Introduction
Medicine had a fast evolution since science allowed a better understanding of health and disease, and technology paved the way for prevention and control. However, the art of medicine, which includes variability in all its expressions and human preferences and attitudes, puts medicine suddenly inside the complexity that rules the function of the universe including biology, and human behavior. Decision-making in the daily settings of medical practice incorporates data derived from investigations that are proven effective under some rules that are not universal and leave much room for improvement.1
Stephen Jay Gould, an anthropologist from Harvard University, wrote many years ago that nature is not conformed by clearly defined entities but works in many different levels that interact diffusely in their borders. Now the concept is named «complexity», and in the words of the German scientist Hans-Peter Dürr, «the whole is greater than the sum of its parts and the new paradigm is complexity instead of reductionism».
The large number of medical papers published negates the possibility of reading all of them, even if the selection is limited only to one topic.2 Some groups help by classifying the papers according to their quality, but even so, they are too many, and the selection methods have been subject to criticism. Another method for applying clinical investigation to the daily practice of medicine is to follow the recommendations of clinical guides. However, currently, there are too many clinical guidelines of very different quality, and some of them are signaled as having different types of bias, like lack of preparation of the authors and conflicts of interest by obeying not the scientific evidence but the industry’s interests.3,4
Paradigms are the backbone of medical recommendations and give the false security of interpreting them as rock-solid concepts. Nevertheless, history tells us that the opposite is true; as an example, Mayo Clinical Proceedings published an analysis in which, after ten years of publication, only 40% of the concepts remained state of the art.5
Among the published papers, there will be some that are relevant to the care of patients. According to J Ioannidis, most investigation in science is of low quality, so it is necessary to identify those with good quality (internal validity) and which can be applied to a particular setting (external validity or applicability in the real world).6
The Cochrane foundation lists those whose qualify was evaluated by the GRADE method. However, to properly evaluate which of them must be chosen to read, many published methods aim to rate their quality and the possible impact on medical care rather than accepting the authors’ conclusions and recommendations.7
The Cochrane foundation mentioned above published its ladder of evidence (Figure 1 and Table 1), where they place the backup of any medical recommendation in one of three steps. The first one is named «efficacy» and includes those concepts derived from medical papers but without confirmation in various settings. At best, they have been shown to function in near-to-ideal settings. Karl Popper states that there should be falsification studies before a concept is confirmed. Even so, currently, they are never done because of a lack of financial backup and the interest to continue promoting findings that will not be reproduced in new investigations. The second step is effectiveness which can be reached when the «epidemiological arrow» described by Jeremiah Stamler points in the right direction by the added value of several studies. Confirmation studies and their application in clinical settings must corroborate the data obtained in the initial clinical trials. The third step relates to the cost/benefit ratio. While medical associations give their advice, this step falls within the realm of governments and official agencies, where decisions take place concerning priorities in money expenditure.
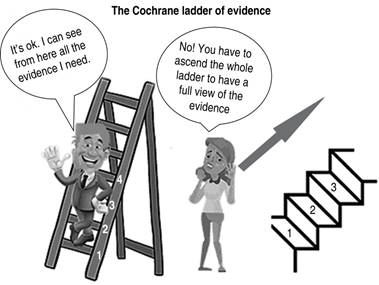
Figure 1: It should be clear for everybody, that for a new and just identified concept you have to ascend the whole staircase before it is established as a solid paradigm and then observe the direction of the epidemiological arrow as described by Jeremiah Stamler.11,12
Table 1: Interpretation of the Cochrane ladder of evidence.13),(14
| Can it work? | Under ideal circumstances, the degree of the intervention producing more benefit than harm | Efficacy | Step 1 |
| Does it work? | The same concept but in the clinical setting | Effectiveness | Step 2 |
| Is it worthwhile? | Measures the intervention effect vs its cost | Cost/benefit ratio | Step 3 |
Notwithstanding all the limitations that medical knowledge confronts, clinicians must decide which recommendations apply to a particular patient and circumstance in every consultation. Here is a list of some scientific characteristics that back up the concept of clinical applicability and will help in the decision.
Rules for clinical applicability
1. Look for the causality rules (Koch, Bradford Hill, Evans). Although subject to some criticism, they give a good view to distinguish etiological and risk factors, and those which are merely accompanying and not causal ones
2. Identify the absolute or attributable risk reduction and do not accept only the relative risk reduction or the risk ratios. Their confidence limits are used to calculate the statistical significance but do not measure the size of the effect. Furthermore, sometimes when the effect is small, the absolute risk reduction is hidden, so it is necessary to dig further to find it.
3. The number needed to treat (NNT): how many patients are to be treated to obtain a reduction of the endpoint selected (i.e., mortality of morbidity). The number needed to harm (NNH): how many patients are treated for every harm or complication detected. Although there is no precise number, the ratio of NNT/NNH must be in favor of the benefits. For example, Sacket published that an NNT greater than ten is unacceptable. However, others currently considered beneficial interventions in medicine stray far from that point, with some numbers reaching the hundreds.
4. Internal and external validity. Those investigations with a proper design, valid protocol, and representative sample, adequately executed, evaluated, and presented, excel over those poorly done. Besides, we must consider at the top of quality evaluation those investigations based on meta-analysis and prospective randomized medical trials, followed by non-randomized trials, retrospective, cohort, and case/control studies. At the bottom are the observational studies and original case reports, which with some exceptions usually indicate the need for more advanced trials. Again, there are exceptions, but as one goes up in the ladder of the quality class of investigations, there is evidence of better scientific merit and a lower bias risk.
5. A good prognosis of greater survival in the first five or ten years must be confirmed in different settings. Clinical trials are the best scenario that an intervention will have. Usually, the actual level of its benefit must be observed in subsequent trials or observational studies during its clinical application (i.e., databases or real-world studies).
6. Clinical setting varies widely from controlled clinical trials (CCT). Patients will differ in their characteristics and their preferences. Other points include economic issues and acceptance to perform a study or to follow a treatment. The physicians’ points of view will also influence the application of the procedure or treatment.
7. Be aware of distraction and even of deceit and fraud. The general under-preparation in epidemiology and biostatistics makes physicians feel overwhelmed by numerical information, so before it is too late, practitioners must start their instruction in scientific methodology.8
8. Do not consider statistical significance as the main factor in judging the quality of a study. In recent decades, based on the publications of Sir Ronald Fischer and the statisticians and clinical researchers who refined and adopted them, the statistical significance of research findings has become the main factor to consider. Researchers put it as their primary factor «p fishing», and readers of publications rely on that number to decide on the «success or failure» of the study. However, it must be emphasized that the more important thing is the size of the effect (i.e., correlation, comparison), and these facts are not measured by the «p» values or the confidence limits of the central tendency.9 In contrast, there are many more points that can guide decision-making. The pillars that support decisions in medicine are its proportions of art and science that comes, in the words of Sir William Osler, from the pursuit of excellence, the practice of abstraction, and learning the method. We could add here the practice of common sense.10











 nueva página del texto (beta)
nueva página del texto (beta)


