Introduction
Sudden cardiac death (SCD) is the death of a cardiovascular cause, occurring less than one hour from the onset of symptoms when it is witnessed. Alternatively, unexpected death of cardiovascular cause in an individual who was observed to be alive 24 hours prior. SCD accounts for 50% of deaths of cardiovascular origin worldwide and about 20% of mortality in the general population.1
Appropriate therapy is a shock triggered by an episode of ventricular tachycardia or ventricular fibrillation. An inappropriate therapy is a shock triggered erroneously by another arrhythmia, whether it be sinus tachycardia, supraventricular tachycardia, or excess sensor sensitivity.
Using an implantable cardioverter defibrillator (ICD) with other pharmacological therapies has become a fundamental strategy for preventing SCD.2-4 Although the most frequent indication for these devices worldwide is primary prevention,5 in Latin America, secondary prevention is the predominant indication, with a low rate of inappropriate therapies and a mortality rate similar to the reported in the world literature.6
In 2018, Aristizábal et al. published a study about the prognostic impact of defibrillator shocks in a Colombian cohort showing that mortality was 12.8%, being 1.8 times higher in patients with ischemic heart disease, who likewise had a 65% higher risk of appropriate therapies, compared to non-ischemic heart disease.7
There are no extensive studies or registries documenting the main risk factors associated with survival in patients with cardioverter defibrillator implantation.
This study aims to follow up on this initial cohort of patients with cardioverter defibrillators and determine survival and associated factors in high complexity centers in the city of Medellín.
Material and methods
A retrospective cohort of 730 patients with cardiomyopathy (of varied etiology) was carried out. The patient had a high risk of sudden death, required an ICD or cardiosynchronizer implantation, and attended the electrophysiology consultation. The follow-up was performed in eight different centers in Medellín, Colombia, between 2013 and 2020. Patients had a clinical and device six months follow-up with two controls. Patients without complete clinical history were excluded from the study.
Each follow-up appointment was performed by at least one teaching electrophysiologist accompanied by at least one electrophysiology resident. At the end of the consultation, an online data record was made in Google Drive.
All the information was obtained by review of medical records and complemented by telephone calls or an additional appointment for review if it was required. Calls and national death databases established the mortality of patients not attending rescheduled appointments.
The main objective of this study was to evaluate the survival, and related factors of patients with ICD attended in several clinics in the city of Medellin by the CES electrophysiology group between 2013 -2020.
Statistical analysis
Continuous variables were presented as mean and standard deviation (SD) or median and interquartile range according to the normal distribution, and categorical variables as absolute numbers and percentages.
A univariate analysis was performed to characterize the study population. The nature of the variables was considered; in the case of quantitative variables, the Kolmogorov-Smirnov normality test was performed to define whether the quantitative variables are presented with averages or medians.
For the bivariate analysis, the associations with respect to survival were calculated independently for each factor. The Chi-square test of independence was used for qualitative variables, and for quantitative variables, the t of Students Test or Mann-Whitney U test (quantitative-qualitative) was used.
ORs and 95% confidence intervals were also calculated from binary logistic regression.
Differences in survival according to covariates were calculated with the Log Rank test.
The association between covariates and time-to-event presentation was calculated using COX regression. A p-value of less than 0.05 was considered statistically significant. All analyses were performed with the software SPSS version 25.
Results
This study included 730 patients with a mean age of 63 years. The youngest patient at the time of implantation was 16 years old, and the oldest was 90 years old. The characteristics of the population are described in Table 1.
Table 1: Socio-demographic characteristics.
| Age (Mean ± SD) | |
| Male | 63.6 ± 11.91 |
| Female | 62.1 ± 13.95 |
| Gender (%) | |
| Male | 72.5 |
| Female | 27.5 |
| Comorbility (%) | |
| Arterial hypertension | 71.1 |
| Diabetes mellitus | 24.0 |
| Chronic kidney disease | 12.5 |
| Hypothyroidism | 23.2 |
| Dyslipidemia | 46.3 |
| Chronic obstructive pulmonary disease | 12.9 |
| Coronary artery bypass graft surgery | 7.8 |
| NYHA (%) | |
| I | 40.7 |
| II | 41.5 |
| III | 13.6 |
| IV | 0.5 |
| Ischemic cardiomyopathy | 56.7 |
| Non ischemic dilated cardiomyopathy | 43.3 |
| First LVEF (%) | |
| < 35 | 72.9 |
| > 35 | 27.0 |
| LVEF control < 35 | 19.9 |
| Secondary prevention | 37.3 |
| Primary prevention | 62.7 |
| Appropriate therapy | 20.3 |
| Inappropriate therapy | 14.7 |
| Electrical storm | 3.6 |
| Death | 23.5 |
| Complications | 15.1 |
72% of patients were male, and the most prevalent pathologies were arterial hypertension (71%) and dyslipidemia (46%), while 24% of the patients had diabetes mellitus, 13% had chronic obstructive pulmonary disease, and 12% had chronic kidney disease.
Additionally, 364 patients (56.7%) had ischemic heart disease, of which 57 (8.1%) were surgically revascularized. 72.9% had an initial ejection fraction (LVEF) less than 35%, and 15% had LVEF greater than 50%; echocardiographic follow-up showed an improvement in LVEF less than 35% in only 19.9% of patients. 40% of patients were New York functional class (NYHA) I, 41% were NYHA II, and only 0.5% were NYHA IV.
62.7% of the patients had an ICD implanted for primary prevention. 20.3% of patients had appropriate therapy, in most cases for ventricular tachycardia (11.2%). 14.7% of the patients presented inappropriate therapy; the most frequent cause was atrial fibrillation (8.5%), followed by supraventricular tachycardia other than AF in 3.8%, noise 1.2%, electrode dysfunction 0.7%, and overdetection 0.3%. The electrical storm was detected in 3.6% of the study population, defined as 3 ICD discharge therapies in 24 hours.
Kaplan-Meier curves show the cumulative survival in the follow-up of patients; total mortality was 23.5%. Figures 1, 2 and 3 show the Kaplan-Meier curves of inappropriate therapy and arterial hypertension, respectively.
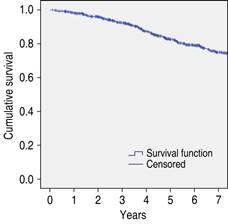
Figure 1: Kaplan Meier survival curve in patients with implanted cardioverter defibrillator implantation.
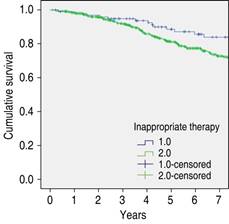
Figure 2: Kaplan Meier survival rate in patients with inappropriate implanted cardioverter defibrillator therapy.
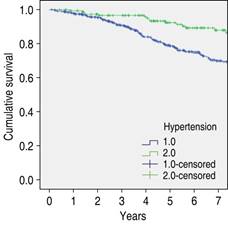
Figure 3: Kaplan-Meier survival rate in patients with arterial hypertension and implanted cardioverter defibrillator implantation.
86.6% of patients did not present any complication associated with device implantation. Among those that did occur, the most frequent was electrode displacement (9.3%), followed by infection (1.8%) and hematoma (0.4%).
In the bivariate analysis, age, presence of hypertension (p = 0), NYHA functional class III (p = 0), inappropriate therapy (p = 0.046), and presented electrical storm (p = 0.049) were significantly associated with decreased survival.
Other variables, such as sex (p = 0.34), diabetes mellitus (p = 0.36), and dyslipidemia (p = 0.35), had no direct association.
Multivariate survival analysis was performed using the Cox Proportional Hazards Model. NYHA functional class III (HR 2.96, 95% CI 1.85-5.15), the presence of arterial hypertension (HR 2.182, 95% CI 1.23-3.86), and age (HR 1.02, 95% CI 1.01-1.03) were associated with decreased survival in patients with ICD (Table 2).
Discussion
Sudden cardiac death is responsible for 50% of deaths of cardiovascular origin worldwide3,4,8 and about 20% of mortality in the general population.1 ICD, in conjunction with pharmacological and non-pharmacological treatment, has been shown to decrease mortality related to sudden cardiac death.9 In Colombia in 2018, Aristizábal et al. published a study about the prognostic impact of defibrillator shocks in a Colombian cohort, showing that mortality was 12.8%, being 1.8 times higher in patients with ischemic heart disease, who also had a 65% higher risk of appropriate therapies, compared to non-ischemic heart disease.7
In this study, the most frequent indication for implantation was primary prevention in patients with ischemic heart disease in 62% of cases, similar to what is reported in the world literature. Welsenes et al. published a long-term follow-up study of patients with implantable cardioverter defibrillators in primary and secondary prevention. 1302 (61%) patients received an ICD for primary prevention of sudden cardiac death and 832 (39%) patients for secondary prevention.5
In addition, we found that arterial hypertension was the most prevalent pathology in patients with ICD, regardless of their indication, and was the one most associated with decreased survival. Several studies have described hypertension as a recognized risk factor for sudden cardiac death.10-12 A prospective study of 7,746 patients in Paris, France, found that the presence of arterial hypertension, and more specifically elevated systolic blood pressure, had an RR of 1.23 (1.02-1.46) for sudden cardiac death and an RR of 0.02-1.37 (1.19-1.56) for fatal acute myocardial infarction.13
At follow-up, it was found that 20.3% of the patients had appropriate therapy, in most cases due to ventricular tachycardia (11.2%). 14.7% of the patients had some inappropriate therapy. The most frequent cause was atrial fibrillation (8.5%), which was associated with increased mortality in our study. Although it is known that the presence of inappropriate therapies leads to significant myocardial injury, the increase in mortality is not so clear in the literature. Studies show that inappropriate therapies correlate with deterioration in the quality of life and increased mortality.5,14 However, other recent studies have found no relationship between the presence of inappropriate therapies and mortality.15,16
The electrical storm was detected in 3.6% of the patients and was associated with a significant decrease in survival. These data correlate with those of different published studies. The MADIT II trial on ischemic heart disease as a primary prevention strategy reported an incidence of electrical storms of 4%.17
On the other hand, the complications inherent to implantation are a reality. The rate of complications reported for any adverse event varies between 12.4 to 22% for primary prevention studies and 8.0 to 22.8% for secondary prevention studies.18 In this study, 13.4% of patients presented complications, with electrode displacement being the most frequent, representing 69% of all complications reported. Other complications, such as hematoma and pocket infection, were equally or less frequent than those found in the world literature.19
Conclusions
In this study of 730 patients followed for seven years, it was found that the main indication for ICD implantation was primary prevention for ischemic heart disease. The vast majority of patients had LVEF of less than 35% at the time of implantation. It showed marked improvement during follow-up, probably related to revascularization therapies and optimal medical management.
Age, arterial hypertension, functional class, electrical storms, and inappropriate therapies were associated with significantly decreased survival. Optimal pharmacological and non-pharmacological treatment of cardiovascular risk factors in patients with ICD positively impacts survival and should always be considered during device evaluation.











 nueva página del texto (beta)
nueva página del texto (beta)


