Introduction
Heart transplantation has become the therapeutic intervention of choice for patients with advanced heart failure (HF). Although life expectancy increases considerably after receiving a transplant, survival rates remain inferior to that of healthy individuals. Functional capacity, exercise tolerance and health-related quality of life are significantly reduced in heart transplant patients1. Individualised exercise prescription and assessment of exercise intensity appear to be the most applicable strategy for this group2-5.
Phase I of cardiac rehabilitation and early mobilisation programmes in the cardiac intensive care unit
Phase I of cardiac rehabilitation programmes (CRP) encompasses the patient's period of hospitalisation, which includes a stay in the intensive care unit (ICU), and focuses primarily on reducing functional complications stemming from hospitalisation6. Early mobilisation is one of the cornerstones of Phase I. Early mobilisation is defined as the initiation of active exercise within the first five days following the onset of critical pathology, including those who are new heart transplant recipients7.
The following is a brief description of a patient with chronic heart failure (CHF) who underwent a heart transplant. His clinical scenario and his management by the Cardiology Department and Critical Area Physiotherapy Department, at Hospital General de México "Dr. Eduardo Liceaga", went from the lowest level of functionality in the ICU to an independent discharge to this home.
Clinical case
A 31-year-old male patient with a history of dilated cardiomyopathy (DCM), and a diagnosis of decompensated heart failure (HF) with severely reduced left ventricular ejection fraction (LVEF) (<16%). He presented with progressive dyspnoea and intolerance to physical activity, with New York Heart Association (NYHA) functional classification III and AHA/ACC/HFSA stage D. Patient's history included mitral valve replacement by mechanical prosthesis in October 2017, with good functional progression, which then developed into severe paravalvular leak (PVL) and severe tricuspid regurgitation.
In 2019, the patient presented with reduced exercise tolerance and physical activity. With the exacerbation of symptoms in April 2022 due to SARS-CoV-2 infection, he was admitted to a COVID-19 converted intensive care unit of Hospital General de México "Dr. Eduardo Liceaga". After a thorough assessment by the Cardiology Department and the Cardiac Intensive Care Unit (CICU), it was decided to present him as a candidate for a heart transplant. Surgery took place on June 9th 2022 with an orthotopic transplantation from a deceased 23-year-old man. Cold ischaemia lasted three and a half hours. Mechanical ventilation was successfully weaned 24 hours after surgery. Transthoracic echocardiogram (TTE) performed four days after surgery revealed an LVEF of 55%. An endomyocardial biopsy was performed on June 27th 2022, showing 2R graft rejection managed by immunosuppression, with 1R control at one week.
Initial physiotherapy assessment
On 14 June 2022, the Critical Area Physiotherapy Department visited the Cardiac Intensive Care Unit (CICU) for an initial postoperative assessment at day 5. The patient was found to be in semi-Fowler position, without mechanical ventilation, calm and cooperative. The Glasgow Coma Scale was 15/15, Richmond Agitation-Sedation Scale (RASS) 0 points, with no signs of delirium. He was receiving haemodynamic support with dobutamine in moderate doses, as a continuous infusion, to maintain arterial perfusion pressures. Physical examination revealed a mediastinal tube and two left and right chest tubes connected to suction with functional water seals.
Global muscle strength was assessed using the Medical Research Council Sum-Score (MRC-SS)8-10, with an initial score of 55/60 and hand dynamometry with a force of 22 kg on the dominant side. Favourable results ruled out the presence of intensive care unit-acquired weakness (ICU-AW). Similarly, the initial degree of functionality was assessed using the ICU Mobility Scale (IMS), with a score of 1/10 that, for the time being, represented the functional ability to perform active movement/exercise in bed independently.
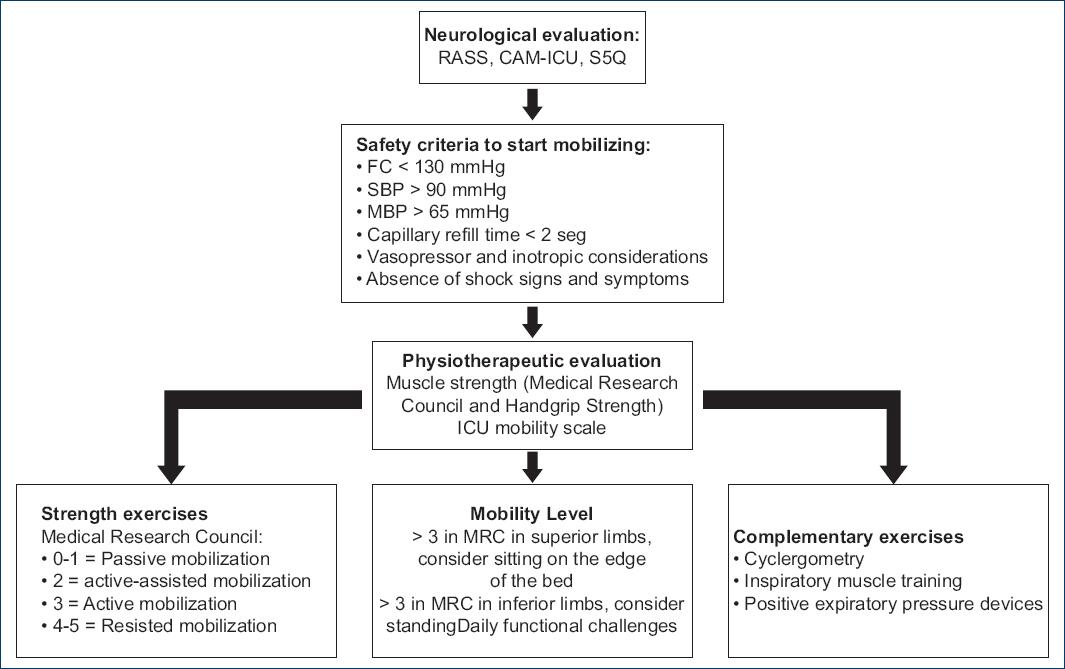
Figure 1 illustrates an algorithm for implementing an early mobilisation programme in CICU. This programme is accompanied by interventions likely to facilitate functional progression according to the score obtained on the MRC-SS and IMS scales.
Functional progression in the CICU
Phase I of the CRP began on the fifth post-surgical day with physical rehabilitation sessions: twice a day, six times a week, 40 to 60 minutes per session. The time slotted to the preparation, plateau (main) and recovery phases of the physical exercise were considered. The intervention began with active, resistant exercises of all four limbs in bed, using elastic bands, walking sticks and gravity itself, in all ranges of motion. According to the optimal outcomes in muscle strength and mobility tolerance, the strategy of each intervention was aimed to reach daily functional challenges. The achievement of functional progression is described in the IMS and days of physiotherapy sessions and shown in Figure 2, Figure 3 and Figure 4. Starting with stages with lower complexity of mobility but which represent a milestone in the naturalness of movement, such as sitting at the edge of the bed, transferring to the bed, achieving supported active standing. Then, stages with a higher degree of complexity such as walking on the spot, assisted walking and finally independent walking.

Figure 2 Functional progression of the patient according to the ICU Mobility Scale. ICU mobility scale (IMS): 0 = Nothing lying in bed, 1 = sitting in bed (exercises in bed), 2 = Passive transfer to chair, 3 = sitting at the edge of the bed, 4 = standing, 5 = transfer active chair, 6= static walking, 7 = walking with the assistance of 2 people, 8 = walking with the assistance of 1 person, 9 = independent walking with the help of a walking aid (cane or walker), 10 = independent walking.

Figure 4 Patient performing exercises with elastic resistance and inspiratory muscle training with linear pressure loading device.
The modified Borg Rating Scale of Perceived Exertion (RPE)11,12 was used to monitor and guide exercise intensity. By consensus, the following safety parameters were defined for stopping exercise: perceived exertion rated > 4 on the modified Borg rating scale, increased heart rate > 15 bpm from baseline and/or clinical evidence of exercise intolerance. Heart rate was not used for exercise prescription.
Complementary exercises were included, such as inspiratory muscle training (IMT) with a linear pressure loading device, and breathing exercises with positive expiratory pressure devices (Threshold PEP®, for both). As for the characteristics of the denervated heart, HR was between 110 and 115 bpm during the initial phase. There was no relevant chronotropic response during exercise.
Physiotherapeutic assessment at discharge
After 16 days of stay in the CICU and treatment by our team, it was decided to perform a series of examinations similar to the one described on the first day of treatment. However, the functional development and tolerance to physical activity that had developed after the intensive prescription of physical activity in the ICU allowed us to include Tinetti Gait and Balance Test, Barthel Index and the one-minute sit to stand test (1-MSTST). The following results were obtained on the day of discharge: IMS mobility level of 10/10 points, representing the ability to move independently without walking aids. An overall muscle strength score, according to the MRC-SS, of 60/60 points; and a total of 27.3 kg of grip strength in the dominant hand, measured by manual dynamometry. No integrated diagnosis of intensive care unit-acquired weakness (ICU-AW). At hospital discharge, with a level of mild dependence, according to the Barthel Index, with a total of 95 points. A favourable outcome, with no risk of falling, according to the assessment and score obtained in the Tinetti Gait and Balance Test; with 14/16 points for balance, 12/12 points for gait, and a total sum of 26/28 points. Finally, the global response and tolerance to exercise-induced stress were assessed using the 1-MSTST, obtaining a score of 17. In January 2023, a follow-up consultation was carried out, and the patient resumed his professional activities without restriction and reported full reintegration into his social roles.
Discussion
Heart transplant patients represent a challenge for healthcare professionals involved in their care. Rehabilitation plays an important role in achieving a favourable outcome for this population. The integration and monitoring of all its components optimises outcomes and enables patients to adhere to the CRP, even during their stay in intensive care. As part of CRP and ICU discharge programmes, education of the patient and family members about their condition, overall care, safety parameters and the benefits of exercise training, psychological follow-up, management by the nutrition department, optimised pharmacological treatment and ongoing exercise are of paramount importance13,14.
Although there are many tools for assessing functionality in the ICU, it seems prudent to use the IMS, due to its practicality, reproducibility and that it has been shown to be associated with significant outcomes at discharge. Exercise prescription in critically ill patients represents a major challenge for rehabilitation professionals. We now know that the best way to achieve this is to set functional goals and take account of the patient's perceived tolerance of exercise. Early mobility has been shown to be an important factor in reducing complications after cardiac surgery15,16. Inspiratory muscle training improves lung capacity, increases peak inspiratory pressure and reduces days of hospital stay. The use of positive expiratory pressure devices, such as the Threshold PEP®, can reduce atelectasis, improve residual functional capacity and promote drainage of tracheobronchial secretions17.











 nueva página del texto (beta)
nueva página del texto (beta)