Introduction
ST-elevation myocardial infarction is one of the leading causes of death worldwide, caused by the thrombotic occlusion of a coronary artery, called «culprit artery».1
Myocardial infarction involving two or more culprit arteries is uncommon in patients undergoing primary percutaneous coronary intervention, and is associated with high mortality.2 This entity is difficult to diagnose from 12-leads electrocardiography, it has been postulated that the presence of a diffuse inflammatory process, caused by occlusion of the first artery, brings about thrombosis of the others.3,4 Not practice guidelines are available for the treatment of this complication.
On the other hand, postinfarction ventricular septal rupture (PIVSR) is a mechanical complication that usually appears in the first 24 hours or three to seven days after infarction,5,6 with an incidence of 0.17-0.31%6 and a near mortality of 100% without surgery or transcatheter closure device.
The association of these pathologies is not mentioned in large retrospective studies.2,3,5,7-10 This paper presents a clinical case report of a patient with multivessel coronary thrombosis in hospital, complicated by interventricular septal rupture after a successful percutaneous intervention.
Case report
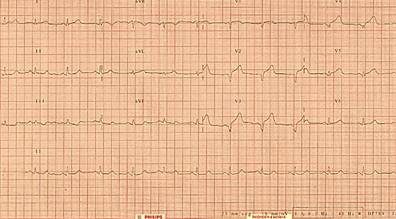
A 50 year old male, smoker during 35 years (8.75 pack-years), with negative past medical history, presented to the emergency department of a secondary care hospital 3 hours after sudden chest pain grade 8/10, accompanied by cough, nausea and vomiting. He was in Killip class II, electrocardiogram showed anterior ST-segment elevation (Figure 1), biomarkers: creatine kinase -MB 639.9 mg/dL (0-24 mg/dL), total creatine kinase 5,019 mg/dL and iTn 8.59 ng/mL (0-0.40 ng/mL). Anterior ST-elevation myocardial infarction was diagnosed, thrombolysis was performed using alteplase with door-to-needle time of 15 minutes, decreasing the ST 50%, but due to hemodynamic instability and persistent angina he was transferred to tertiary care hospital.
On arrival vital signs: BP 80/50 mmHg, SaO2 78%, T 37 oC, HR 113 bpm, RR 34 rpm. Jugular venous distention was recognized. Cardiac auscultation revealed rhythmic heart sounds, no murmurs. Lungs revealed crackling rales. No limb edema. He was intubated and vasopressors/inotropic infusion were set. Electrocardiogram showed J point elevation in DII, DIII, AVF and V1-V5 with anterior leads T wave inversion (Figure 2). Chest X-ray revealed cephalization of the pulmonary vessels, Kerley B lines, peribronchial cuffing, «bat wing» pattern, patchy shadowing with air bronchograms, and increased cardiac size (Figure 3). Coronary angiography demonstrated thrombotic occlusion of the left anterior descending and thrombotic suboclusive lesion of the right coronary artery. The patient underwent percutaneous coronary intervention of the left anterior descending with four drug-eluting stents and two drug-eluting stents in the right coronary artery, antegrade flow was restored to TIMI 3 (Figure 4).

Figure 4: Coronary angiography: A) acute occlusion in the left anterior descending artery and B) in the right coronary artery. C) TIMI III flow return from the left anterior descending artery and D) from the right coronary artery.
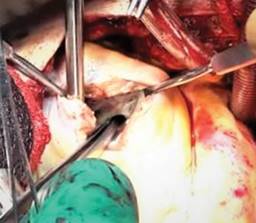
Ten hours later, he had holosystolic murmur grade III/VI without thrill at the left inferior parasternal border. The echocardiogram showed an interventricular septal rupture of 5 × 3 mm at the apical level with speed of 4.4 m/s, maximum gradient 77.6 mmHg, QP/QS 1.4, pulmonary artery systolic pressure 43 mmHg, anterior, inferior and septal wall akinesis, apex dyskinesia, without pericardial effusion, intracavitary thrombus or vegetation (Figure 5). Intra-aortic balloon counterpulsation was placed due to cardiogenic shock and, 48 hours later, the septal rupture was repaired with a bovine pericardial patch (Figure 6). Post-surgical echocardiogram revealed a residual defect 3 mm in size, with a speed of 2 m/sec. He died from refractory cardiogenic shock, before percutaneous closure with transcatheter device.

Figure 5: Echocardiogram shows a defect of the interventricular septum at the apical level with a speed of 4.4 m/s and a maximum gradient of 77.6 mmHg.
Discussion
In percutaneous coronary intervention (PCI) for acute ST-segment elevation myocardial infarction (STEMI), the main finding is thrombotic occlusion of a coronary artery, due to rupture or erosion of atherosclerotic plaque,1 known as the «culprit artery». Simultaneous thrombosis of two main coronary arteries is uncommon.2,3 It is defined as STEMI associated with angiographic visualization of two or more thrombi that cause partial or complete occlusion of at least two epicardial coronary arteries.3 The incidence is 2.5% in PCI and 50% in autopsies of patients with sudden cardiac death,11 with hospital mortality of 2 to 5%.2,3 Risk factors include: male sex, smoking and systemic arterial hypertension, with an average age of presentation of 59 years. Cardiogenic shock is the clinical presentation in 40% of cases and up to 38% requires an intra-aortic balloon pump (IABP).3
Diagnostic approach includes the search for thrombosis causes (hypercoagulable states,12 unusual coronary anatomy,13 drug-induced coronary vasospasm,14 endocarditis of the mitral or aortic valve), when they are not identified, it has been postulated that the diffuse inflammatory process of an occluded artery leads to the thrombosis of another;3,4 also, multiple plaque rupture secondary to coronary panarteritis,15,16 as well as an increase in catecholamines with platelet activation are other proposed theories.17
By electrocardiogram, acute multi-vessel involvement cannot be determined; this patient had ST elevation in anterior leads, but in retrospective studies 29% had elevation in inferior leads, 21% in anterior leads, and 41% in two territories (inferior plus anterior leads),3 so the standard diagnosis is ICP. Coronary angiography of the patient showed occlusion of the right coronary artery plus the anterior descending one; 50% of the cases have this combination.3 He was treated with a direct stent, but thrombus aspiration and the implantation of 2 V-stents are also options with good results.18
On the other hand, post infarction interventricular septal rupture (PIVSR) is a mechanical complication that causes pulmonary overcirculation and biventricular failure,6 it can occur within 24 h to several days after myocardial infarction,5 the incidence is 0, 17-0, 31% in STEMI, 49.7% due to inferior infarction and 41.1% anterior infarction,5,7,19 without having reported patients with multivessel thrombosis who developed it. The diagnostic standard is transthoracic Doppler echocardiography, with a sensitivity and specificity of 100%, but it can underestimate the size of the rupture, since many are complex (thin, akinetic, greater in systole or diastole).20 Cardiac magnetic resonance imaging provides transverse plane imaging to estimate the size of the defect;21 in this patient, it was not performed due to hemodynamic instability.
Early surgical closure is the standard of care despite the high mortality (56 ± 23%) and postoperative residual shunts (up to 20%),20 in part due to the high hemodynamic instability of the patients and the friable tissue that surrounds the PIVSR. There is the alternative of delaying surgical closure until the myocardial tissue has healed to better hold the sutures, although it is generally reserved for more stable patients. The interventional approach with a transcatheter occlusion device is considered a definitive treatment, or as a bridge to surgery (hybrid closure) with a 90% success rate in delivery, but the frequency of the residual shunt is unknown.8,22 One limitation is the anatomical complexity of the rupture, not appropriate if the size is ≥ 15 mm.22
The treatment of the patient was according to the procedures established in international guidelines; since he did not present improvement with medical treatment, intra-aortic balloon contrapulsation was placed, although the cardiogenic shock for which he was taken to surgery persisted, which did not improve his hemodynamic status in part due to residual shunt that was attributed to the friable tissue around the PIVSR. It was proposed to close with a percutaneous device; however, due to biventricular failure, he suffered a sudden death.
The 2017 European Society of Cardiology guidelines promote early surgery when there is no improvement with pharmacological treatment (vasodilator, diuretic) and the IABP does not stabilize patients; it may be delayed in patients who respond well to aggressive therapy for heart failure.23 The same guidelines mention that there is no consensus on the optimal time for surgery. Therefore, to obtain better results, the hemodynamic status of the patient, the anatomical complexity of the defect, and the availability of devices for percutaneous closure as well as a surgical team with experience in these types of complications should be evaluated.
The coexistence of both pathologies has not been reported previously (at least explicitly) in the medical literature. Probably, this association represents a subgroup with extreme mortality, and the lack of autopsy in all cases provides no help to identify them.
Conclusions
Multivessel coronary thrombosis is an uncommon angiographic finding in an acute myocardial infarction with ST-segment elevation. At this time, not practice guidelines are available for optimal treatment strategy; but restoration of coronary blood flow with thrombolysis or primary PCI, should always be the goal. The presence of PIVSR in this subgroup has not been reported or studied, due to the scarcity of cases; therefore, the gold standard management is not clearly defined, and suitable timing for surgery remains controversial. The present clinical case exposes the medical needs to clarify facts which lead to a reduction of mortality with efficient and scientific supported clinical practice guidelines.











 nova página do texto(beta)
nova página do texto(beta)