Introduction
Penetrating cardiac trauma (PCT) has been well defined over time. It was first described in Homer’s famous Iliad, where exsanguination is described as a cause of death due to foreign objects penetrating the heart.1
Penetrating cardiac injuries are devastating injuries that currently represent a 40-90% mortality rate. Its short therapeutic window implies a surgical challenge where treatment depends on the patient’s mechanism of injury and hemodynamic status.2-6 The most affected cavity in this type of lesion is the right ventricle due to its anterior location.7 Surgical repair in PCT has improved notably in recent decades, with successful surgical results.8
Case presentation
Case 1: a 27-year-old male was brought by relatives with a stab wound in the anterior precordial region. During the physical examination, the patient was drowsy, hypotensive (80/50 mmHg), with tachycardia (110 beats/min), jugular vein distention and muffled heart sounds.
Initial laboratory tests showed a hemoglobin of 10.6 g/L with a normal white blood cell count and normal platelet count.
The surgery was performed in supine decubitus. The patient experienced a cardiac arrest during general anesthesia induction and was provided with rapid stabilization. Then a left thoracotomy with transverse sternotomy was performed via the fourth intercostal space following vascular control of the mammary arteries.
A large hematoma was found opening the pericardium in the anterior wall of the right ventricle (RV). A clot was extracted, and an internal cardiac massage was performed.
After sinus rhythm was recovered, a 1 cm wound was found in the anterior wall of the RV, near the lower margin of the heart. The wound was irrigated and closed with a 3-0 nylon suture. A 1 cm laceration was also found in the inferior wall of the RV and was closed with a 3-0 nylon suture.
The left margin of the heart was lifted with no signs of bleeding (Figure 1), and we then performed ligation of the internal mammary arteries. Subsequently, the thoracic cavity was explored with no findings of pleuropulmonary lesions (Figure 2). A 2 cm laceration in the diaphragmatic side of the liver was repaired with a 3-0 nylon suture by performing a 10 cm longitudinal incision in the epigastrium. The surgery was finished with no other complications.

Figure 1: Exposure to cardiac sutures. Suture on the anterior wall of the right ventricle (yellow arrow). Inferior wall suture (black arrow).
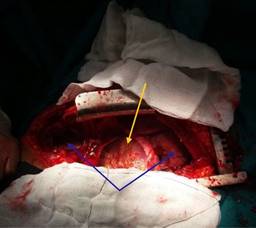
Figure 2: Left anterolateral thoracotomy with a transverse section of the sternum. Opening of the pericardium with cardiac visualization (yellow arrow) and opening of both pleurae with the observation of both lungs (blue arrows).
During the postoperative period, three units of red blood cells were transfused, and 1 gram of ceftriaxone every eight hours was administered. Days later, an exploratory laparotomy was performed because of severe persistent abdominal distension. Nevertheless, we did not find any alterations. The patient was referred to the Intensive Care Unit (ICU) of a private clinic by agreement with the ministry of health, where he evolved favorably.
Follow-up visits were made for a total period of one year after surgery, and no cardiovascular sequelae were reported.
Case 2: a 38-year-old male was admitted to the emergency department with a stab wound in the lateral region of the thorax. On admission, the patient was dyspneic, hypotensive (80/50 mmHg), with tachycardia (130 beats/min), jugular vein distention and muffled heart sounds.
Initial laboratory tests showed a hemoglobin of 8.7 g/L with a normal white blood cell count and normal platelet count.
A life-saving pericardiocentesis was performed in the emergency room and resulted in an immediate improvement of the patient’s hemodynamic status. Five units of red blood cells were transfused, and 2 grams of cefazolin and an intravenous norepinephrine infusion were administered.
The patient was rapidly taken to the operating room (OR), where a left thoracotomy was performed via the fourth intercostal space. We immediately found a cardiac tamponade that improved with the opening of the pericardium.
After blood aspiration was performed, we identified a 2 cm longitudinal laceration in the left ventricle (LV), approximately half a centimeter from the left anterior descending artery (LAD). A cross stitch was made to control bleeding, using a 3-0 nylon suture that bordered the LAD artery in the epicardium, deepening the incision below the artery and returning to the other edge of the ventricular wound to avoid kinking of the vessel and prevent the occurrence of perioperative infarction. An additional stitch was placed due to residual bleeding, and both stitches were reinforced with a pericardial patch (Figures 3 and 4).

Figure 3: View of left heart and lung: lung suture (yellow arrow), cardiac suture with a pericardial patch (white arrow).

Figure 4: View of left heart and lung: pericardial patch (black arrow), lung suture (blue arrow), anterior interventricular groove, course of the anterior descending artery (yellow arrow).
A nylon 3-0 suture was used to close a 3 cm laceration located in the lower lobe of the left lung, and we then performed ligation of the internal mammary arteries. Other structures of the thorax were checked without any abnormal findings, and a 24 cm thoracostomy tube was placed. The surgery was finished with no other complications.
During the postoperative period, the patient remained in the ICU with a thoracostomy tube for four days and an intravenous treatment of meropenem 500 mg every eight hours for seven days. The patient was discharged three days later and continued to be evaluated for one year without cardiovascular complications.
Discussion
Historically, cardiac injuries had fatal outcomes and were considered untreatable; currently, around 90% of patients die before reaching the emergency room.9 Some authors have found associations between mortality and hemodynamic status of the patient on admission, type of weapon, surgical findings, and complexity of the repair.10 In our case, the role played by the medical emergency team was crucial for the survival of these patients.
A cardiac injury should be suspected in any patient with penetrating wounds in the thorax, especially in the anterior face of the thorax, mainly on the left side, upper abdomen, and neck.11
The presence of agitation, cold extremities, venous distension of the neck, paradoxical pulses and muffled cardiac sounds in patients with penetrating wounds suggest cardiac injury with tamponade.6 Some authors consider cardiac tamponade as a protective factor for patient survival.12 The resolution of tamponade increases cardiac output, restores normal circulation, and improves anoxia.13 Cardiac tamponade was present in both our patients, where a life-saving pericardiocentesis was performed in one of them before the patient was rapidly taken to the OR.
The RV is affected more frequently than the LV due to its location and anterior extension.2 Bamous et al. showed similar results, with greater involvement of the RV (56%), 52% of which was associated with PCT.14
There are several types of approaches to dealing with PCT, including left anterior thoracotomy, right anterior thoracotomy, pericardial window, and median sternotomy. The latter is widely used due to its exposure,10 although it is not as fast as other approaches. In our cases, left thoracotomy with transverse sternotomy was performed in one patient, where a classic sternotomy would have delayed vascular control.
Several authors recognize that the survival rate after suffering a penetrating cardiac injury probably depends on the time of attention.12 Stranch et al. found a highly significant association between delay in reaching the hospital, clinical condition on admission, mechanism of injury, and aggressive surgical treatment with survival rates.15
Conclusions
Emergency thoracotomy, which is characterized by relief of tamponade and control of bleeding, is an important pillar that increases survival in patients with PCT. The left anterior thoracotomy is the fastest cardiac approach and, with its extension to a transverse sternotomy, offers wider exposure to right chambers and caval veins. After surgical intervention, the patient should undergo a thorough cardiological study to rule out intracardiac lesions.











 nueva página del texto (beta)
nueva página del texto (beta)


