Servicios Personalizados
Revista
Articulo
Indicadores
 Citado por SciELO
Citado por SciELO Accesos
Accesos
Links relacionados
 Similares en SciELO
Similares en SciELO
Compartir
Boletín médico del Hospital Infantil de México
versión impresa ISSN 1665-1146
Bol. Med. Hosp. Infant. Mex. vol.69 no.2 México mar./abr. 2012
Artículo de investigación
Direct medical costs of treating Mexican children under 2 years of age with respiratory syncytial virus
Joaquín F. Mould-Quevedo,1 Iris Contreras-Hernández,2 Silvia Martínez-Valverde,3 Miguel A. Villasis-Keever,4 Víctor M. Granados-García,5 Guillermo Salinas-Escudero,3 Onofre Muñoz-Hernández3
1 Health Economics and Outcomes Research Director, Latin America and Primary Care Products, Pfizer Laboratories, Mexico, D.F., Mexico
2 Hospital General de Zona 1-A Venados, Instituto Mexicano del Seguro Social (IMSS), Mexico, D.F., Mexico
3 Centro de Estudios Económicos y Sociales en Salud (CEESES), Hospital Infantil de México Federico Gómez, Mexico, D.F., Mexico
4 Unidad en Investigación en Epidemiología Clínica, Hospital de Pediatría, Centro Médico Nacional Siglo XXI, IMSS, Mexico, D.F., Mexico
5 Unidad de Investigación de Economía de la Salud, IMSS, México, D.F., México
Corresponding author:
Mtro. Guillermo Salinas Escudero
CEESES, Hospital Infantil de México Federico Gómez,
Dr. Márquez 162, segundo piso, Col. Doctores,
Delegación Cuauhtémoc, 06720 México, D.F., México.
Tel: 52289917, ext. 3001.
E-mail: guillermosalinas@yahoo.com
Received for publication: 3-16-12.
Accepted for publication: 4-4-12.
Abstract
Background. Respiratory syncytial virus (RSV) is the most frequent etiologic agent causing lower respiratory tract infection in children <2 years of age. Between 0.5 and 3% of patients will require hospitalization. The aim of this study was to estimate the direct medical cost of treating children <2 years old with suspicion of RSV at the Instituto Mexicano del Seguro Social (IMSS).
Methods. Direct medical costs were estimated from an institutional perspective. Medical records were reviewed from patients <2 years of age who attended emergency services in second-level hospitals including subjects who required hospitalization. Estimated costs were obtained with the microcosting technique using the institutional costs from IMSS (year 2010). Costs were reported in USD (year 2011).
Results. When analyzing total medical costs, outpatient management yielded a cost of $230.0 ± $10.30 U.S. dollars (USD), whereas hospitalized patients exhibited an average cost of $8,313.20 ± $595.30 USD. The main components of outpatient management costs were emergency visits, specialist consultations and diagnostic testing (41.6%, 32.7% and 10.7% of the total cost, respectively). In the case of hospitalized patients, intensive care unit cost (89.3%) and overall hospitalization cost (6.5%) represented 95.7% of the total cost.
Conclusions. RSV is a disease that represents a significant economic burden for health care institutions, although most patients are treated on an outpatient basis.
Key words: direct medical costs, respiratory syncytial virus, microcosting.
INTRODUCTION
Respiratory syncytial virus (RSV) is the most frequent etiologic agent that causes lower respiratory tract infection in children <2 years of age.1 It is generally a benign disease; however, between 0.5 and 3% of patients will require hospitalization.2 Between 30% and 40% of children will have a lower respiratory tract infection,2-5 and it is considered to be the principal cause of bronchiolitis (60-80%) and pneumonia (20-40%) in infants, which represent the most common clinical presentations.6
There are reports of epidemiological surveillance in Mexico that make it possible to determine that circulation of respiratory viruses during winter months is similar to that of other countries.7 Etiologically, studies by Muraira et al. and Noyola et al. in patients hospitalized for lower respiratory infections with viral infections (30.7-47.2%) place RSV as the most frequent viral agent with (61.3-85.6%).8,9 The epidemiological burden of RSV is estimated at 64 million cases and 160,000 deaths each year.10 In the U.S., direct medical costs of RSV associated with hospitalizations for children between 1997 and 2000 had an average annual cost of $750 million U.S. dollars (USD).11 In Canada, these costs are quantified in the amount of $18 million USD12 where hospitalization (62%) was the most important component of direct medical costs followed by outpatient follow-up (38%).13 At the international level there are striking differences in terms of direct medical costs in the care of patients with RSV. Costs of medical care corresponding to hospitalization in patients <36 months of age were reported for Germany as $1,832 USD ($99.20 USD in the case of outpatient care, using an exchange rate of $1.64 euros to $1 USD),14 followed by those reported in Holland and Spain where the same hospital costs were $2,200 USD15 and $2,750 USD, respectively.16 Finally, the highest costs were those reported in the U.S. where the costs per hospital admission for RSV ranged from $3,799 USD to $9,000 USD.17,18
In Mexico there is no information regarding the costs involved in the care of patients with RSV; therefore, its impact on health institutions and society is unknown. Even with a high incidence of disease, the majority of RSV infections do not require medical care (ambulatory and/ or hospital). However, taking into consideration the high impact of this disease and its impact on high-risk groups (such as patients with heart disease who do require medical attention), carrying out a study that provides information to assist decision-makers in regard to resource allocation and planning within health institutions for management of RSV and its complications in Mexico is warranted.
In this regard, the objective of this study was to identify the management pattern of those patients who receive medical care for suspicion of RSV infection (with hospital and/or ambulatory management) within the public health system and the estimated direct medical costs associated with patient management.
MATERIALS AND METHODS
Given that the public health institutions cover more than two-thirds of the Mexican population, the analysis was conducted from the perspective of the public health institutions where information from Hospital General Regional of the Instituto Mexicano del Seguro Social (IMSS) located in Mexico City was used. This hospital is representative of a second-level care facility within the IMSS. To reference the importance of the IMSS, this institution covers 80.8% of the social security services in Mexico.19
A descriptive, cross-sectional, retrospective study was performed and included all patients who were seen from January 2006 to December 2009 in the emergency room and/or were hospitalized with suspicion of bronchiolitis or pneumonia. All patients with gastroesophageal reflux disease, patients with lipoidic pneumonia or with airway malformations were excluded.
A review of medical records was done using a survey that identified the principal demographic and clinical characteristics of the patients (gender, age, weight, height) as well as resources utilized for their management (dose, frequency, duration, quantities, etc.). This review covered information up to 1 year of patient follow-up from the initial contact in case the patient returned to the hospital due to a complication related to the first encounter. The survey used was previously validated in a pilot study by a group of medical experts within the hospital.
Cost analysis was carried out using a case-mix technique. In the case of services used, unit costs were determined, whereas for estimation of drug costs, the microcosting technique was used (adjusting the calcu lation according to the presentation and corresponding unit price).
Sources of information used were costs of institutional care (IMSS 2010)20 and unit costs for purchasing drugs by the IMSS during 2010.21 Due to the duration of the study, no discount rate in the costs is used.
Total costs were divided according to the principal cost components and according to whether they corresponded to ambulatory and/or hospital medical care. For each component percentage of utilization, average values of the monetary equivalent expressed in Mexican pesos (year 2010) were presented as well as its standard deviation (SD) and/or resource utilization rates. To generate more robust estimates in the estimation of the SD of the costs, adjustment by means of the bootstrap technique was used.22 For statistical analysis, Excel 2007 and Stata v.10 software were used. Results are reported in USD where an exchange rate of $12 Mexican pesos to $1 USD was used.23
RESULTS
A total of 74 patients who were treated during the study period were analyzed; 46% (n = 34) were managed as outpatients and 54% (n = 40) required hospitalization. Among the principal characteristics of the patients, females represented 52.7% of the sample. Average age of the patients was 10.78 (±8.2) months. Average weight was 8.23 (±2.5) kg and average height was 68.0 (±10.0) cm (Table 1).
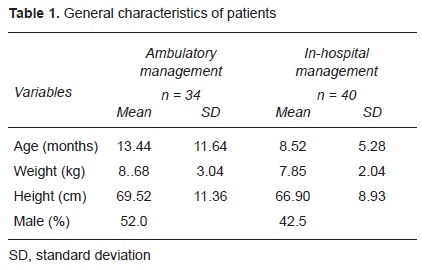
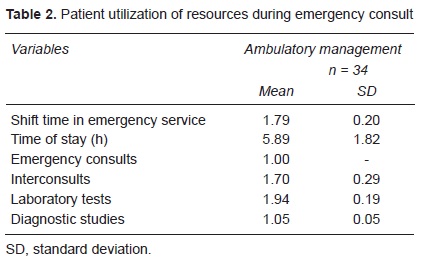
For patients who received outpatient treatment, the average length of stay was 5.89 ± 1.82 h. With regard to the resources used, a consistent pattern was found for these patients. Among these averages were included interconsultations (inhalation therapy and, to a lesser degree, cardiology) and chest x-ray; 50% had venous infusion as part of their treatment (Table 2). Of the hospitalized patients, 100% were admitted through the emergency room. In order to calculate the total resources utilized for these patients, it is necessary to add the resources previously reported for outpatient management. The resources detailed here correspond to hospital management (Table 3).
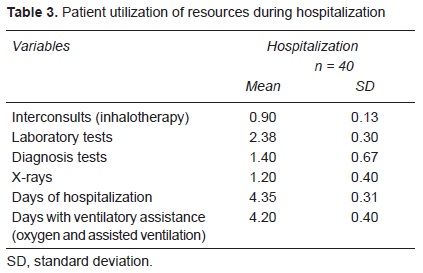
Patients managed in the hospital had an average hospital stay of 4.35 ± 2.6 days; 98% of patients required ventilatory therapy support, 90% required an additional consultation and a new battery of diagnostic and laboratory studies. Total average cost for patients who received out- patient management was $230.0 ± $10.35 USD, whereas for patients admitted to the hospital the average cost was $8,313.2 ± $595.36 USD (Table 4).
In patients with outpatient management, a percentage of the total costs were for emergency room consultation (41.6%), interconsultation (32.7%), diagnostic/imaging studies (10.7%), costs for venous infusion (7.1%), laboratory tests (5.9%) and, finally, medications and solutions, which together represent 1.9%.
In those patients requiring hospital management, the principal component of the total cost was represented by hospitalization (95.7% of the total cost, intensive care 89.3% and general hospitalization 6.5%), placement of central venous catheter (CVC) 2.0%, interconsultations 0.7%, and ventilatory support and diagnostic/imaging studies 0.5%. The remainder of the resources used represented 0.2%.
DISCUSSION
Emergency services in the IMSS hospitals have a specified length of stay in the emergency room as a maximum of 3 h. One of the important findings in this study was that 20% of the patients exceeded the specified waiting times. Another important finding in the review of the medical records and which was widely discussed with the physicians was the existing problem of lack of rapid diagnostic tests to confirm the etiology of the cases treated in the emergency department, which leads to the following three problems:
1) Without a supportive diagnosis, an increased length of stay in the emergency department is generated in order to assess patient progress.
2) Lack of accurate diagnosis implies that, in some cases, antibacterial coverage was administered to the patient with this type of infection.
3) Increase in wait time in the emergency room generates a saturation of service and high costs for other patients who arrive for such services.
These three factors increase the actual cost of treatment of patients with RSV within the institution.
When comparing the costs obtained per episode of outpatient management of $230 USD in this study with those costs reported in Germany by Ehlken et al. ($99.20 USD),13 we find that the cost obtained in our study is almost 2.3 times greater. Similarly, we found that our corresponding costs for hospital management reported in our study ($8,313 USD) were greater than those reported by Miedema et al.15 ($2,200 USD) and Diez Domingo et al.16 ($2750 USD) for various European countries; however, these were found to be within the range of those reported for the U.S. Health System by Stewart et al.17 and Pelletier, et al.18 of $3,800 USD-$9,000 USD.
Information reported in this study may be valuable in terms of management for decision-makers because it identifies two main aspects: 1) to obtain costs associated with management of patients presenting to medical services with RSV and 2) to identify a niche of opportunity to improve patient management with the use of rapid diagnostic tests and to improve utilization of resources within emergency services of the institution. Performance of these tests does not necessarily establish the best alternative; however, it provokes an opportunity for possible further studies including patient characteristics, cost-effectiveness or cost-benefit for the patient and/or institution.
One of the limitations of this study is that the corresponding information regarding patient severity was not included, which may provide additional information to explain the somewhat prolonged observation of patients.
Finally, we are aware that the use of medical records as a source of information to determine resource utilization may be a limitation due to underreporting of information normally associated with these types of clinical records.
Estimating the management of patients <2 years of age who seek public health services with suspicion of RSV represented an average direct medical cost of $275 USD in the case of patients managed on an outpatient basis and $7,739 USD in the case of patients requiring hospitalization.
REFERENCES
1. Levy BT, Graber MA. Respiratory syncytial virus infection in infants and young children. J Fam Pract 1997;45:473-481. [ Links ]
2. Meissner HC, Welliver RC, Chartrand SA, Law BJ, Weisman LE, Dorkin HL, et al. Immunoprophylaxis with palivizumab, a humanized respiratory syncytial virus monoclonal antibody, for prevention of respiratory syncytial virus infection in high risk infants: a consensus opinion. Pediatr Infect Dis J 1999;18:223-231. [ Links ]
3. Wright AL, Taussig LM, Ray CG, Harrison HR, Holberg CJ. The Tucson Children's Respiratory Study. II. Lower respiratory tract illness in the first year of life. Am J Epidemiol 1989;129:1232-1246. [ Links ]
4. Darville T, Yamauchi T. Respiratory syncytial virus. Pediatr Rev 1998;19:55-61. doi: 10.1542/pir.19-2-55. [ Links ]
5. Dubois B, Ray G. Viral infections of the lower respiratory tract. In: Taussig LM, Landau LI, eds. Pediatric Respiratory Medicine: New York: Elsevier; 1999. pp. 573-579. [ Links ]
6. Murtagh P, Cerqueiro C, Halac A, Avila M, Salomón H, Wissenbacher M. Acute lower respiratory infection in Argentinian children: a 40 month clinical and epidemiological study. Pediatr Pulmonol 1993;16:1-8. [ Links ]
7. Miranda-Novales G, Solórzano-Santos F, Leaños-Miranda B, Vázquez-Rosales G, Palafox-Torres M, Guiscafre-Gallardo H. Blood culture and respiratory syncytial virus identification in acute lower respiratory tract infection. Indian J Pediatr 1999;66:831-836. doi:10.1007/BF02723847. [ Links ]
8. Muraira GA, Villareal CE, Quiroga GA, Ábrego MV, Duran RAG, Cárdenas CBG, et al. Agentes virales en niños hospitalizados por infecciones respiratorias bajas. Rev Mex Pediatr 2002; 69;185-189. [ Links ]
9. Noyola DE, Rodríguez-Moreno G, Sánchez-Alvarado J, Martínez-Wagner R, Ochoa-Zavala JR. Viral etiology of lower respiratory tract infections in hospitalized children in Mexico. Pediatr Infect Dis J 2004;23:118-123. [ Links ]
10. World Health Organization. Acute respiratory infections (update September 2009). Respiratory syncytial virus and parainfluenza viruses. Available at: http://www.who.int/vaccine_research/diseases/ari/en/index2.html [ Links ]
11. Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr 2003;143(suppl 5):S127-S132. [ Links ]
12. Langley JM, Wang EE, Law BJ, Stephens D, Boucher FD, Dobson S, et al. Economic evaluation of respiratory syncytial virus infection in Canadian children: a Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study. J Pediatr 1997;131:113-117. [ Links ]
13. Ehlken B, Ihorst G, Lippert B, Rohwedder A, Petersen G, Schumacher M, et al. PRIDE Study Group. Economic impact of community-acquired and nosocomial lower respiratory tract infections in young children in Germany. Eur J Pediatr 2005;164:607-615. [ Links ]
14. Banco Nacional de México. Tipo de cambio EUA. Tipo de cambio promedio Dólar/Euro 2005. Available at: http://www.banamex.com/esp/finanzas/historicos/economia_int/ei_eua_cambio.jsp?init=2005&offset=7 [ Links ]
15. Miedema CJ, Kors AW, Tjon A Ten WE, Kimpen JL. Medical consumption and socioeconomic effects of infection with respiratory syncytial virus in The Netherlands. Pediatr Infect Dis J 2001;20:160-163. [ Links ]
16. Díez Domingo J, Ridao López M, Úbeda Sansano I, Ballester Sanz A. [Incidence and cost of hospitalizations for bronchiolitis and respiratory syncytial virus infections in the Autonomous Community of Valencia in Spain (2001 and 2002)]. An Pediatr (Barc) 2006;65:325-330. [ Links ]
17. Stewart DL, Romero JR, Buysman EK, Fernandes AW, Mahadevia PJ. Total healthcare costs in the US for preterm infants with respiratory syncytial virus lower respiratory infection in the first year of life requiring medical attention. Curr Med Res Opin 2009;25:2795-2804. [ Links ]
18. Pelletier AJ, Mansbach JM, Camargo CA Jr. Direct medical costs of bronchiolitis hospitalizations in the United States. Pediatrics 2006;118:2418-2423. [ Links ]
19. Secretaría de Gobernación. Anexo Estadístico Tercer Informe de Gobierno, Felipe Calderón Hinojosa. Estadísticas Nacionales. México; 2009. pp. 251-270. [ Links ]
20. Diario Oficial de la Federación. Instituto Mexicano Seguro Social. Costos Unitarios de Atención Médica. May 18, 2010. Available at: http://dof.gob.mx/nota_detalle.php?codigo=5143097&fecha=18/05/2010 [ Links ]
21. Instituto Mexicano del Seguro Social. Portal de Transparencia México. IMSS va a comprar. IMSS compró. January-December 2010. Available at: http://www.imss.gob.mx/transparencia/Pages/index.aspx. [ Links ]
22. Glick HA, Doschi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Handbooks in Health Economic Evaluation. Great Britain: Oxford University Press; 2007. pp. 89-113. [ Links ]
23. Diario Oficial de la Federación. Banco de México. Tipo de cambio para solventar obligaciones denominadas en moneda extrajera pagaderas en la República Mexicana. March 24, 2011. Available at: http://www.notasfiscales.com.mx/indicadores.html [ Links ]














