Introduction
The European System for Cardiac Operative Risk Evaluation (EuroSCORE) is a probabilistic model designed in 1999 to estimate the risk of death in patients undergoing major cardiac surgery.1,2 The model has shown good calibration, with chi-square (χ2) of Hosmer-Lemeshow (H-L) of 7.5, p2. It was initially published in an additive version and later in a logistic version, both of which have been evaluated in multiple latitudes and countries, showing generally good performance.3-7
Nevertheless, in recent years, some authors pointed out that the additive version of the EuroSCORE model overestimated mortality risk in low-risk patients and underestimated it in high-risk patients.8 On the other hand, several authors have shown that both the additive and logistic versions of the model overestimated risk, especially in high-risk patients.9-15 As a result of this situation, the Score underwent a redesign and was published in 2012, adopting the name EuroSCORE II.16
Some variables of the old model were redefined or modified; for example, renal function was evaluated by creatinine clearance with cut-off points of 85 mL/min, 50-84 mL/min, < 50 mL/min, and on dialysis, replacing the previous one based on serum creatinine levels. The variable neurological dysfunction was replaced by poor mobility due to neurological diseases and musculoskeletal diseases; pulmonary arterial hypertension was redefined as < 30 mm Hg, 30-55 mm Hg, and > 56 mm Hg. In total, 18 variables constitute the EuroSCORE II model. The new model has a predicted mortality of 3.95% and observed mortality of 4.18%, as well as discrimination evaluated through the AUC-ROC of 0.8095 and calibration through the χ2 of H-L of 15.48 with p < 0.0505. The calibration of the model was also assessed using the risk-adjusted risk ratio (RAMR), with a score of 1.058, which shows good calibration of the score.17,18
The EuroSCORE II model has been subjected to external validation in different latitudes, with contradictory results.19-25 It has nevertheless been used to evaluate the risk of mortality in patients undergoing cardiac surgery in our institution without confirmatory studies of its relevance.
Therefore, the present study aimed to evaluate the calibration and discrimination of the EuroSCORE II model in patients undergoing cardiac surgery at the Hospital Regional de Alta Especialidad del Bajío (HRAEB).
Material and methods
Inclusion and exclusion criteria
An observational, cross-sectional, retrospective study was conducted at the Hospital Regional de Alta Especialidad del Bajío (HRAEB) in León, Guanajuato, Mexico. The study population consisted of all records (343) of patients who underwent cardiac surgery between 2008 and 2013. The inclusion criteria included having undergone cardiac surgery with and without a heart-lung machine and having all the information requested by the EuroSCORE II model. Four cases were eliminated since they did not contain the information requested by the model, and one case was triplicated, resulting in a total of 338 cases that were included.
Data collection
Four Cardiology and Cardiac Surgery Service physicians collected data from clinical records that met the inclusion criteria. A structured, purpose-built instrument was used to gather the information. The following variables were obtained: demographics, comorbidities, unadjusted mortality until hospital discharge, defined as death occurring during the index hospitalization; type of surgery, defined as the procedure or procedures performed during the index surgery whether it was a) valve surgery, b) coronary revascularization surgery, c) surgery to correct congenital malformation(s) and d) surgery of a different type (valve surgery plus coronary revascularization surgery, aortic surgery, closure of postinfarction ventricular septal defect, traumatic heart injury, pericardial resection). In addition, the variables required for the calculation of the EuroSCORE II mortality risk score were collected using the online calculator on the EuroSCORE website: https://www.euroscore.org/index.php?id=1 Data of the participants, obtained from the clinical file, were subjected to an anonymization procedure to dissociate the personal data from the holder, not allowing the participant to be identified due to the structure, content or degree of disaggregation.
Statistical analysis
Quantitative variables are presented as means and standard deviations if normally distributed or as median and interquartile ranges when not normally distributed. Qualitative variables are presented as frequency percentages and compared with χ2, or Fisher’s exact test. Quantitative variables of two groups were compared with Student’s t-test when normally distributed and comparison of three or more averages with analysis of variance (ANOVA). A significance level of p ≤ 0.05 was accepted.
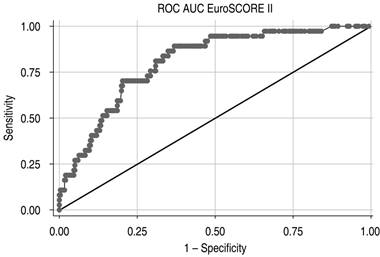
Discrimination is the ability of a mathematical model to identify patients who will survive from those who will die (accuracy), and it was evaluated by the area under the receiver operating characteristic curve (AUC-ROC). Values ≤ 0.5 indicate that the model does not discriminate better than chance, and values of one indicate perfect discrimination. Values greater than 0.75 identify systems with good model discrimination capability.
The calibration compares the expected episodes with the observed ones across the risk range. It was evaluated using the χ2 of the H-L goodness-of-fit test, which calculates a C-statistic which measures the difference between the model’s expected mortality values and the mortality values observed in risk decile groups of the population studied. The lower the value of this statistic and the p-value > 0.05, the better the calibration of the model (expected and observed mortality are close, and there is no statistical difference between them). A p-value greater than 0.05 suggests that the model has a good calibration and consequently predicts the probability of dying for patients across the risk range well.
We also calculated the RAMR obtained by the coefficient of observed mortality to expected mortality (RAMR = O/E), which has also been proposed to evaluate calibration.18 A ratio of 1.0 means that the score or test model predicts mortality in a perfect way (the same number of [observed] patients die as the number of expected [predicted] patients). A RAMR > 1.0 means that the model underestimates mortality, while a RAMR < 1.0 implies that the model overpredicts (overestimates) mortality.18
Finally, to obtain final results, a 1000-sample bootstrap procedure was conducted, using robust errors, taking care of any possible errors derived from the distribution of the data and the reduced sample size.
Microsoft Excel spreadsheet was utilized as the database, and descriptive and inferential statistics were performed in Stata version 16.
Results
The present study was a retrospective review of 338 consecutive patient records of patients who underwent cardiac surgery with or without a heart-lung machine at the HRAEB. The mean age and standard deviation (SD) of the evaluated population were 49.9 ± 16.6 years with a range of 16-80 years. 47.9% were women. The average weight was 67.2 ± 14.4 kg; 32.8% were overweight, and 18% had obesity. 26.9% had diabetes mellitus, a higher Figure than that observed in our general population; 45.2% had systemic arterial hypertension, also higher than that observed in our general population, and 30.7% were smokers (Table 1).
Table 1: General characteristics and comorbidities of the study population (N = 338).
| Characteristic | n (%) |
|---|---|
| Age [years], mean ± SD (range) | 49.87 ± 16.6 (16-80) |
| Age groups [years] | |
| ≤ 50 | 139 (41.12) |
| 51-60 | 101 (29.88) |
| 61-70 | 72 (21.30) |
| ≥ 70 | 26 (7.69) |
| Gender | |
| Male | 176 (52.07) |
| Female | 162 (47.93) |
| Weight [kg], mean ± SD | 67.21 ± 14.49 |
| Height [cm], mean ± SD | 160.06 ± 0.93 |
| Body mass index [kg/m2], mean ± SD | 26.07 ± 5.05 |
| Underweight [< 18.5] | 17 (5.03) |
| Normal weight [18.5-24.9] | 135 (39.94) |
| Overweight [25.0-29.9] | 111 (32.84) |
| Obesity I [30.0-34.9] | 61 (18.05) |
| Obesity II [35.0-39.9] | 11 (3.25) |
| Obesity III [≥ 40.0] | 3 (0.89) |
| Diabetes mellitus type II | 91 (26.92) |
| Insulin-dependent diabetes | 42 (12.4) |
| Non-insulin dependent diabetes | 49 (14.49) |
| Systemic arterial hypertension | 153 (45.26) |
| Hypercholesterolemia | 78 (23.08) |
| Hypertriglyceridemia | 105 (31.07) |
| Smoking | 104 (30.77) |
SD = standard deviation.
The surgical procedures performed were valve surgery 108 (31.95%), coronary artery bypass surgery 101 (29.88%), congenital surgery 51 (15.08%), and miscellaneous surgery 78 (23.07%). The aortic clamping time and extracorporeal circulation time were 88.7 ± 43.4 and 118.88 ± 54.4 minutes, respectively. Thirty-seven patients died during the index hospitalization (10.9%) (Table 2). Table 3 shows the number and percentage of each of the variables of the EuroSCORE II model found in our study population. Table 4 compares the variables found in the population from which the EuroSCORE II was obtained and the population evaluated at the HRAEB. The population from which the EuroSCORE II model was derived was almost 15 years older than our study population (64.6 vs 49.9 years). Body weight (77.9 vs 67.2 kg) and height (168.5 vs 160 cm) were also higher. The prevalence of chronic obstructive pulmonary disease (10.7 vs 6.2), the percentage of emergent surgery (4.3 vs 0.9), isolated coronary revascularization (46.7 vs 29.9), and valve surgery (45.5 vs 31.9) were also more frequent in the EuroSCORE II population than in our population.
Table 2: Surgical procedures.
| Procedure | n (%) |
|---|---|
| Valvular | 108 (31.95) |
| Aortic valve replacement | 33 (9.76) |
| Mitral valve replacement + tricuspid repair | 23 (6.80) |
| Mitral valve replacement | 20 (5.19) |
| Mitral and aortic valve replacement | 12 (3.55) |
| Tricuspid valve replacement | 7 (2.07) |
| Mitral valve replacement + coronary revascularization | 6 (1.77) |
| Mitral, aortic, and tricuspid valve replacement | 4 (1.18) |
| Valve conduit + coronary reimplantation | 3 (0.88) |
| Isolated coronary artery bypass grafts | 101 (29.88) |
| Off-pump coronary artery bypass | 77 (76.25) |
| Single-vessel coronary artery bypass | 8 (2.36) |
| Double-vessel coronary artery bypass | 43 (12.72) |
| Triple-vessel coronary artery bypass | 46 (13.60) |
| More than triple-vessel coronary artery bypass | 4 (1.18) |
| Congenital anomalies | 51 (15.08) |
| Atrial septal defect | 24 (7.10) |
| Patent ductus arteriosus | 7 (2.07) |
| Coarctation of the aorta | 5 (1.47) |
| Ventricular septal defect | 4 (1.18) |
| Tetralogy of Fallot | 3 (0.88) |
| Ebstein’s anomaly | 1 (0.29) |
| Other congenital anomalies | 7 (2.07) |
| Miscellaneous | 78 (23.07) |
| Pericardial window/resection | 34 (10.05) |
| Thoracic aorta | 23 (6.80) |
| Myxomas | 6 (1.77) |
| Epicardial permanent pacemaker | 5 (1.47) |
| Post-infarction ventricular septal rupture | 3 (0.88) |
| Metastatic tumors | 3 (0.88) |
| Stab wounds | 2 (0.59) |
| Gunshot wounds | 1 (0.29) |
| IV septum rupture + free wall rupture due to MI | 1 (0.29) |
| Aortic clamp time, mean ± SD | 88.7 ± 43.4 |
| Extracorporeal circulation time, mean ± SD | 118.88 ± 54.4 |
| Patients who died | 37/338 (10.95) |
Table 3: Distribution, number, and percentage of EuroSCORE II variables in the study.
| Characteristic | n (%) |
|---|---|
| Patient-related factors | |
| Age [years], mean ± SD | 49.87 ± 16.61 |
| Women | 162 (47.93) |
| Extracardiac arteriopathy | 19 (5.62) |
| Creatinine clearance (Cockcroft-Gault) [mL/min] | |
| 85 | 201 (59.46) |
| 50-85 | 101 (29.88) |
| < 50 | 16 (4.73) |
| On dialysis | 20 (5.91) |
| Poor mobility | 25 (7.39) |
| Previous cardiac surgery | 47 (13.90) |
| Chronic obstructive pulmonary disease | 21 (6.21) |
| Active endocarditis | 24 (7.10) |
| Critical preoperative condition | 49 (14.49) |
| Diabetes under insulin control | 42 (12.42) |
| Cardiac-related factors | |
| NYHA functional class | |
| Class I | 46 (13.6) |
| Class II | 172 (50.9) |
| Class III | 95 (28.1) |
| Class IV | 25 (7.4) |
| SCC class IV angina | 39 (11.5) |
| Left ventricular ejection fraction | |
| More than 50% | 223 (65.97) |
| 31-50 | 113 (33.43) |
| 21-30 | 2 (0.59) |
| ≤ 20 | 0 (0.00) |
| Recent myocardial infarction | 46 (13.64) |
| Pulmonary artery systolic pressure [mmHg] | |
| No | 115 (30.02) |
| Moderate [31-54] | 171 (50.59) |
| Severe [≥ 55] | 53 (15.68) |
| Surgery-related factors | |
| Type of surgery | |
| Elective | 179 (53.0) |
| Urgent | 155 (45.9) |
| Emergency | 3 (0.9) |
| Salvage | 1 (0.3) |
| Extent of surgery | |
| Isolated CABG | 90 (26.6) |
| One non-CABG procedure | 189 (55.9) |
| Two procedures | 38 (11.2) |
| Three procedures | 21 (6.2) |
| Surgery on the thoracic aorta | 23 (6.8) |
NYHA = New York Heart Association. SCC = Canadian Society of Cardiology. CABG = coronary artery bypass grafts.
Table 4: Variables from the present study and the EuroSCORE cohort.
| Variable | HRAEB | EuroSCORE II |
|---|---|---|
| Number, n | 338 | 22,381 |
| Age [years], mean | 49.9 | 64.6 |
| Women, % | 47.9 | 30.9 |
| Weight (kg), mean | 67.2 | 77.9 |
| Height (cm), mean | 160 | 168.5 |
| Diabetes mellitus (total), % | 26.9 | 25.0 |
| Insulin-dependent diabetes, % | 12.4 | 7.6 |
| Chronic obstructive pulmonary disease, % | 6.2 | 10.7 |
| Poor mobility, % | 7.4 | 3.2 |
| Extracardiac arteriopathy, % | 5.6 | |
| Infective endocarditis, % | 7.4 | 2.2 |
| Serum creatinine [mg/dL] | 1.2 | 1.3 |
| Ejection fraction, % | ||
| > 50 | 65.9 | |
| 31-50 | 33.4 | |
| 21-30 | 0.6 | |
| < 20 | 0.0 | |
| Critical preoperative status, % | 14.5 | 1.7 |
| Emergency surgery, % | 0.9 | 4.3 |
| Isolated CABG, % | 29.9 | 46.7 |
| Valve surgery, % | 31.9 | 45.5 |
| EuroSCORE II, % | 4.1 | 3.9 |
HRAEB = Hospital Regional de Alta Especialidad del Bajío. CABG = coronary artery bypass grafts.
In contrast, the percentage of women (47.9% vs 30.9%), insulin-dependent diabetes mellitus (12.4% vs 7.6%), poor mobility (7.4% vs 3.2%), infective endocarditis (7.4% vs 2.2%), and critical preoperative status (14.5% vs 1.7%) were higher in the present series. The predicted risk in the EuroSCORE II model was 3.95%, and in this study group, it was 4.10%.
The EuroSCORE II model in the present study had an AUC-ROC of 0.806 (95% CI, 0.739-0.872), consistent with good discrimination (Figure 1). The χ2 of H-L was 14.2, with p = 0.08, which is compatible with good calibration. However, the other tool proposed to evaluate calibration, the RAMR,18 was 2.65, consistent with the EuroSCORE II model, generally underestimating perioperative mortality in our series (Figure 2).
Discussion
Implementing a mathematical model to predict operative mortality in cardiac surgery requires evaluating its performance in the hospital where it is to be used. The present study included a retrospective series of 338 adult patients who underwent cardiac surgery and aimed to evaluate the discrimination and calibration of the EuroSCORE II model in the HRAEB.
The EuroSCORE model for predicting perioperative mortality in general cardiac surgery in adult patients was widely used in the first decade and part of the second decade of the present century in various latitudes, showing generally good predictive performance. Nevertheless, it has shown deficiencies in its calibration while retaining good discrimination in recent years. For this reason, the model was updated in 2012 and called EuroSCORE II.
The new model improved its discrimination: AUC-ROC 0.8095 (95% CI, 0.7820-0.8360) and its calibration, χ2 of H-L of 15.48, with p < 0.0505.16 In addition to being evaluated by the classical χ2 method of H-L goodness-of-fit, the calibration was also assessed by the RAMR, which was 1.058.
Like the EuroSCORE II, our study included patients who underwent general cardiac surgery (ischaemic, valvular, congenital, and mixed) with and without a heart-lung machine. Compared to the population used by Nashef et al., from which the EuroSCORE II model was derived,16 our population appears to have advantages concerning risk: younger population, lower prevalence of chronic obstructive pulmonary disease, and emerging surgeries. However, it was more prevalent in other relevant prognostic variables: more women, insulin-dependent diabetes mellitus, poor mobility, infective endocarditis, and preoperative critical condition (Table 4). Therefore, it is unsurprising that the EuroSCORE II in our population was higher but only slightly compared to the original EuroSCORE II model population, 4.10% vs 3.95%.
On the other hand, several studies have evaluated the discrimination and calibration of the EuroSCORE II model with contradictory results. Some studies corroborate good to very good discrimination and good calibration, while other studies, although corroborating good discrimination, question its calibration. Di Dedda et al., in a retrospective series of 1,090 patients, report discrimination, with AUC-ROC of 0.81 (95% CI, 0.78-0.83) and good calibration, with an observed mortality of 3.75%, expected of 3.10 and conclude that «the EuroSCORE II represents a useful update of the previous version of the EuroSCORE, with much better clinical performance and the same good level of accuracy».26 Barili et al., in a retrospective validation study of the new model involving 12,325 general cardiac surgery patients report an AUC-ROC of 0.82 (95% CI, 0.80-0.85) consistent with good discrimination and «optimal calibration but only up to 30% of predicted mortality».23 Gao et al., in a series of 1,628 Chinese patients, reported good discrimination with AUC-ROC of 0.90 and good calibration, with the χ2 of H-L of 0.071 (p > 0.05). However, discrimination and calibration decreased efficiency up to five years after patient follow-up.27 Borracci et al., in a prospective series of 2,000 Argentinean patients undergoing general cardiac surgery, reported an AUC-ROC of 0.80 (95% CI, 0.75-0.85), compatible with good discrimination and χ2 of H-L values of 11.4 (p = 0.178), consistent with good calibration.28 Kinkel et al., in a retrospective series of 704 adult patients undergoing general cardiac surgery, found an AUC-ROC of 0.821 (95% CI, 0.772-0.871) and a χ2 of H-L = 17.7, p = 0.64, consistent with good discrimination and calibration. In the present retrospective study of 338 patients who underwent general cardiac surgery, we found AUC-ROC of 0.806 (95% CI, 0.739-0.872) compatible with good discrimination and a χ2 of H-L of 14.2, p = 0.08, suggestive of adequate calibration.24
García-Valentín et al. report the results of a prospective study conducted in Spain to validate the EuroSCORE II in which 20 Spanish hospitals participated, recruiting 4,034 adult patients who underwent general cardiac surgery. The AUC-ROC was 0.78 (95% CI, 0.76-0.82), compatible with good discrimination, and χ2 of H-L of 38.98 (p < 0.001), consistent with poor calibration.29 In the same sense, Kunt et al., in a retrospective series of 428 adult patients from Turkey who underwent coronary artery bypass surgery, found an AUC-ROC of 0.72 (95% CI, 0.62-0.81), compatible with acceptable discrimination. The observed mortality was 7.9%, the predicted mortality by EuroSCORE II was 1.7%, and they concluded that while the model showed good discrimination, it significantly underestimated the risk of perioperative death.22
The RAMR has yet to be used in most studies evaluating the calibration of the EuroSCORE II model, with some exceptions. For example, Alvarez-Cabo, in an ambispective series of 206 adult Spanish patients undergoing coronary revascularization surgery, in addition to the χ2 of H-L to evaluate calibration, also used the RAMR, with a point value of 0.83, suggesting a slight overestimation of the model, supported by the 95% confidence interval of the point value of the RAMR reported.29 Similarly, Borracci et al., in their prospective series of 2,000 Argentinean adult patients undergoing general cardiac surgery, used in their calibration evaluation in addition to the χ2 of H-L the RAMR, whose point value was 1.4 suggestive of slight underestimation of risk; «the clinical validation of the model, based on the ratio of observed/expected mortality, showed that the system performed better in the lowest and highest risk groups while underestimating the risk in the intermediate groups.»28
We used the present work’s H-L χ2 and the RAMR to evaluate the calibration. According to χ2 of H-L, the model has an adequate calibration. Nevertheless, according to the RAMR (point value 2.65), the model, in general, underestimates the risk of death in our study population; in graph 2, we can see how, in the first deciles, the model overestimates the risk, but in the high-risk deciles, underestimation of the risk predominates.
In this study, the observed mortality of 10.9% stands out, higher than that reported in the EuroSCORE II and multiple validation studies in European and Anglo-Saxon populations, but similar to that reported in our country: 9.68% in the Rodriguez-Chávez series of 1,188 valve surgery patients to validate the EuroSCORE30 and 12.5% at 30 days reported in the Kinkel series of 704 patients undergoing general cardiac surgery.24 The explanation for this high mortality is given by factors related to the patient: biological status, socioeconomic status, and low health education that leads to seeking medical attention late, when the condition has already produced advanced structural and functional cardiac and extracardiac damage,30 as well as factors related to health care centers: resources, infrastructure, experience, previous results, among others.31
In summary, the performance of the updated EuroSCORE II model evaluated in our population showed good discrimination. As assessed by χ2 of H and L, the calibration suggests adequate calibration. However, when calibration was evaluated using the RAMR, the result was consistent with underestimating the risk of death, in line with the observed mortality.
Limitations
The study’s period and the presentation of the results are long. However, the model has retained relevance and contributes to re-evaluating the EuroSCORE II calibration measure. Future studies should include patients who intervened during recent years and increase the sample size or design a prospective study with an adequate sample size to have a fairer evaluation of the performance of the EuroSCORE II model in the Mexican context.
Conclusions
In the present study, the EuroSCORE II model showed good discrimination and adequate calibration based on the χ2 data of Hosmer and Lemeshow. However, the data obtained from the RAMR indicates that the model underestimates the risk of death in the medium- and high-risk groups of patients. Considering the limitations mentioned above, we considered continuing the EuroSCORE II instrument in the hospital where the study was conducted. Ultimately, it is necessary to design a model to measure the risk of operative mortality in cardiac surgery in Mexico that includes characteristics and variables specific to the Mexican population, not contemplated so far by traditional international instruments.











 nueva página del texto (beta)
nueva página del texto (beta)