Introduction
Systemic autoimmune rheumatic diseases, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SS), spondyloarthropathies, and vasculitis (Takayasu’s arteritis [TA]), are inflammatory disorders which can all have cardiovascular (CV) clinical manifestations, for example, atherosclerosis that may lead to blood vessels stenosis. Furthermore, autoimmune disease characterized for hypercoagulable states, for example, antiphospholipid antibody syndrome (APS) gives rise to vascular disease as recurrent venous and arterial thromboembolisms, these manifestations may, in fact, be the initial presentation of the rheumatologic condition1. The National Institute of Medical Sciences and Nutrition (INCMNSZ) is a tertiary medical center and research facility in Mexico City that receives and treats a large number of patients with autoimmune diseases and vasculitis. Experience treating patients with RA, SLE, SS, and TA have been evaluated, and the influence of inflammatory markers during the early phase, clinical factors, and patient-related variables associated with disease progression has been analyzed, as well as the severity of disease, worsening ischemic symptoms, indications for interventions, and clinical outcomes2.
Atherosclerosis
RA and SLE have long been recognized as having a significant burden of atherosclerotic CV disease1,3. The other autoimmune inflammatory disorders have been less well studied given their lower prevalence, but early reports in APS and SS suggest similar increased CV risk4,5. As therapies for autoimmune diseases have improved over the past several decades, increasing patient longevity, the risk of premature atherosclerosis has become more clinically evident. It is now accepted that accelerated atherosclerosis is the leading cause of morbidity and mortality in the patient with a systemic autoimmune disease4.
Other rheumatologic conditions that are more common in women, such as SS and APS, have also been shown to exhibit accelerated atherosclerosis6,7. Inflammation and autoimmunity underscore the pathogenesis of atherogenesis seen in these conditions, similarly to RA and SLE (but possibly in varying degrees). In APS, the presence of circulating antiphospholipid antibodies (aPL) appears to be the mediator of pro-inflammatory and prothrombotic effects on the vasculature8.
Takayasu’s arteritis
TA is a rare, systemic, and inflammatory large vessel form of vasculitis of unknown etiology that may lead to occlusion or aneurysmal degeneration of the arteries in various degrees9, typically involves the aorta and its branches, as well as the pulmonary arteries; the clinical spectrum ranges from asymptomatic disease to severe ischemia, with catastrophic consequences10. This entity affects with greater frequency young Asian and Latin American individuals than other ethnic groups and has a female-to-male predominance of 5.8 to 111. The natural course of TA is characterized by cycles of active and inactive phases that reflect the different inflammatory states of the arterial lesions. During the “early” phase, symptoms indicate active inflammation and during the late or chronic phase, evidence of arterial insufficiency may become clinically present12,13.
Treatment strategies for these two phases are different; during the active phase, immunosuppressive and cytotoxic agents are used to control the development of inflammation, relieve symptoms, and restrict the extent of the affected arteries. The chronic phase may progress resulting in extensive arterial injury, and in some cases, the need for surgical or endovascular intervention (Fig. 1)13, although due to the rarity of the disease and limited experience, evidence-based consensus regarding the indications for revascularizations is lacking14.
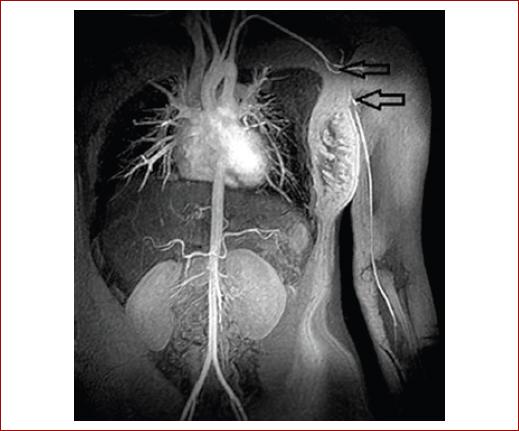
Figura 1 Magnetic resonance angiography demonstrates complete occlusion of the left axillary artery (hollow arrow) in a young woman who required surgical revascularization for disabling the left upper extremity claudication. (Reproduced with permission from Elsevier from Hinojosa et al.2.)
TA is primarily treated by pharmacological therapy, but surgical and endovascular treatment may be required to treat organ ischemia, renovascular hypertension, or aneurysmal lesions. These interventions have been performed successfully to ameliorate complications that would adversely affect the quality of life or life expectancy of patients. The initial experience with endovascular procedures was promising, but more recent data suggest that endovascular interventions are associated with a higher failure rate than open vascular reconstruction15; however, the long-term outcome over several decades has rarely been described and there are no guidelines to direct the choice between open surgery and endovascular approaches. In all cases, the technique and surgical approach for revascularization must be individualized, based on the extent of the arterial lesions and performed during the late phase16.
Patients with TA who underwent interventions had a higher erythrocyte sedimentation rate at the time of the diagnosis and active smoking was associated with progression of the disease, worsening ischemic symptoms, and the need for intervention. Revascularization procedures (open surgery or endovascular) are effective at relieving symptoms; these approaches may provide benefit to this relatively young population. Lifelong follow-up is mandatory2.
For example, in figure 2A and B, a 38-year-old female with known diagnosis of TA followed in our institution since 2000 was referred to our vascular surgery clinic with 4 months history of progressive and frequent episodes of amaurosis fugax in the left eye. A computed tomography angiography (CTA) revealed focal stenotic segments in the right common carotid artery (CCA) and internal carotid artery; near occlusion of the proximal left CCA was also present. Her physical examination was notable for bilateral carotid bruits, more accentuated on the left side. This case illustrates the clinical presentation of TA affecting both carotid arteries; open revascularization through carotid subclavian bypass grafting was successfully performed with minimal morbidity, complete resolution of symptoms, and improvement of the patient’s quality of life. As conclusion with this case report, revascularization procedures when indicated should be performed while the disease is inactive and close surveillance is mandatory16. Other forms of the presentation of AT are an isolated stenotic or occluded segment of the descending thoracic and/or the abdominal aorta associated and are very uncommon and the clinical expression is known as “middle aortic syndrome” (MAS). Manifestations depend on the lesion location and may include hypertension originating from the aortic coarctation or renovascular, buttock or lower extremity claudication, and rarely chronic intestinal angina. Its prevalence is reported below 0.000001%, with approximately 200 cases reported in the literature. As an example, a 27-year-old female with a diagnosis of TA based on the American College of Rheumatology Criteria was sent to our clinic with 1-year history of intermittent claudication in April 2012. Her physical examination was notable for diminished femoral and distal pulses bilaterally; the patient had been previously treated with immunosuppressive therapy during the inflammatory phase of the disease. A CTA revealed a stenotic lesion in the infrarenal aorta, extending to both proximal common iliac arteries (Fig. 3A). Given her young age and following discussions about open and endovascular approaches, an aortobiiliac bypass grafting using an 18 mm × 9 mm Dacron graft through transperitoneal approach with medial visceral rotation was performed (Fig. 3B). She had an uneventful recovery and at 46 months from the procedure remains without symptomatology.
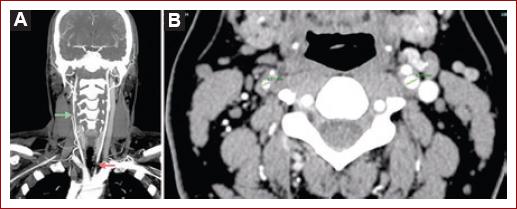
Figure 2 A and B: computed tomography angiography, coronal view demonstrated focal stenosis in the right common carotid artery (CCA) (green arrow) and near occlusion of the proximal left CCA (red arrow). Axial view shows focal stenosis in the right internal carotid artery (black hollow arrow). (Reproduced with permission from Elsevier from Hinojosa et al.2.)
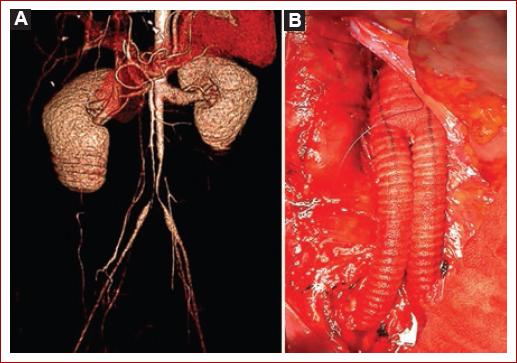
Figure 3 A and B: computed tomography angiography three-dimensional reconstruction demonstrates the stenotic lesion in the infrarenal aorta extending to the proximal common iliac arteries bilaterally. An intraoperative photograph showing the aortobiiliac reconstruction with an 18 × 9 mm Dacron graft. (Reproduced with permission from Elsevier from Hinojosa et al.2.)
MAS associated with TA requiring surgical intervention remains a rare event in the western hemisphere and expanding the library of aortic reconstructions, and the experience is particularly important for improvement in decision-making, surgical techniques, and outcomes. Surgery is recommended for incapacitating symptoms during the late or chronic phase of the disease. In the two cases described in this article, in situ reconstruction demonstrated to be effective in treating severe claudication and durable with a mean follow-up of 63 months17.
Antiphospholipid syndrome
The APS as aforementioned is an autoimmune disease characterized by hypercoagulable state, leading to thrombosis in the venous and arterial circulation1-4. This disorder is associated with the presence of the lupus anticoagulants in plasma anticardiolipin antibody of immunoglobulin (Ig) G and/or IgM and anti-b-2-glycoprotein 1 antibodies2. The revised classification criteria from 2006 emphasized that the presence of specific antibodies and a persistent elevation for more than 12 weeks of high titers of autoantibodies detected by the enzyme-linked immunosorbent assay and by the lupus anticoagulant assay is necessary for the diagnosis.9 This typically affects young individuals, and with more frequency the female gender with autoimmune diseases (e.g., SLE), and should be suspected in women with a history of repeated abortions and/or venous and arterial thrombosis6. APS can be primary in the absence of any other related disease (autoimmune or connective tissue disorders) or secondary in the presence of autoimmune diseases such as SLE6. The deep veins of the lower limbs are the most commonly affected sites7,8; on the other hand, the incidence of primary arterial involvement is unknown because no literature has differentiated between thromboembolic disease from the presence of underlying atherosclerotic disease in this particular group of patients9. According to the literature reports, the most affected arteries are the coronary circulation followed by the visceral vessel district, renal, retinal, and peripheral arteries2, there are only five cases of aortic thrombosis reported in patients with APS10.
APS associated with limb or organ ischemia is rarely encountered and recognized in a vascular surgery practice, and little has been written regarding its therapeutic approach and clinical outcomes12. The INCMNSZ also receives and treats a large number of patients with prothrombotic12-14.
Limb loss in patients with APS represents another devastating complication. Despite the technical success, the risk of recurrent thrombosis, thromboembolic events, restenosis of vessels, graft failure, and progression of the disease in these patients remains high even on optimal anticoagulation and commonly results in a high rate of limb loss in this relatively young population15. Although some authors state that an optimal anticoagulation postoperatively has shown to maintain a lower incidence in thrombosis recurrence which has led to the recommendation of lifelong anticoagulation therapy with an international normalized ratio (INR) target of 3.015, following arterial reconstructions, we have maintained an aggressive anticoagulation regime with an INR target range from 3.0 to 3.5 and antiplatelet therapy, and patients are clinically followed closely and monitored for possible hemorrhagic complications. With respect to the conduits, we agree with Lauvao et al. in the recommendation of the use of autogenous grafts when possible and a strict perioperative and long-term anticoagulation to prevent graft failure16.
Recognized limitations of the studies in our country include the small cohort of patients and its retrospective nature, thus further clinical experience and recognition of the association of APS to vascular events (arterial and venous) and long-term follow-up are critical for understanding the natural course and establish the appropriate post-operative management and long-term follow-up.
The APS is a prothrombotic disorder that may lead to arterial involvement with less frequency than the venous circulation but has significant morbidity and limb loss rate. Arterial surgical reconstruction seems to be feasible in an attempt to salvage limbs and organs; however, further experience and research are necessary to establish the optimal anticoagulation regime and long-term management following surgical interventions.
Conclusion
Arterial involvement in rheumatological disorders is rare, but when clinically present, its management may be complex. The experience has demonstrated that the open and endovascular approaches are effective in select clinical scenarios. Further, research including clinical trials when possible is necessary to better define the optimal approach.











 text new page (beta)
text new page (beta)


