis, kappa and Bland-Altman results indicated that anti-CCP and anti-CarP tests are independent diagnostic tools.
Table 1
Baseline characteristics of the formed groups
Baseline characteristics of the formed groups
| Variable | Arthritis |
FstD |
Healthy |
p |
|---|---|---|---|---|
| Female (%) | 66 (86.8) | 110 (70.5) | 46 (85.1) | p < 0.001 |
| Age (range) | 50.5 (24-78) | 35 (15-71) | 44 (20-68) | p < 0.001 |
| Anti-CCP level IU/mL (range) | 312.1 (10.2-3162) | 16.4 (9-95) | 20.9 (0.7-25.9) | p < 0.001 |
| Anti-CCP + (%) | 65 (85.5) | 33 (21.1) | 2 (3.7) | p < 0.001 |
| Anti-CarP level AU/mL (range) | 197.9 (2.6-2000) | 161 (50.8-477.2) | 154 (59.5-408) | p < 0.001 |
| Anti-CarP + (%) | 32 (42.1) | 8 (5.1) | 5 (9.2) | p < 0.001 |
| Rheumatoid factor level (range) | 157 (0-529.5) | 6.0 (0-34.9) | 4.7 (0.1-19.3) | p < 0.001 |
| Rheumatoid factor + (test-) | 21 (2) * | 1 (23) * | 2 (28) * | p < 0.001 |
| Smoker (%) | 6 (7.9) | 31 (19.8) | 6 (11.1) | p < 0.001 |
| eRA < 1 years (%) | 18 (23.6) |
Thumbnail
Figure 1
Data distribution for autoantibodies. A: RF; B: anti-CCP, C: anti-CarP, and D: the correlation analysis. The dashed line indicates the cut-off values for each measure. The figure was produced with the ggplot2 R package.
Data distribution for autoantibodies. A: RF; B: anti-CCP, C: anti-CarP, and D: the correlation analysis. The dashed line indicates the cut-off values for each measure. The figure was produced with the ggplot2 R package.
Table 2
Agreement of Anti-CCP with anti-CarP tests in the study population
Agreement of Anti-CCP with anti-CarP tests in the study population
| Variable | anti-CarP+ | anti-CarP- | Total | Statistic |
|---|---|---|---|---|
| Anti-CCP + | 32 | 68 | 100 | Agreement = 0.72 |
| Anti-CCP - | 13 | 174 | 187 | Kappa = 0.28 |
| Total | 100 | 187 | 287 |
Thumbnail
Figure 2
Bland-Altman plot for Anti-CCP and anti-CarP test. The X-axis represents the log transformed average of the values obtained by the two tests ([Anti-CCP + anti-CarP]/2) and the Y-axis represents the differences of the two tests (Anti-CCP-anti-CarP). The horizontal dashed lines indicate the 95% confidence limits.
Bland-Altman plot for Anti-CCP and anti-CarP test. The X-axis represents the log transformed average of the values obtained by the two tests ([Anti-CCP + anti-CarP]/2) and the Y-axis represents the differences of the two tests (Anti-CCP-anti-CarP). The horizontal dashed lines indicate the 95% confidence limits.
Diagnostic value for anti-CCP and anti-CarP tests
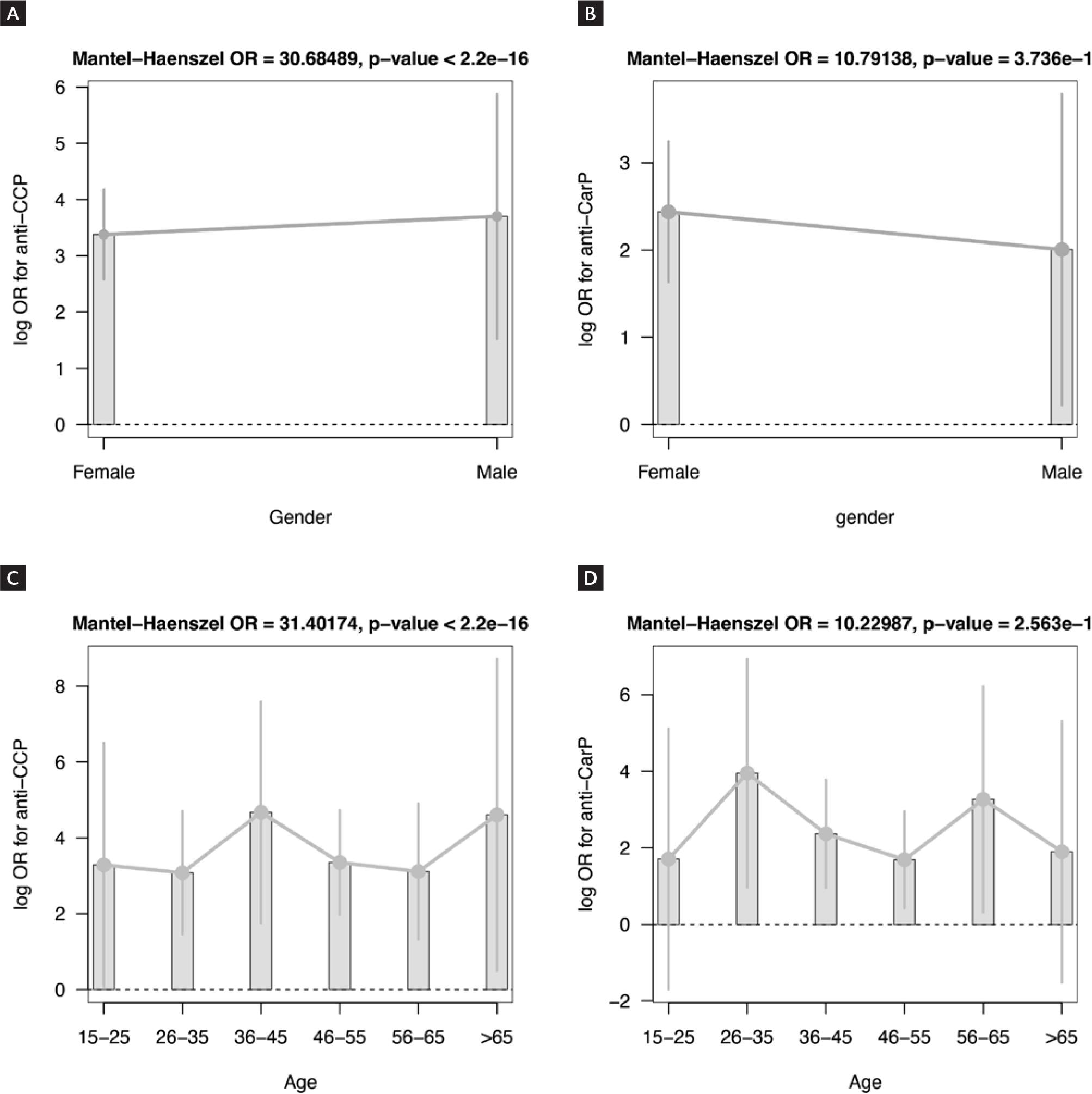
To assess the OR of having RA associated with anti-CCP and/or anti-CarP positivity, the lsRA, eRA, and FstD groups were compared to the healthy control group (Table 3). The OR in anti-CCP-positive subjects was higher than that of anti-CarP-positive subjects in all group comparisons, even when an anti-CarP cut-off of 293.2 was applied (Table S1). In the FstD group, the OR of anti-CCP was significant but the OR of anti-CarP was not. Considering the similar OR results pertaining to anti-CarP and the similar data distributions of anti-CCP and anti-CarP (Fig. 1B and C), we calculated ORs after merging the lsRA group with the eRA group (to form an “RA group”) and merging the FstD group with the healthy control group (to form a “non-RA group”) (Table 4). Again, the OR in anti-CCP-positive subjects was higher than the OR in anti-CarP-positive subjects, even after correcting for confounding variables (Fig. 3A-D). Hence, anti-CCP was more strongly associated with RA than anti-CarP. Sensitivity and specificity were also calculated (Table 4). The sensitivity of the anti-CCP test (85%) was higher than that of the anti-CarP test (43%), but the specificity of the anti-CarP test (96%) was higher than that of the anti-CCP test (74%). Thus, the anti-CCP test is more useful for diagnosing individuals with RA, and the anti-CarP test is more useful for ruling out the disease, which is concordant with the OR results. Based on the above-described results we analyzed the serial and parallel use of both assays. When both tests were applied in parallel the sensitivity increased to 91.4%, and when the tests were used in series the specificity increased to 98.4%. Hence both tests either in series or parallel could improve the diagnostic accuracy.
Table 3
Individuals with positive and negative results to anti-CarP and anti-CCP tests antibodies and their OR compared to the healthy group
Individuals with positive and negative results to anti-CarP and anti-CCP tests antibodies and their OR compared to the healthy group
| Test | LsRA |
eRA |
FstD |
Healthy |
LsRA-healthy OR |
eRA-healthy OR |
FstD-healthy OR |
|---|---|---|---|---|---|---|---|
| anti-CCP + | 51 | 14 | 33 | 2 | 189.42 |
91 |
6.9 |
| anti-CCP - | 7 | 4 | 124 | 52 | |||
| anti-CarP + | 25 | 7 | 8 | 5 | 7.42 |
6.236 |
0.53 |
| anti-CarP - | 33 | 11 | 149 | 49 |
Table 4
Odds ratio for the rheumatoid arthritis and healthy merged groups
Odds ratio for the rheumatoid arthritis and healthy merged groups
| Variable | RA (%) | Healthy (%) | Total (%) | Statistic |
|---|---|---|---|---|
| anti-CarP (+) | 32 (71.1) | 13 (28.9) | 45 (100) | OR = 11.07 |
| anti-CarP (-) | 44 (18.2) | 198 (81.8) | 242 (100) | |
| Total | 76 (26.5) | 211 (73.5) | 287 (100) | |
| anti-CCP (+) | 65 (65) | 35 (35) | 100 (100) | OR = 29.7 |
| anti-CCP (-) | 11 (5.9) | 176 (94.1) | 187 (100) | |
| Total | 76 (26.5) | 211 (73.5) | 287 (100) |
Thumbnail
Figure 3
A and B: Natural log and the Mantel-Haenszel OR for tests by gender, C and D: and age strata.
A and B: Natural log and the Mantel-Haenszel OR for tests by gender, C and D: and age strata.
DISCUSSION
A timely diagnosis is critical to improving the prognosis of RA. Early treatment has been shown to be highly effective and significantly impact the quality of life and financial burden of patients, their families, and healthcare institutions26. Several tests have been used in the diagnosis of RA. Worldwide the medical community has adopted the anti-CCP test to assist in the diagnosis of RA5. Despite this, to the best of our knowledge, the anti-CCP and anti-CarP tests are not routinely used in our clinical setting, and instead, RF is commonly used. It has been suggested that the anti-CarP test may be another useful diagnostic tool because a high percentage of subjects with RA are seronegative for anti-CCP but seropositive for anti-CarP10. The presence of anti-CarP in anti-CCP-negative RA patients is reported to be strongly associated with joint erosion, and thus anti-CarP testing can also yield prognostic information10,27.
-
26El costo de las principales enfermedades reumáticas inflamatorias desde la perspectiva del paciente en México.Gac Med Mex., 2008
-
52010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative.Arthritis Rheum., 2010
-
10Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage.Proc Natl Acad Sci USA., 2011
-
10Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage.Proc Natl Acad Sci USA., 2011
-
27Association of the presence of anti-carbamylated protein antibodies in early arthritis with a poorer clinical and radiologic outcome: data from the French ESPOIR cohort.Arthritis Rheumatol., 2017
In the present study, anti-CCP and anti-CarP antobodies were evaluated in healthy subjects in conjunction with FstD relatives of RA patients. Although there were similar levels of autoantibodies in healthy subjects (Fig. 1), there was a significant difference in OR when the FstD group was compared with the healthy control group, suggesting that consanguinity may be an influential factor for anti-CCP-positive tests and a propensity to develop RA. Anti-CCP-positive patients may have the shared epitope, explaining this finding. On the other hand, the anti-CCP test was highly associated with RA patients (including lsRA and eRA patients), even after accounting for confounding variables such as age and sex (Fig. 3A-D). Interestingly, experimental and clinical studies have demonstrated that anti-CCP and anti-CarP exhibit a degree of cross-reactivity16,17,28. In agreement analysis in the present study, only a small proportion (32/287) of subjects were double positive, suggesting that cross-reactivity with citrullinated and carbamylated proteins may have been limited in the study population. Concordantly, the correlation between the two tests was also poor.
-
16Anti-carbamylated protein antibodies are present in arthralgia patients and predict the development of rheumatoid arthritis.Arthritis Rheum., 2013
-
17Anti-carbamylated protein antibodies in the pre-symptomatic phase of rheumatoid arthritis, their relationship with multiple anti-citrulline peptide antibodies and association with radiological damage.Arthritis Res Ther., 2015
-
28Anti-CarP antibodies in two large cohorts of patients with rheumatoid arthritis and their relationship to genetic risk factors, cigarette smoking and other autoantibodies.Ann Rheum Dis., 2014
Regarding diagnostic utility, previous studies have reported that the sensitivity of the anti-CCP test is higher than its specificity7,8. In the current study, the anti-CCP test exhibited higher sensitivity than that reported in previous studies7-9. This result may be partially explained by the same studies utilizing 1987 ACR criteria, which are inherently less sensitive to early arthritis. In contrast to the anti-CCP test, the anti-CarP test was more specific but exhibited lower sensitivity. The diagnostic value of the anti-CarP test suggested in the present study is similar to that described by Brink et al.17 who reported a specificity of 97% and sensitivity of 42% in Swedish patients. Hence, the anti-CarP test may be more useful for ruling out RA, and the anti-CCP test may be more useful for diagnosing RA. Similar results pertaining to the sensitivity and specificity of anti-CCP and anti-CarP testing were reported in a recent meta-analysis29. The present study suggests that anti-CCP and anti-CarP tests could be applied simultaneously (favoring sensitivity) or sequentially (favoring specificity). In fact, several studies report that combined laboratory tests (anti-CCP, RF, and anti-CarP) outperform individual tests to diagnose RA30. Thus, our results of the combination of both tests may be relevant in different clinical scenarios regarding RA diagnosis and treatment and particularly in seronegative RA. Implementation of these tests in the public health institutions in Mexico is a pending necessity that would allow for early identification of RA patients in the early stages of the disease as well as high-risk individuals. Further studies should address the cost-benefit of using CCP and CarP tests to improve outcomes and limit disability in these high-risk groups.
-
7Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis.Ann Intern Med., 2007
-
8Systematic review: accuracy of anti-citrullinated peptide antibodies for diagnosing rheumatoid arthritis.Ann Intern Med., 2010
-
7Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis.Ann Intern Med., 2007
-
9Comparison of two assays to determine anti-citrullinated peptide antibodies in rheumatoid arthritis in relation to other chronic inflammatory rheumatic diseases: assaying anti-modified citrullinated vimentin antibodies adds value to second-generation anti-citrullinated cyclic peptides testing.Biomed Res Int., 2014
-
17Anti-carbamylated protein antibodies in the pre-symptomatic phase of rheumatoid arthritis, their relationship with multiple anti-citrulline peptide antibodies and association with radiological damage.Arthritis Res Ther., 2015
-
29Meta-analysis: diagnostic accuracy of anti-carbamylated protein antibody for rheumatoid arthritis.PLoS One., 2016
-
30Anti-carbamylated protein (Anti-CarP) antibodies in patients evaluated for suspected rheumatoid arthritis.Diagnostics, 2022
The current study had several limitations. It was a cross-sectional study with heterogeneous age and gender proportions between groups. The sample size of the eRA group was also small.
In conclusion, anti-CCP antibodies are more prevalent than anti-CarP antiobodies in Mexican patients with RA. Anti-CCP is strongly associated with RA and may also identify FstD at risk of developing RA. The anti-CCP test is more sensitive for the diagnosis of RA than the anti-CarP test, but the anti-CarP test is more specific. Both tests can be utilized in parallel and series, improving their diagnostic value. Both anti-CCP and anti-CarP could be used routinely in medical practice, to enhance diagnostic accuracy and thus facilitate timely treatment decisions.
ACKNOWLEDGMENTS
L. A. Trouw is listed as an inventor on a patent application for the detection of anti-CarP antibodies in RA. The other authors declare that they have no conflicts of interest.
This work was supported by the "Instituto Mexicano del Seguro Social" and "Consejo Nacional de Ciencia y Tecnología" (grant numbers FIS/IMSS/PROT/PRIO/13/028 JAEM and JECD-FOSSIS-CONACYT 262304). E.E. Lara-Ramírez was supported by the "Secretaría de Investigación y Posgrado, Instituto Politécnico Nacional" through grant PRORED-2024". We thank Dr O. Proudfoot from Edanz Group (www.edanzediting.com/ac) for editing this manuscript.
SUPPLEMENTARY MATERIAL
Supplementary data are available at 10.24875/RIC.24000181. These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.
REFERENCES
-
1.Wouters F, Maurits MP, van Boheemen L, Verstappen M, Mankia K, Matthijssen XM, et al. Determining in which pre-arthritis stage HLA-shared epitope alleles and smoking exert their effect on the development of rheumatoid arthritis. Ann Rheum Dis. 2022;81:48-55. Links
-
2.Kourilovitch M, Galarza-Maldonado C, Ortiz-Prado E. Diagnosis and classification of rheumatoid arthritis. J Autoimmun. 2014; 48-9:26-30. Links
-
3.Chauhan K, Jandu JS, Brent LH, Al-Dhahir MA. Rheumatoid arthritis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK441999 [Last accessed on 2023 Mar 01]. Links
-
4.Pope RM, McDuffy SJ. IgG rheumatoid factor. Relationship to seropositive rheumatoid arthritis and absence in seronegative disorders. Arthritis Rheum. 1979;22:988-98. Links
-
5.Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;69: 2569-81. Links
-
6.Van Hoovels L, Studholme L, Cruyssen BV, Sieghart D, Bonroy C, Nagy E, et al. Standardisation of ACPA tests: evaluation of a new candidate reference preparation. Ann Rheumat Dis. 2022;81: 1379-84. Links
-
7.Nishimura K, Sugiyama D, Kogata Y, Tsuji G, Nakazawa T, Kawano S, et al. Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med. 2007;146:797-808. Links
-
8.Whiting PF, Smidt N, Sterne JA, Harbord R, Burton A, Burke M, et al. Systematic review: accuracy of anti-citrullinated peptide antibodies for diagnosing rheumatoid arthritis. Ann Intern Med. 2010;152:456-64. Links
-
9.Díaz-Toscano ML, Olivas-Flores EM, Zavaleta-Muñiz SA, Gamez-Nava JI, Cardona-Muñoz EG, Ponce-Guarneros M, et al. Comparison of two assays to determine anti-citrullinated peptide antibodies in rheumatoid arthritis in relation to other chronic inflammatory rheumatic diseases: assaying anti-modified citrullinated vimentin antibodies adds value to second-generation anti-citrullinated cyclic peptides testing. Biomed Res Int. 2014; 2014:198198. Links
-
10.Shi J, Knevel R, Suwannalai P, van der Linden MP, Janssen GM, van Veelen PA, et al. Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci USA. 2011; 108:17372-7. Links
-
11.Nakabo S. Clinical and etiological meaning of anti-carbamylated protein antibodies in rheumatoid arthritis. Immunol Med. 2018; 41:147-53. Links
-
12.Trouw LA, Rispens T, Toes RE. Beyond citrullination: other post-translational protein modifications in rheumatoid arthritis. Nat Rev Rheumatol. 2017;13:331-9. Links
-
13.Wang Z, Nicholls SJ, Rodriguez ER, Kummu O, Hörkkö S, Barnard J, et al. Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nat Med. 2007;13:1176-84. Links
-
14.Reijm S, Brehler AS, Rantapää-Dahlqvist S, Kawakami A, Maeda T, Kawashiri SY, et al. Cross-reactivity of anti-modified protein antibodies is also present in predisease and individuals without rheumatoid arthritis. Ann Rheum Dis. 2022;81:1332-4. Links
-
15.Kolarz B, Ciesla M, Rosenthal AK, Dryglewska M, Majdan M. The value of anti-CarP and anti-PAD4 as markers of rheumatoid arthritis in ACPA/RF negative rheumatoid arthritis patients. Ther Adv Musculoskelet Dis. 2021;13:1759720X21989868. Links
-
16.Shi J, van de Stadt LA, Levarht EW, Huizinga TW, Toes RE, Trouw LA, et al. Anti-carbamylated protein antibodies are present in arthralgia patients and predict the development of rheumatoid arthritis. Arthritis Rheum. 2013;65:911-5. Links
-
17.Brink M, Verheul MK, Rönnelid J, Berglin E, Holmdahl R, Toes RE, et al. Anti-carbamylated protein antibodies in the pre-symptomatic phase of rheumatoid arthritis, their relationship with multiple anti-citrulline peptide antibodies and association with radiological damage. Arthritis Res Ther. 2015;17:25. Links
-
18.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149-60. Links
-
19.Ramos-Remus C, Castillo-Ortiz JD, Aguilar-Lozano L, Padilla-Ibarra J, Sandoval-Castro C, Vargas-Serafin CO, et al. Autoantibodies in prediction of the development of rheumatoid arthritis among healthy relatives of patients with the disease. Arthritis Rheumatol. 2015;67:2837-44. Links
-
20.R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. Available from: https://www.R-project.org Links
-
21.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276-82. Links
-
22.Giavarina D. Understanding bland Altman analysis. Biochem Med. 2015;25:141. Links
-
23.Haldane JB. The estimation and significance of the logarithm of a ratio of frequencies. Ann Hum Genet. 1956;20:309-11. Links
-
24.Anscombe FJ. On estimating binomial response relations. Biometrika. 1956;43:461-4. Links
-
25.Thrusfield M. Veterinary Epidemiology. 3rd ed. Ames, Iowa: Blackwell Publishing Professional; 2005. p. 235-9. Links
-
26.Mould-Quevedo J, Peláez-Ballestas I, Vázquez-Mellado J, Terán-Estrada L, Esquivel-Valerio J, Ventura-Ríos L, et al. El costo de las principales enfermedades reumáticas inflamatorias desde la perspectiva del paciente en México. Gac Med Mex. 2008;35:225-31. Links
-
27.Truchetet ME, Dublanc S, Barnetche T, Vittecoq O, Mariette X, Richez C, et al. Association of the presence of anti-carbamylated protein antibodies in early arthritis with a poorer clinical and radiologic outcome: data from the French ESPOIR cohort. Arthritis Rheumatol. 2017;69:2292-302. Links
-
28.Jiang X, Trouw LA, van Wesemael TJ, Shi J, Bengtsson C, Källberg H, et al. Anti-CarP antibodies in two large cohorts of patients with rheumatoid arthritis and their relationship to genetic risk factors, cigarette smoking and other autoantibodies. Ann Rheum Dis. 2014;73:1761-8. Links
-
29.Li L, Deng C, Chen S, Zhang S, Wu Z, Hu C, et al. Meta-analysis: diagnostic accuracy of anti-carbamylated protein antibody for rheumatoid arthritis. PLoS One. 2016;11:e0159000. Links
-
30.Ricchiuti V, Chun KY, Yang JM, Aure MA, Gomez L, Norman GL, et al. Anti-carbamylated protein (Anti-CarP) antibodies in patients evaluated for suspected rheumatoid arthritis. Diagnostics (Basel). 2022;12:1661. Links

![Bland-Altman plot for Anti-CCP and anti-CarP test. The X-axis represents the log transformed average of the values obtained by the two tests ([Anti-CCP + anti-CarP]/2) and the Y-axis represents the differences of the two tests (Anti-CCP-anti-CarP). The horizontal dashed lines indicate the 95% confidence limits.](/img/revistas/ric/v76n6//0034-8376-ric-76-6-243-fg2.jpg)