Introduction
Heart Failure (HF) is a public health problem with a high mortality rate. A recent United States of America (USA) study found that the deaths caused by HF had increased from 275,000 in 2009 to 310,000 in 2014.1 In Europe, the incidence of HF is 3/1,000 people per year (all age groups) or 5/1,000 people per year in adults.2,3 The treatment for HF is costly for any country. In the USA, the annual cost of HF in 2010 was estimated at $39.2 billion, corresponding to 2% of the total US healthcare budget.4 A revision from different European countries found similar HF-related costs for overall health care expenditure.5,6 Not many studies have evaluated the incidence of HF in Latin America. Ciapponi et al.7 report an incidence of 199 cases per 100,000 person-years, a prevalence of 1%, and a 1-year mortality rate of 24.5%; for these reasons, it is imperative to optimize HF management. Cardiac Resynchronization Therapy (CRT) reduces morbidity and mortality in selected patients8 and improves cardiac function and quality of life.9,10 The currently approved class IA indication for CRT is in patients with optimal drug therapy who are still symptomatic and have Left Ventricle Ejection Fraction (LVEF) < 35%, QRS width > 150 ms and QRS morphology of Left Bundle Branch Block (LBBB).11 Despite implementing CRT in patients with class I recommendation, the rate of non-response is up to 30%.12-14 Although, studies have shown that response rates range from 32 to 91%, depending on the criteria used to define response.15 The definitions adopted in randomized essays versus clinical practice remain discrepant. Clinical essays typically measure variables based on events, while less defined criteria are used in practice. Various definitions of CRT response have been proposed, and the response rate is different in every case.15,16 Response rates are higher when clinical parameters such as symptoms are used but much lower when using outcome measures or ventricular remodeling.12 For this study, the definition by Hu YR et al.17 was used, in which after one year of follow-up, patients were defined as non-responders if the LVEF increased 24.5 ± 3.7% vs 26.2 ± 4.0% or less with a reduction of the Left Ventricle End-Diastolic Diameter (LVEDD) of 76.8 ± 6.3% vs 75.3 ± 7.3%. Patients were classified as responders if their LVEF increased by 27.4 ± 5.2% vs 42.5 ± 10.4% or more and had a reduction of the LVEDD of 70.3 ± 9.1 vs 61.8 ± 10.3 mm or greater. Many parameters have been used to predict non-response to CRT, such as electrocardiographic, echocardiographic and clinical parameters. Hu YR et al,17) after much logistic regression analysis, found that two variables were strongly associated with non-response to CRT after one year of follow-up: fragmented QRS and LVEDD ≥ 77 mm. If any of the two was present, the probability of non-response was 14-17%; if both variables were present, the probability of non-response was close to 50%. For this study, electrocardiographic and echocardiographic features pre-CRT and their association with non-response to the therapy were analyzed.
Material and methods
A retrospective and observational study was performed with patients from the cardiology department of the ISSEMyM Medical Center of Toluca (IMCT), who were treated with CRT with or without an Implantable Cardioverter Defibrillator (ICD) from June 1st, 2003, to June 1st, 2019. A sample of 24 patients was used. The inclusion criteria were 18 years old or older, both genders and having received CRT. Exclusion criteria were a basal QRS length of less than 120 ms and patients with LVEF of 40% or greater before the procedure. The only elimination criterion was death before the control echocardiogram post-CRT. The electrocardiographic features analyzed were the length of the QRS, the presence of LBBB and the presence of a fragmented QRS complex previous to the CRT. The echocardiographic feature was the end-diastolic diameter of the left ventricle previous to the CRT. A descriptive statistics analysis was performed using normality and symmetry tests for the quantitative variables. The minimum, maximum, median and standard deviation were calculated, with a 95% confidence interval for the median. For the qualitative variables, we obtained absolute and relative frequencies; cross-tabulation for variables association. Inferential statistics consisted of applying Pearson’s χ2 test, the one-factor ANOVA test and Wilcoxon’s test, all with a p-value < 0.05. The database was organized in excel, and we used the SPSS program 22 version for the analysis.
Results
A total of 24 patients were included, two were excluded, and two were eliminated. The average age was 65.8 ± 12.0 years, with a minimum of 38 years and a maximum of 88 years. Sixteen patients were classified as responders, and eight patients as non-responders. When comparing age among groups, no statistically significant differences were found. The distribution by gender mainly corresponded to males, with 79% (19 cases). When comparing gender among groups, no statistically significant association was found. However, it is worth noting that 100% of the females were responders, vs 57.9% of males, with an Odds Ratio (OR) of 1.7 times for the female gender. Previous LBBB was associated with response to CRT with statistical significance, with a protection odds ratio of 0.722 times. We found that 75% of the patients with a fragmented QRS complex were non-responders to CRT (Table 1).
Table 1: Association between a fragmented QRS complex and response to Cardiac Resynchronization Therapy.
| Fragmented QRS complex | Responder | Total | |
|---|---|---|---|
| Yes n (%) |
No n (%) |
||
| Yes | 6 (37.5) | 6 (75.0) | 12 (50.0) |
| No | 10 (62.5) | 2 (25.0) | 12 (50.0) |
| Total | 16 (100.0) | 8 (100.0) | 24 (100.0) |
Figure 1: shows a comparison between pre-LVEDD and post-LVEDD. The investigators found that patients with the highest values of LVEDD pre-CRT, with a mean of 77 mm, were classified as non-responders, vs a mean value of 63 mm for patients classified as responders.
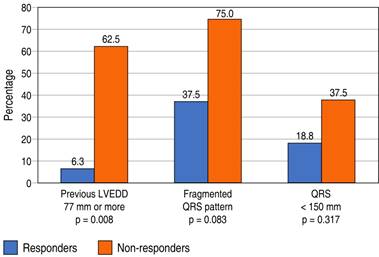
Figure 2: shows a comparison of the frequency of the different variables and their association with the response or non-response to CRT. It is noticeable that the percentage of responders was greater in patients without a fragmented QRS pattern in their electrocardiogram, with a previous LVEDD smaller than 77 mm and a QRS length equal to or greater than 150 ms, though only the LVEDD < 77 mm previous to CRT was statistically significant.
In counterpart, Figure 3 shows the association between the variables and non-responders. It is evident that the variable that had a greater association with non-response to CRT was the fragmented QRS pattern, with 75%, though without statistical significance. 62.5% of patients with an LVEDD of 77 mm or greater were classified as non-responders, with statistical significance. The length of the QRS < 150 ms was present in 37.5% of non-responders without statistical significance.
Discussion
Many trials have found electrocardiographic features associated with response to CRT, such as the length of the QRS > 150 ms and the presence of LBBB.18,19 Moreover, they have also used echocardiographic parameters like the LVEF, LVEDD and the Left Ventricular End-Systolic Volume Index (LVESVI) to determine the positive response to CRT.18,19 However, very few studies have been designed to find predictors of non-response. After a comprehensive revision of the literature, we found only two trials designed that way.17,20 Hu YR et al.17 found that the presence of a fragmented QRS and a dilated LVEDD prior to CRT are strong predictors of non-response. In patients with both features, the rate of non-response was 46.2%. Shanks M et al.20 concluded that patients with a shorter QRS duration (150.6 ± 29.9 milliseconds vs 156.0 ± 32.5 milliseconds, p = 0.041) and larger left atrial volumes (44.9 ± 16.9 mL/m2 vs 40.9 ± 17.6 mL/m2, p = 0.006) were more frequently non-responders. In the present study, we found that most patients with QRS length < 150 ms were non-responders, with a p-value of 0.317. The atrial volumes were also determined, but there was no association with response to CRT. Similar to the results obtained by Hu YR et al.,17 we found that two parameters were associated with non-response to CRT, an LVEDD > 77 mm and a fragmented QRS pattern. Nevertheless, only the first one had a significant p-value. The main limitation of this study was the small sample size, it is likely that if the number of patients is increased, we might obtain more statistically significant results.
Conclusions
The LVEDD greater than 77 mm prior to the cardiac resynchronization therapy is a strong predictor of non-response. The fragmented QRS pattern previous to CRT was associated with non-response, although with a p-value > 0.05. It is necessary to do studies with much bigger sample sizes to increase these findings’ statistical significance.











 nueva página del texto (beta)
nueva página del texto (beta)