Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Medicina y ética
versão On-line ISSN 2594-2166versão impressa ISSN 0188-5022
Med. ética vol.33 no.4 Ciudad de México Out./Dez. 2022 Epub 31-Jul-2023
https://doi.org/10.36105/mye.2022v33n4.05
Article
Lex Artis in Ophthalmology, Ethical and Bioethical Analysis
* Instituto de Oftalmología FAP Conde de Valenciana, IAP, CDMX, México. Correo electrónico: dra.claudiaarellano@gmail.com Autor de correspondencia.
** Asociación de Oftalmología y Salud Visual, CDMX, México. Correo electrónico: fernandampalomo@gmail.com Autor de correspondencia.
*** Instituto de Oftalmología FAP Conde de Valenciana, IAP, CDMX, México. Correo electrónico: dr.rene.davila@hotmail.com
**** Instituto de Oftalmología FAP Conde de Valenciana, IAP, CDMX, México. Correo electrónico: docpaulin@hotmail.com
***** Instituto de Oftalmología FAP Conde de Valenciana, IAP, CDMX, México. Correo electrónico: cnv@outlook.com
****** Instituto de Oftalmología FAP Conde de Valenciana, IAP, CDMX, México. Correo electrónico: udediosc@hotmail.com
******* Instituto de Oftalmología FAP Conde de Valenciana IAP, CDMX, México. Correo electrónico: jaime.rosales92@hotmail.com
******** Universidad Anáhuac México, CDMX, México. Correo electrónico: jane.nemer@gmail.com
********* Universidad Anáhuac México, CDMX, México. Correo electrónico: gonzalezrcamila7@gmail.com
People dedicated to providing health services have the legal, ethical, professional and human commitment to ensure the health and welfare of society. A physician must not only be trained in the academic and technical field, but must also build and work on his or her professional ethics. Continuous medical updating in evidence-based medicine and continuous training in the practical and clinical area, although of utmost importance, must go hand in hand with the application of ethical principles such as respect for autonomy, beneficence, non-maleficence to the patient and justice. The analysis of real clinical cases in the light of ethics is a very enriching exercise to transcend in our daily practice. It is not only of great help to detect and prevent behaviors that could violate or attempt against the dignity of patients, but also to reaffirm the value and centrality of the human person in the medical approach.
Keywords: medical act; deontology; deontological principles; glaucoma; cataract
Las personas dedicadas a otorgar servicios de la salud tienen el compromiso legal, ético, profesional y humano de velar por la salud y el bienestar de la sociedad. Un médico no sólo debe formarse en el ámbito académico y técnico, también debe construir y trabajar en su ética profesional. La actualización médica continua en medicina basada en evidencia y el continuo adiestramiento en el área práctica y clínica, si bien son de suma importancia, deben ir de la mano con la aplicación de los principios éticos tales como el respeto por la autonomía, la beneficencia, no maleficencia al paciente y la justicia. El análisis de casos clínicos reales a la luz de la ética es un ejercicio muy enriquecedor para trascender en nuestra práctica diaria. No solamente es de gran ayuda para detectar y prevenir conductas que pudieran vulnerar o atentar contra la dignidad de los pacientes, sino para reafirmar el valor y la centralidad de la persona humana en el abordaje médico.
Palabras clave: acto médico; deontología; principialismo; glaucoma; catarata
1. Medical act, ethics, medical ethics, bioethics
In order to carry out an accurate analysis of real clinical cases, it is necessary to know the precise definitions that will guide and contextualize the reader during this analysis. For this reason, we present the definition of the concepts “medical act”, “ethics”, “medical ethics” and “bioethics”.
The “medical act” is defined as:
A set of actions ranging from a simple diagnosis to the most complex surgical intervention, and which carries a load of risks, to the extent that it is not possible to count on concrete and objective elements that allow giving an exact result (1).
The medical act is considered correct when it is performed under certain premises, such as responding to a medical indication, applying the correct technique, that the health professional is trained in that area, that his actions and decisions are lawful and under the light of an ethical conduct (2). The four pillars of this act are prevention (avoiding the acquisition of a disease and timely detection of risk factors), cure (diagnosis and timely treatment of diseases to prevent their progression), rehabilitation (limiting the damage caused and correcting or avoiding disability) and, finally, palliation (comprehensive care to preserve the quality of life).
Ethics comes from the Greek ethos “custom” and the suffix ica “belonging to”. It is a philosophical discipline that aims to study, understand, reflect and criticize the moral phenomenon and morality. Ethics has several areas of study, among which medical ethics stands out.
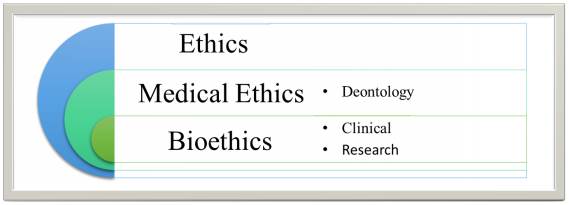
In this sense, medical ethics is a discipline dedicated to the study of the correct behavior of health professionals. In other words, they are norms and principles that guide the work of health care personnel (3). Medical ethics is closely related to bioethics, an area of this philosophical discipline that focuses on the study of human behavior, specifically in the life and health sciences in the light of ethical values and principles. As can be seen in Figure 1, it is important to differentiate one from the other, because while medical ethics deals fundamentally with problems raised by the practice of medicine, bioethics addresses moral problems arising from advances in the biological sciences in a more general way (4).
The latter, bioethics, which provides the necessary tools to carry out a critical analysis of specific clinical cases based on casuistry, will therefore be of particular importance in this article. Now, it seems necessary to introduce the background of bioethics.
Currently, we find many definitions of bioethics. At first, it was defined as “The relationship between the ethics of the relations of human beings with animals and nature”, although nowadays it has been taken to a more humane sense.
According to the National Bioethics Commission, bioethics is defined as:
The branch of applied ethics that reflects, deliberates and makes normative and public policy approaches to regulate and resolve conflicts in social life, especially in the life sciences, as well as in medical practice and research that affect life on the planet, both now and in future generations (5).
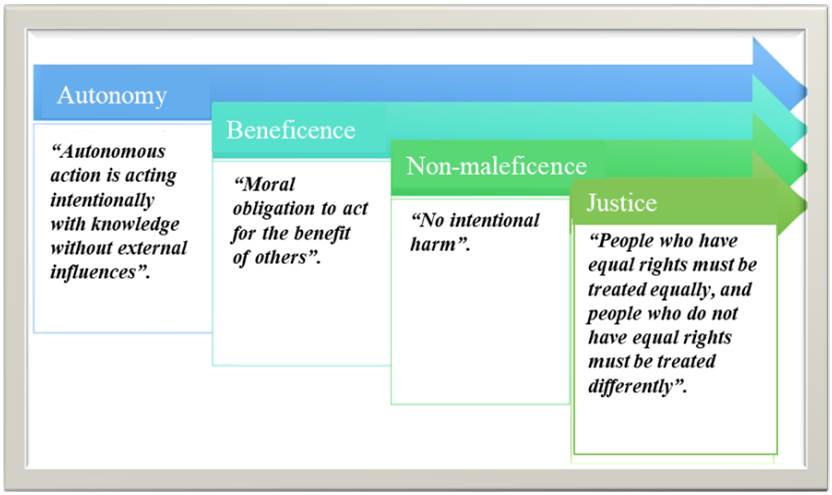
The focus of attention in this definition is, from our perspective, on human conduct in the health sciences, in the light of the values and principles of the principlist current. Principlism has its antecedents in 1979, with T. Beauchamp and James F. Childress, who based themselves on the Belmont report to create the work entitled: Principles of Biomedical Ethics; where in addition to setting out the 4 principlist principles (autonomy, beneficence, non-maleficence and justice, as shown in Figure 2), they reformulated the bioethical principles established in that report so that they could be applied in the clinic (6).
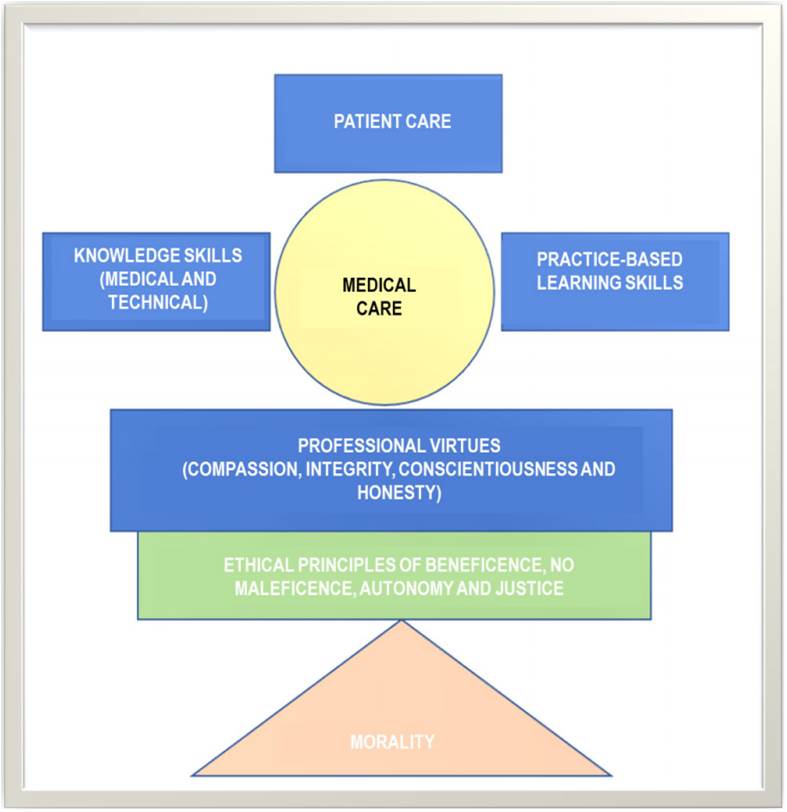
The aforementioned background and definitions form the structure of correct medical practice. In this profession, not only technical knowledge and skills are required, but also ethical training and continuous development of professional virtues.
The author Basil Varkey in his article entitled: Principles of Clinical Ethics and Their Application to Practice proposes the following Patient Care Model, which includes the four main principles (7). We present it below (Figure 3) and we feel it is important to do so since, on occasions; the biological part is separated from the human part of the treatment of patients, thus losing the integrity of medical care with a broad sense of what the human being and its different dimensions are.
2. Lex Artis in ophthalmology
After having defined the concepts under which this article is developed, the application of this knowledge in the different medical specialties is of vital importance. In fact, we will focus on ophthalmology. The critical incident that generated our interest in analyzing this was an extraordinary case in which medical ethics and bioethics were a turning point for this case to have a favorable or less harmful outcome.
Ophthalmology is a medical-surgical specialty dedicated exclusively to the study, diagnosis and treatment of diseases of the eye, orbit, eyelids and adnexa.
As in other medical specialties, the practice of ophthalmology is governed by the principle of Lex Artis, defined as:
the set of rules and knowledge generated for the practice of a medical specialty about techniques and procedures that have been universally accepted, which are based on scientific and ethical principles that guide medical practice (8).
This specialty is distinguished from the others because it has great technological advances that are continually evolving. However, the use of such complex technology requires a great deal of knowledge and management, both theoretical and practical. Nowadays, technology, training and the constant evolution of the tools in this area, have made it possible to perform microsurgeries with minimum hospitalization periods. Even outpatient stay; to perform intraocular lens cleaning without the need of surgical intervention, but by means of yag laser (procedure that can be performed in the office), among many other methods that are not risk-free, but that are very benevolent in trained hands.
3. Case report
Below (Figure 4 and 5), we present a case report from the specialty of ophthalmology, which will be analyzed, discussed and reflected upon in the following section, under the threshold of the medical act; its resolution by the medical team and the ethical values involved in this scenario are likewise appended.
A female patient came for ophthalmologic consultation with low visual acuity and bilateral ocular pain of 15 days of evolution after the application of yag laser.1
During the interrogation, the patient refers to a history of cataract surgery with intraocular lens implantation in both eyes 16 years ago due to a diagnosis of congenital cataract. She mentions that she presented a decrease in visual acuity, so she went to see a private physician who indicated the application of yag laser for intraocular lens cleaning. The patient comments that she is being treated with dorzolamide 2%, brimonidine 0.15-0.2% and timolol 0.1-0.25-0.5% 1 drop every 12 hours in both eyes.2
On physical examination, the right eye had a visual acuity of finger count at 30 c.m. and an intraocular pressure of 27 mmHg, the left eye the same visual acuity with an intraocular pressure of 20 mmHg.
In both eyes, upon biomicroscopic examination, 3+3 cellularity and hydrated crystalline lens were observed. Specifically, in the left eye, iridotomy in M XI4 was observed. Drugs were applied to dilate the pupil and to have a better vision of the fundus. In both eyes, there was a loss of central continuity of the anterior lens capsule, abundant opaque and hydrated crystalline debris and an apparent rupture of the posterior capsule. In order to confirm the posterior capsule rupture, an A and B mode ultrasound of both eyes was requested; in addition to confirming the clinical suspicion, crystalline debris was identified in the posterior segment.
The physical examination and questioning made the ophthalmology team question whether the surgery to remove the congenital cataract had actually been performed, since the remains of the crystalline lens, part of the eye that had previously been removed, were observed.
Briefly, this patient’s pathologic condition was triggered by the application of yag laser on an intact crystalline lens. The application of the laser resulted in the rupture of this natural lens causing the fragments to obstruct the iridocorneal angle, 5 thus generating an increase in aqueous humor that culminated in an increase in intraocular pressure leading to damage to the nerve fibers that are responsible for transmitting the image to our brain, this is known as glaucoma (Figure 6).
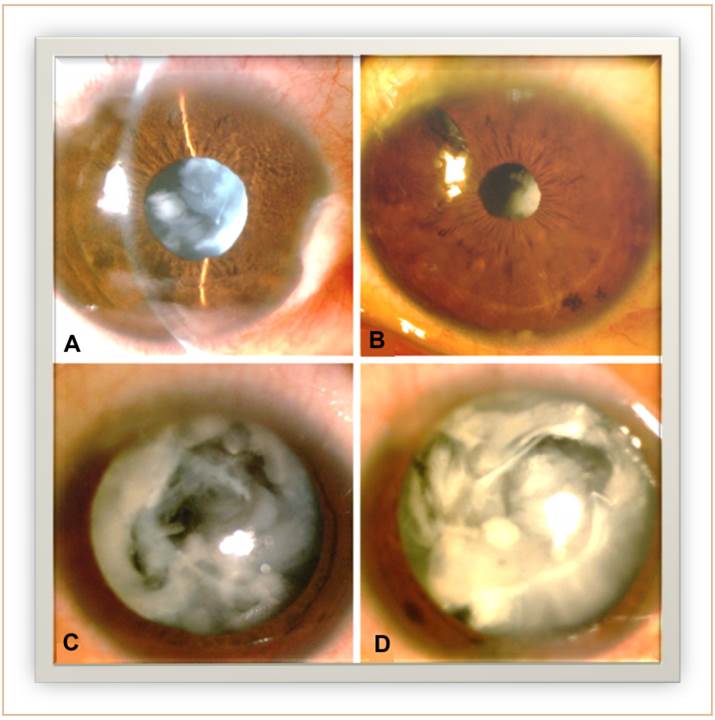
Source: prepared by the authors.
(A) Slit-lamp bio microscopy image of the right eye without pharmacologic dilation showing anterior chamber with cellularity, intact iris with hydrated lens.
(B) Slit-lamp bio microscopy image of the left eye without pharmacologic dilation showing anterior chamber cellularity, iris with iridology at the meridian of M XI and hydrated lens.
(C) Slit-lamp bio microscopy image of the left eye under pharmacologic dilation demonstrates loss of central continuity of the anterior capsule, opaque and hydrated crystalline debris and apparent rupture of the anterior capsule.
(D) Slit-lamp bio microscopy image of the right eye under pharmacologic dilation demonstrates loss of central continuity of the anterior capsule, opaque and hydrated crystalline debris and apparent rupture of the anterior capsule.
Figure 6 Images of the clinical case.
After medical evaluation, the ophthalmologists decided to perform surgery on the right eye due to posterior capsule rupture and the presence of crystalline debris in the vitreous cavity. A pars plana lensectomy, vitrectomy, and placement of an intraocular lens in the sulcus were performed. The patient did not present perioperative complications. In the postoperative period, antibiotic/anti-inflammatory treatment (gatifloxacin 0.3%/prednisolone 1% 1 drop every 4 hours) and cycloplegic treatment (tropicamide-phenylephrine 8 mg/50mg/ml 1 drop every 8 hours) were indicated. 24 hours after surgery, the patient presented visual acuity of 20/100 and intraocular pressure of 16 mmHg. Biomicroscopy revealed slight corneal edema, formed anterior chamber, 2+ cellularity, and centered intraocular lens.
The favorable results of this first intervention led to perform the same procedure in the left eye. After 24 hours, the patient presented visual acuity 20/80 and intraocular pressure of 16 mmHg. Biomicroscopy showed a clear cornea, anterior chamber formed with 2+ cellularity and centered lens.
On postoperative follow-up examination, the right eye had a best corrected visual acuity of 20/40 and an intraocular pressure of 16 mmHg, in the left eye a best corrected acuity of 20/30 with an intraocular pressure of 15 mmHg. In both eyes a 3-piece intraocular lens in sulcus was observed.
4. Bioethical analysis
This clinical case represented a complex challenge for the team of ophthalmologists who followed up the case. It is not only interesting, illustrative and fruitful in the clinical setting, but also in the area of bioethics.
However, a complete bioethical analysis must have a multidimensional vision of the person, as well as an inter and transdisciplinary approach. This is why the analysis is essentially made up of the medical indications (medical data, diagnosis and lines of treatment), the patient’s preferences (who is our patient?), his or her quality of life and life expectancy, and finally, contextual aspects (religion, interests, economic scope, among others).
In the following, we will focus solely on an analysis based on the principled principles involved in this particular case and their relevance to medical action.
a. Autonomy
Autonomy is a fundamental principle and right and is defined as the free action of an individual. Physicians have the moral and legal responsibility to provide patients with truthful information so that they can make a decision in accordance with their needs, interests and values.
In order for a person to responsibly exercise his or her autonomy in the medical field, he or she must have clear, truthful, prudent and timely information about his or her diagnosis. They must also have the capacity to make a decision, i.e., they must have the skills to be able to know, evaluate and manage information; and finally, they must be legally competent.
The tool that health professionals use to protect and respect patient autonomy is informed consent. A process guarantees respect for the patient’s dignity and autonomy in the face of a clinical or surgical approach. It is also a legal medical document legislated by the regulations of the General Health Law on the Provision of Health Care Services and by nom-004 of the Clinical Record, which protects both the patient and the physician. This document must contain the diagnosis (health problem presented by the patient), risks and benefits of the medical intervention, treatment alternatives and prognosis, essentially.
In ophthalmology, it is especially difficult to explain to patients the pathophysiology of diseases and treatments, especially surgical approaches. However, this does not exempt ophthalmologists from making sure that patients clearly understand the information being presented. It is not a matter of making the patient a medical expert. The key is to inform in understandable terms, use visual aids such as videos, anatomical models, drawings or analogies, and give the patient a forum for questions and feedback.
In the aforementioned case, the patient did not have accurate knowledge about her diagnoses and previous approaches. This would have been important for the first contact team to better manage the information so that the patient could make informed and free decisions; likewise, with accurate information, it would probably have been possible to avoid performing a yag laser on an intact lens.
b. Beneficence and non-maleficence
The purpose of the medical act is to ensure the health and well-being of individuals. When physicians offer an intervention, it must provide benefits to the patient; although not in its entirety, these must outweigh the risks involved in the procedure.
These two principles go hand in hand, because while non-maleficence protects the maxim Primum non nocere (above all, do no harm) embodied in the Hippocratic oath, beneficence is, quite simply, always acting in the best interest of the patient and choosing the approach that entails risks that do not outweigh the benefit of the procedure.
We must also take into account the principle of double effect, especially implied in the principle of non-maleficence. This is based on the duality between favorable and unfavorable effects, but allows us to make a decision as physicians when choosing a therapeutic option, always seeking the greatest benefit for patients.
When we practice a health profession, we not only need to have a theoretical mastery with information based on scientific evidence and constant updating, we must also have the practical knowledge and the necessary skills to perform manual procedures. Faced with these crucial needs of the medical act, health personnel must know what their capabilities are and know how to recognize their limitations, precisely in order to take care of these principles. It is completely valid that certain situations get out of our hands and we need to ask for support. This reflects our respect for the patient and our aim to look after his or her well-being.
In ophthalmology, as in any medical specialty, one must have an impeccable professional preparation. Physical examination is a challenge at the beginning of the specialty, since it requires a great deal of skill to use ophthalmologic examination equipment such as lamps or lenses that allow visualization and evaluation of microscopic structures. In addition to theoretical knowledge, ophthalmologists must have theoretical and practical skills when performing surgical interventions, since we are talking about microsurgeries in which there is a very small margin of error with very severe complications.
In the case we are dealing with, it is a lesson that the physician must have impeccable clinical and theoretical knowledge to perform an adequate approach. Particularly with this patient, it would have been a point of good practice to perform a complete ophthalmologic review prior to the application of the yag laser, in order to have observed the integrity of the lens and avoid performing this procedure.
c. Justice
The technology for practices in this specialty is very short range for doctors in training, who require a lot of practice to obtain the necessary skills in the technical application part of their specialty. Many are the rules and principles that govern this stage of medical training, but we must not forget that it is unfair to subject a person to risks and that the rest of society benefits from the results.
When a physician does not have the necessary development to be able to face different clinical scenarios, he/she must be assisted by a professional with the necessary skills and knowledge to guide and be able to act in the event of a mishap.
This principle goes hand in hand with non-maleficence and awareness of limits. It is totally acceptable to recognize when the situation is beyond our capabilities and to ask for help when such cases arise. We must also understand that patients should not be a means in our skill building. It should not be inferred that there must be “sacrifices” or “failures” in order to achieve the required competencies; we cannot harm some people in order to benefit the rest.
As mentioned above, an appropriate course of action in the clinical case could have been the assistance of a more experienced physician to guide the first contact health professional. This would have provided two professional opinions that would substantially reduce an incorrect diagnosis and the repercussions of applying a treatment that was not the treatment of choice in this particular case.
5. Conclusions
Ethics is inherently part of clinical medicine. Health professionals must know how to make decisions. These decisions are not only clinical, for example, therapeutic decisions based on information obtained by the scientific method and with significant evidence values. We must also know how to make ethical decisions. On the one hand, we must opt for those courses of action that safeguard the autonomy, beneficence, non-maleficence and justice of patients along with their needs, beliefs and values. On the other hand, as humans, we must know how to make the decision of when to stop and ask for support, by the latter we mean to be physicians of integrity; when we refer to a person of integrity, we are talking about someone who has the prudence to make correct judgments.
In order for the patient to be certain of our actions and the treatment options offered, we must be clear, truthful and prudent when transmitting information. We should not use technical terms or medical language that is difficult to understand, but neither should we fall into simplicity; it is also a virtue of the physician to learn to balance the information so that the patients understand it. Patients have the right to know and understand not only because of their autonomy, but also because information is power, and a patient who is educated about his or her disease can give the physicians who attend him or her in other scenarios the tools to make an accurate diagnosis and offer the best treatment.
It is essential for us to be a trustworthy figure for patients. We must get them to ask us questions or share their concerns with us, because that is how we will get these people to make a free and responsible decision. The pillars in the medical act that reflect respect for the patient’s dignity are respect for autonomy, truth and confidentiality.
Patients should always be seen as an individual and valuable person, not as just another patient. Human dignity should be respected in medical practice, in the understanding that, generically, dignity refers to the respectful treatment that should be given to people because of their condition as human beings.
Vulnerability is a fundamental condition in the maturation process of human autonomy(9), this quality should not be seen as something negative, but should rather serve as a call to the practice of solidarity and humanism to protect and help people who are more susceptible to suffering some kind of harm.
We know that explaining the physiological, pathological and surgical principles of ophthalmology is quite complex. We believe that this work could not only serve as a didactic writing for medical specialists in training to know how to deal with complex ophthalmologic cases. This work could also serve as a clinical and ethical background to design communication techniques with patients in the ophthalmology service and make it easy for both the physician and the patient to have an adequate transmission and reception of information. This area of opportunity would ensure the highest ethical standards in medicine. It would not only benefit patients in their right to understand and know, but it would also be a benefit for physicians since the patient would provide the necessary information so that the physician who comes to treat him/her has enough tools to make a more adequate diagnosis and, therefore, provide the best therapeutic approach.
Respect for human life, the dignity of the person and health care should be our compass in the medical act. There is a moral duty of health professionals not to abandon patients. The negative consequences of decisions made must be assumed and patients must be offered clear, constructive and prudent information about the error along with solutions.
There are other specialties in medicine in which bioethics is more clearly and commonly seen; however, this article is intended to show readers that this branch of ethics is present in any area belonging to the health sciences, including ophthalmology. We believe it is essential to disseminate the importance of analyzing clinical cases, such as the one presented in this paper, from a multidimensional perspective, thus including bioethics.
REFERENCES
1. Orrego E. Mal Praxis Médica. Acta Cancerológica. 2002. [ Links ]
2. Fernández SB. El acto médico: error y mal praxis. Boletín CONAMED-OPS, 2016 mar-abr 2016; (5):3-6. [ Links ]
3. Manual de Ética Médica. World Medical Association. CONAMED-OPS. 2018. p. 1-4. [ Links ]
4. Farías E, Hall RT. Bioética clínica: una breve introducción. CONBIOÉTICA. 2020; (1)8-83. [ Links ]
5. Guía Nacional para la integración y el funcionamiento de los Comités Hospitalarios de Bioética. Secretaría de Salud/Comisión Nacional de Bioética. 2015; (5)9-17. [ Links ]
6. Busquets E. Principios de Ética Biomédica, de Tom L. Beauchamp y James F. Childress. Camps V, Carrera J, Feito L, editors. Bioética & Debat. 64th ed. Barcelona: Institut Borja de Bioética, 2011. p. 2-19. [ Links ]
7. Varkey B. Principles of Clinical Ethics and Their Application to Practice. Vol. 30, Medical Principles and Practice. S. Karger AG. 2021. p. 17-28. [ Links ]
8. Lex Artis Ad Hoc, Especialidad de Oftalmología. Vol. 1, Consejo Mexicano de Oftalmología. México: CONACEM; 2019. p. 9-14. [ Links ]
9. ten Have H. Vulnerability: challenging bioethics. Abingdon, Oxon; New York: Routledge. 2016. [ Links ]
10. Glaucoma. Consejo General de Colegios Farmacéuticos. 2020. p. 4-13. [ Links ]
1The yag laser, among its multiple uses, consists in the application of laser on the crystalline lens when it is opacified after cataract surgery.
3The 3+ is the objective manifestation of inflammation characterized by floating cells observable in the anterior chamber.
4In ophthalmology, the meridian system is used, as in clocks, as a universal language for describing lesions.
Received: April 10, 2022; Accepted: July 12, 2022











 texto em
texto em