Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Medicina y ética
versão On-line ISSN 2594-2166versão impressa ISSN 0188-5022
Med. ética vol.32 no.1 Ciudad de México Jan./Mar. 2021 Epub 14-Ago-2023
https://doi.org/10.36105/mye.2021v32n1.03
Artícles
Proposal of an action guide to coordinate the last visits of relatives during the «last days life» of a Covid-19 patient in Mexico
* Departamento de Anestesiología y Comité de Bioética del Hospital General Regional No. 12, Lic. Benito Juárez, del IMSS, Mérida, Yucatán, México. Correo electrónico: rapavons@gmail.com
** Departamento de Educación e Investigación del Centro Algia para la Educación en Salud, Ciudad de México, México.
*** Coordinación Clínica de Medicina Interna del Hospital General Regional No. 12, Lic. Benito Juárez, del IMSS, Mérida, Yucatán, México.
**** Departamento de Educación e Investigación del Centro Algia para la Educación en Salud, Ciudad de México, México.
***** Departamento de Educación e Investigación del Centro Algia para la Educación en Salud, Ciudad de México, México.
****** Departamento de Educación e Investigación del Centro Algia para la Educación en Salud, Ciudad de México, México.
******* División de Cuidados Paliativos y Clínica del Dolor del Hospital General Dr. Manuel Gea González, Ciudad de México, México.
******** División de Cuidados Paliativos y Clínica del Dolor del Hospital General Dr. Manuel Gea González, Ciudad de México, México.
********* Programa «Médico a Domicilio» del Ayuntamiento de la ciudad de Mérida, Yucatán, México.
In December 2019, a new, potentially fatal acute respiratory illness caused by a coronavirus was described in Wuhan Province in China. This disease was called Covid-19. In Mexico, mortality from this disease is high and a significant percentage of patients die in hospitals.
For now, there is no specific protocol in Mexico’s public and private health system for families to say goodbye to patients with Covid-19. A panel of experts in palliative care and bioethics proposes one, so that it could serve as a reference in every health unit in our country.
Keywords: palliative; last days; Covid-19; agony; hospital
En diciembre del 2019, en la provincia de Wuhan, China, se describió una nueva enfermedad respiratoria, aguda y potencialmente letal, causada por un coronavirus. A esta enfermedad se le denominó Covid-19. En México, la mortalidad por esta enfermedad es elevada y un porcentaje importante de los enfemos muere en los hospitales.
Por ahora no existe en México un protocolo específico en el sistema de salud tanto público como privado, para que las familias puedan decirle adiós a los enfermos con Covid-19. Un panel de expertos en cuidados paliativos y bioética proponen uno, para que pueda servir como referencia en cada unidad de salud de nuestro país.
Palabras clave: paliativo; últimos días; Covid-19; agonía; hospital
Introduction
In December 2019, in Wuhan Province, China, a number of people were reported to have an acute atypical respiratory disease. The cases presented in that location spread to neighboring towns and, later, to the entire world. Over the months, it was discovered that a coronavirus was responsible for the disease, which was called «Severe Acute Respiratory Syndrome CoronaVirus-2» [SARS-CoV-2, 2019nCoV] (1).
It was given that name because of its morphological similarity (almost 80% homogeneity) with the SARS-CoV virus that was responsible for the «Acute Respiratory Distress Syndrome, [ARDS]» (2). The disease caused by this coronavirus was called Covid-19 (Corona-Virus-Disease, and is number 19 for the year in which the outbreak occurred). As the disease rapidly spread to more than 200 countries and territories with high mortality, the World Health Organization considered classifying the disease as a pandemic on March 11, 2020 (1).
With infectious diseases (such as that produced by SARS-CoV-2) it is important to consider their severity and capacity to produce death. Mortality rates help us understand the severity of a disease, identify populations at risk, and assess the quality of medical care (3).
Two parameters are used to evaluate the proportion of infected persons with a fatal outcome: a) The first is the infection fatality rate (IFR), which estimates this proportion of deaths among all infected individuals; b) the second is the case fatality rate (CFR), which estimates this proportion of deaths among identified confirmed cases. In the case of Covid-19, the IFR cannot be measured accurately because of the time the disease has been on the planet. On the other hand, the CFR in this disease presents a great variability by country, from less than 0.1% to more than 25% (3).
In Mexico, up to October 20, 2020, more than 86,000 deaths have been recorded and more than 1.1 million deaths worldwide. Our country ranks first in deaths per inhabitant worldwide (with a rate of 10.6%) (4). Under this frame of reference, it is worth considering that many people will die under a protocol of isolation that will have an impact on the accompaniment at the end of life.
1. End-of-life accompaniment protocols
In Latin America, especially in Mexico, the family bond is strong. In this context, it is important for members of a Latin community to say goodbye to the family member who is on his or her deathbed. In this social framework, funeral rituals or death ceremonies are considered a fundamental element of the family dynamic. Over time, surviving members will remember the deceased family member every year. In Mexico, this occurs in the month of November, on the Saints day and Souls day, and these rites are part of the Mexican tradition of honoring the dead.
In international literature, there are «farewell protocols» (5, 6). In Mexico, the «Operational Manual of the Course for the Accompaniment of Mourning in Special Situations during the Covid-19 Pandemic in Mexico» has been published (7). Although it has a meritorious creation, it presents a psycho-affective and non-operational approach.
2. The creation of a farewell protocol at the end of life
To fill the lack of goodbye protocols, a team of experts proposed a «protocol for saying goodbye to the sick». The motivation for such a protocol is due to the importance of saying goodbye to a sick relative, since such an action has a profound impact on the emotional dimension of any person. Goodbyes allow one to close circles or life cycles. However, the Covid-19 pandemic has limited the possibility for sick people and their families to say their «last goodbye», since the high rate of person-to-person transmission limits a «goodbye or formal closure».
Various disciplines are concerned with the importance of providing accompaniment and adequate conditions of death to the sick in their final days. Among them is bioethics, whose principles of charity and solidarity have accompanied palliative care in this pandemic. Not to leave alone the one who is going to die is a humanitarian measure, since every sick person has the right to die accompanied.
Consequently, the importance of having protocols for final accompaniment in this pandemic protects the right of the sick person to die accompanied, and should consider reducing the risk of contagion in the family. Having a clear and functional protocol may lessen the pathological mourning of the family, given the certainty that the patient had adequate conditions of death (dignified death).
In Mexico, the legislation has evolved in a favorable way for the attention of people with a palliative disease in a terminal situation. Such legislative evolution makes palliative care and the accompaniment of a person in a terminal state obligatory.
The «international recommendations for palliative care for patients at the end of life with Covid-19» involve the process of dismissal (8). This includes the following actions: a) doctor-patient communication; b) remote doctor-family communication; c) palliative care in patients with severe Covid-19; and d) spiritual care, psychosocial care, and bereavement care.
These practices are valued positively by patients and their families, who, when describing the care received, emphasize «warmth in treatment», «affection», «concern», and «containment», among other expressions. These actions are part of the so-called «humanization of medicine» (9).
3. Objective of the farewell protocol at the end of life
This article aims to suggest a proposal for a protocol so that a companion has the opportunity to say goodbye to the dying relative with Covid-19 and do so safely.
4. Selection of cases to include families in the end of life farewell protocol
To apply by mutual agreement the farewell protocol by the committee, the hospital’s palliative care team or the treating physician. The scales of terminality and/or need for palliative care (SOFA, APACHE, SPICT, NECPAL), Criteria for Terminality of the Official Journal of the Federation NOM 2014-2018 in Palliative Care and Mentem Scale) will be applied to determine if the patient is in agony.
Agony, as defined by the Spanish Society of Palliative Care (SECPAL), is the final stage of the terminal illness that is marked by a very significant deterioration in the general state, and indicates a potential imminent death (within hours or a few days) (10). When, according to the appropriate scales, it is determined that the patient is in agony, the companion of the patient who has requested it (as long as he or she is not a high-risk person) and after giving consent, may initiate the protocol (11).
5. Development of the farewell protocols at the end of life
a) Face-to-face farewell protocol
In order to protect and safeguard the life and health of the companions at the time the farewell protocol is activated, the following points should be considered:
1. There will be no more than one person involved in the process of saying goodbye to the patient.
2. If the patient’s cognitive capacity is still intact, he or she may designate the person who will accompany him or her in his or her farewell (trying to determine if this is possible from the moment of admission with Social Work). If this last point is not possible, it will have to be based on a family consensus and to inform Social Work. The person selected must be of legal age, not at high risk or vulnerable. In addition, you must know that you are not a carrier of Covid-19. He/she should not have the criteria of the operational definition of «suspected case of Viral Respiratory Disease (VRE), which includes Covid-19», as it appears in the last update in the website of the National Institute of Public Health of Mexico. It is the person of any age who in the last 10 days has presented at least one of the following major symptoms: cough, fever, difficulty in breathing, headache accompanied by muscular pain, joint pain, sore throat, runny nose, conjunctivitis and chest pain (12).
3. Corroborate if the patient has an advance directive (13).
4. When the medical personnel determine the imminent death of the patient, the designated companion will be notified by telephone by the social work personnel, and will carry out the protocol of accompaniment and dismissal. It is suggested that, in the event that the patient is intubated, this protocol should not be considered, due to the high emission of aerosols from the ventilator. It will be preferable to say goodbye by means of a smartphone.
- Before contact:
1. The designated person should be trained by the health team on the generalities of the Covid-19, the technique of hand washing and the technique of dressing and removing personal protective equipment (PPE). In addition, she should follow the informed consent process: after explaining the implications of participating in the protocol and once understood by the participant, she will sign the informed consent document.
2. The participant’s belongings will be temporarily safe guarded by Social Work. Participants will be asked not to carry personal objects that could be fomites (lifeless objects that could carry a pathogen on their surface), and to have their nails trimmed, clean and unpolished.
3. The designated person must follow at all times the process of hygiene and prevention of infection of Covid-19, established by the authorities of each hospital or health institution.
4. The designated companion must be provided with the EPP for the areas where patients with Covid-19 are cared for, as determined by each institution, and the change of EPP if necessary.
5. The person designated for the dismissal process must always be accompanied by institutional personnel (nurse or doctor), for emotional support and for travel in the health facilities.
- In the process of saying goodbye:
1. Explain to the companion how much time he or she will have for the farewell and that, in case of leaving the patient’s room, he or she will not be able to return. Each hospital institution will previously designate the time.
2. The designated person will be able to talk to the patient and have physical contact with him/her, using disposable gloves (hands must be washed with soap or an alcohol-based solution of at least 70%).
3. No personal objects may be removed from the patient or that were previously in the Covid-19 patient care area.
- Term of the dismissal:
1. Direct the companion to the EPP removal area, and monitor the removal of the patient, based on the protocols of each institution, in addition to following the process of disinfection, hand hygiene and change of clothes.
2. The entire protocol process must be recorded with the names of the participants.
3. When the patient dies, the family will be notified, following the same process that is followed with all other patients.
b) Farewell protocol with photograph for intubated patients (Figure 1)

The figure shows a model through which the disease process is explained and the measures that are taken by health personnel to improve the conditions associated with the life of a person with Covid-19 and the process of intubation.
Figure 1 Example of model for description and preparation of farewell by photographs.
1. Preferably, this protocol will be done by the team psychologist.
2. A photograph of the patient will be requested, with the authorization of the treating physician and the request of the family members. This will reflect the contour of the patient, according to the area of the hospital where his or her bed is.
3. Before showing the photograph to the family member, the palliative care team will review what you will see on the image: tubes, catheters, medical equipment, endotracheal tube, in order to minimize the visual impact. The process will be with «healthy distance» from the person who will receive the information, and following the safety measures of the area of the hospital where the patient is.
4. Afterwards, the photograph of the patient will be shown and the doubts about his situation, maneuvers and invasive measures will be answered.
5. The responsible family member will be asked to say goodbye to the patient in a symbolic way, if he or she so wishes: pending issues, last words or thanks. This will favor the expression of the family member’s emotions.
6. A brief emotional containment will be performed by the psychologist, and thus the process ends.
7. Contact numbers for the palliative care area or the treating service will be provided for further questions (14).
c) Farewell letter protocol (Figure 2)
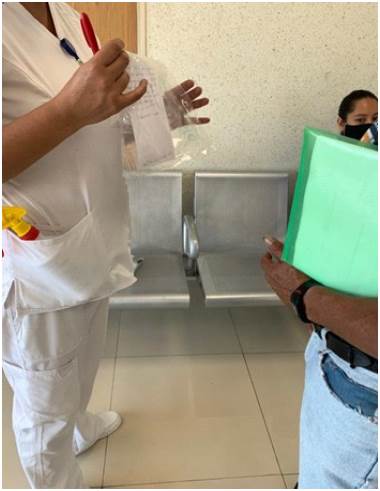
The figure shows how health personnel deliver a letter made by the hospitalized patient to the family in the hospital waiting room.
Figure 2 Farewell letter protocol.
1. With the prior authorization of the treating physician and at there quest of family members, health personnel will be allowed to carry letters to the patient in critical areas: emergencies, internal medicine, intensive care, etcetera.
2. The family member or family members responsible will be asked to prepare one or two letters with free speech, to be read or given to the patient within the Covid area, depending on the conditions of the patient.
3. The responsible family member will be guided to say goodbye to the patient in a symbolic way and ask him/her to write pending issues, last words and thanks to encourage the expression of his/her emotions.
4. Once the family member delivers the letter, it will be put in a plastic bag, which will be heat-sealed and then sanitized (with alcohol, chlorine, water and soap or quaternary ammonia).
5. This letter will be given to the patient’s treating physician or nursing staff on duty to be read to the patient.
6. The family of the person who read the letter will be notified in writing and then notified by telephone of the time and any subsequent reaction of the patient.
7. Contact numbers for the palliative care area or the treating service will be given for further questions (14).
d) Audio release process
1. Upon authorization by the treating physician and at the request of family members, a voice message will be delivered to the patient in critical areas.
2. The responsible family member(s) will prepare an audio message of a maximum duration of three minutes, to be played in front of the patient within the Covid area.
3. The responsible family member will be oriented to say goodbye to the patient in a symbolic way and to express pending issues, last words, gratitude, in order to favor the expression of emotions.
4. Once the family member sends the audio, it is played for the patient by the attending physician or by the nursing staff in charge.
5. The family member will be informed of who played the audio to the patient, the time of the event and if there was any reaction afterwards.
6. Contact numbers for the palliative care area or the treating service will be given for further questions (14).
e) Video call farewell protocol (Figure 3)
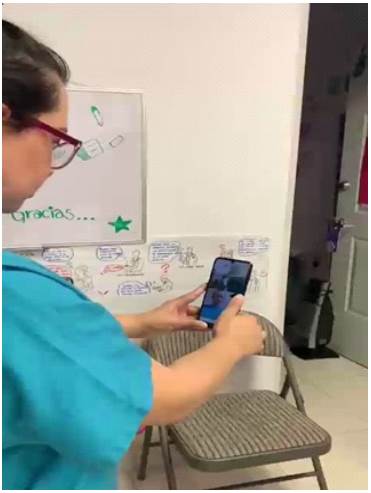
The figure shows a health professional making the video call link. The patient and the family are identified.
Figure 3 Video call farewell protocol.
1. With the previous authorization of the treating physician and at the request of the family members, a video call will be made to the patient who is in critical areas.
2. The patient will be asked for his/her consent to participate in the video call, and the family member or family members who requested it will be told that they will have three minutes to communicate with the patient who is isolated in the Covid area.
3. The patient or the responsible family member will be oriented about the farewell: pending issues, last words, thanks, to favor the expression of their emotions.
4. The medical and/or nursing staff on duty to the patient will direct the video call.
5. Contact numbers of the palliative care area or of the treating service will be given for further questions (14).
6. Epidemiology and other care services
In case that at any moment the established protocol of epidemiological security is violated, the visitor will be considered «case contact» and will be in home isolation for 15 days; the time will vary according to the medical unit where the patient is. The epidemiology service and the Family Medicine Unit will be notified.
It is also convenient that the family member or members receive psychological or thanatological attention, depending on the existing human resources.
Conclusions
Throughout the pandemic we have observed, not only in Mexico but worldwide, that we have to adapt as living beings and learn to live with the SARS-CoV-2 virus, so any protocol related to the care and management of this type of patient during the contingency has been and will continue to be modified. For this reason, the process of saying goodbye to a loved one who is in agony from Covid-19, must also be more «empathic and humanized», so that the patient does not die alone and, above all, so that he can exercise the right to say goodbye to his loved ones, of course, in a safe environment for all involved. The protocol proposed in this article can be adapted to the various levels of care in our health system, both public and private, or where patients with Covid-19 are treated, based on their own care regimes.
Acknowledgements
We thank the Residents of Algology and Palliative Medicine of the General Hospital Dr. Manuel Gea González (Montserrat Díaz, Juan Luis Vega, Lenia Alvarado, Guadalupe Sales), who have collaborated in the realization of the protocols. We also thank our patients and their families.
REFERENCES
1. Yuki K, Fujiogi M, Koutsogiannaki S. Covid-19 pathophysiology: A review. [Consultado el 20 de abril del 2020]. Clin Immunol. 2020; 215: 108427. https://doi.org/10.1016/j.clim.2020.108427 [ Links ]
2. Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003; 348(20): 1953-1966. https://doi.org/10.1056/NEJMoa030781 [ Links ]
3. Organización Mundial de la Salud. Estimating mortality from Covid-19. [Consultado el 4 de agosto de 2020]. Recuperado en: https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19 [ Links ]
4. Johns Hopkins University of Medicine. Covid-19: Mortality analysis. 2020. [Consultado el 01 de septiembre del 2020]. Recuperado en: https://coronavirus.jhu.edu/data/mortality [ Links ]
5. NHS. Clinical guide for supporting compassionate visiting arrangements for those receiving care at the end of life. [Consultado el 1 de septiembre del 2020]. Recuperado en: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0393-clinical-guide-for-supporting-compassionate-visiting-arrangements-11-may-2020.pdf [ Links ]
6. Derecho a morir dignamente. Covid 19: Protocolos para el acompañamiento y la muerte digna. 15 de abril del 2020. [Consultado el 1 de septiembre del 2020]. Recuperado en: https://derechoamorir.org/2020/04/15/covid-19-listado-de-iniciativas-para-facilitar-el-acompanamiento-al-final-de-la-vida/ https://doi.org/10.16925/gcgp.21 [ Links ]
7. Osiris Pazarán RM, Guerrero Uribe GE, Herrera Melo A, Ascencio Huertas L, Rodríguez Lugo ME, Aguilar Salas I, Esquivias Zavala H, Beltrán-Uribe A, Ibarreche-Beltrán J. Manual operativo del curso para el acompañamiento del duelo en situaciones especiales durante la pandemia del Covid-19 en México. 2020. [Consultado el 1 de septiembre del 2020]. Recuperado en: http://inprf.gob.mx/ensenanzanew/archivos/2020/manual_duelo.pdf https://doi.org/10.1016/j.rx.2020.09.006 [ Links ]
8. Janssen DJA, Ekström M, Currow DC, Johnson MJ, Maddocks M, Simonds AK,Tonia T, Marsaa K. Covid-19: Guidance on palliative care from a European Respiratory Society international task force. Eur Respir J. 2020; 56(3): 2002583. https://doi.org/10.1183/13993003.02583-2020 [ Links ]
9. Núñez Cortés JM. Humanización de la medicina, medicina humanizada, medicina humanista: ¿de qué estamos hablando? Ed Méd. 2018; 19(3): 131-132. https://doi.org/10.1016/j.edumed.2018.05.001 [ Links ]
10. Sociedad Española de Cuidados Paliativos. Capítulo 14. Los últimos días: atención a la agonía. s. f. [Consultado el 1 de septiembre del 2020]. Recuperado en: https://www.secpal.com/biblioteca_guia-cuidados-paliativos_14-los-ultimosdias-atencion-a-la-agonia https://doi.org/10.5209/psic.59195 [ Links ]
11. Rubio O, Estella A, Cabre L, Saralegui-Reta I, Martín MC, Zapata L, Esquerda M, Ferrer R, Castellanos A, Trenado J, Amblas J. Ethical recommendations for a difficult decision-making in intensive care units due to the exceptional situation of crisis by the Covid-19 pandemia: A rapid review & consensus of experts. Med Intensiva. 2020; S0210-5691(20): 30110-8. https://doi.org/10.1016/j.medin.2020. 04.006. [ Links ]
12. Instituto Nacional de Salud Pública. Signos, síntomas y prevención (Covid19). 25 de agosto del 2020. [Consultado el 1 de septiembre del 2020]. Recuperado en: https://www.insp.mx/nuevo-coronavirus-2019/signos-sintomas-prevencion.html https://doi.org/10.1590/s1135-57272003000400002 [ Links ]
13. Secretaría de Salud. Voluntad anticipada. s. f. [Consultado el 1 de septiembre del 2020]. Recuperado en: https://www.salud.cdmx.gob.mx/actividades/voluntadanticipada https://doi.org/10.33539/lumen.2015.n11.543 [ Links ]
14. Consuegra Fernández M, Fernández Trujillo A. La soledad de los pacientes con Covid-19 al final de sus vidas. Rev Bioética y Derecho. 2020; 50(nov): 81-98. https://doi.org/10.1344/rbd2020.50.31683 [ Links ]
Received: September 20, 2020; Accepted: October 15, 2020











 texto em
texto em 



