Introduction
Small bowel obstruction (SBO) is a common cause of hospitalization in the operating room and brings remarkable morbidity and mortality with 30,000 deaths annually1.
This condition is responsible for 15% of all acute abdominal surgeries. It is reported that about 65-75% of strangulated intestinal obstructions (SIOs) are due to postoperative adhesions that usually occur within the first 4 postoperative weeks. The other pathological factors that can cause OIE are malignant tumors (10-20%), inguinal hernias (10-20%), inflammatory bowel disease (5%), and volvulus (3%)2. In about 0.2-0.9% of patients, OIE develops due to internal hernia. This hernia can develop due to the presence of abnormal anatomical changes or the presence of normal anatomical variations1.
Internal abdominal hernia is defined as a protrusion of the intestine or other organs through a natural opening or defect within the peritoneal cavity3 may cause incarceration, strangulation, or necrosis. The clinical symptoms are non-specific, and therefore, AIH is sometimes difficult to diagnose. On imaging, AIH-related findings can also be difficult to interpret. This difficulty leads to delays in diagnosis followed by ischemia, gangrene, perforation, and peritonitis. If strangulation develops, the overall mortality rate exceeds 50%3.
They are often manifested by an occlusive syndrome of which they constitute a rare etiology2. Internal hernias are a rare cause of SBO and are estimated to represent 1-6% of all cases, and transmesosigmoid hernias constitute 6% of all internal hernias2.
Presentation of the case
A 78-year-old female patient presented with a history of systemic arterial hypertension and hip surgery with prosthesis placement and cesarean section. She presented to the emergency department with abdominal pain, intolerance to the oral route, nausea and vomiting, absence of gas channeling, and bowel movements of 3 days of evolution. On examination, she was conscious, oriented, and with pale skin, blood pressure – 60/40 mmHg (TAM 46.66 mmHg), heart rate – 123 beats/min, and respiratory rate – 25 breaths/min. On abdominal examination, she has a distended abdomen, with absent peristalsis, tympanic, diffuse abdominal pain on palpation, rectal examination without alterations. It was decided to place a central venous catheter (right subclavian) to start aminergic support, a double antibiotic regimen, analgesics, and management with crystalloid solutions was started. A simple abdominal X-ray was performed, showing distension of the small bowel loops (Fig. 1), a control chest X-ray was also taken showing right pneumothorax, for which it was decided to place an intrapleural tube without complications. A nasogastric tube was placed with evidence of fecaloid discharge. Upon admission, laboratories are taken reporting: Complete blood count: Hemoglobin – 9.8 g/dL (Grade II or moderate anemia according to the World Health Organization), leukocytosis 16.92 at the expense of neutrophilia 87.6%, blood chemistry: Glucose – 255 mg/dL (hyperglycemia), serum creatinine – 1.7 mg/dL (Grade I acute kidney injury), prothrombin time – 14.9 s, partial thromboplastin time – 35.9 s, and INR – 1.11.

Figure 1 Simple abdominal X-ray showing dilated intestinal loops with a coin-stack pattern, interloop edema, and multiple air-fluid levels, absence of distal gas in the colonic setting.
The diagnoses of intestinal occlusion secondary to probable adhesions and septic shock are integrated, so the patient is stabilized and admitted to the operating room. Exploratory laparotomy was performed, finding 100 cc hemoperitoneum, internal hernia secondary to adherence in the pelvic region, with 70 cm of ischemic small intestine that did not remit to release, starting 130 cm from the angle of Treitz and ending 30 cm from the valve. ileocecal; adhesiolysis is performed and it is decided to perform intestinal resection of affected segments (Fig. 2), the distal stump is closed in two planes (Connel-Mayo and Lembert), a pneumatic test is performed without leakage, prophylactic appendectomy is performed, drainage is placed with left counter-opening, toward the pelvic cavity, the proximal segment of the resection is exteriorized through the right counter opening (Fig. 3).
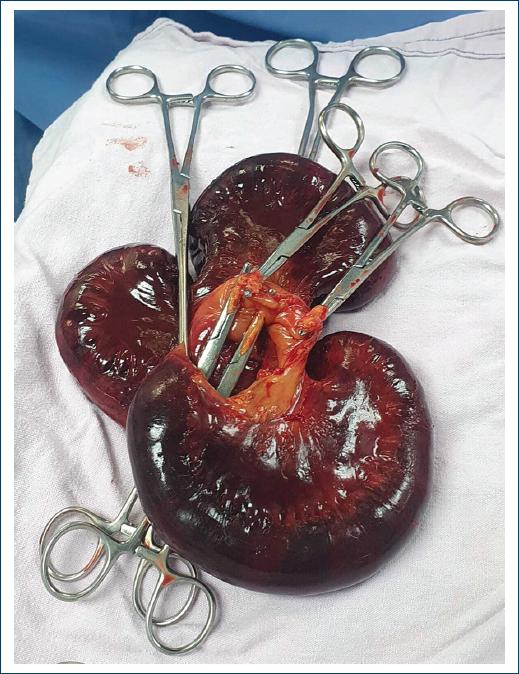
Figure 3 Resected segment of 70 cm of small intestine with non-reversible acute mesenteric ischemia.
The postoperative period was uneventful, with recovery of intestinal transit, removal of aminergic support, and removal of the nasogastric tube on the 2nd day. Tolerating the diet, removing Penrose drainage and crystalloid solutions on the 3rd day. The intrapleural tube was removed on the 7th day, and he was discharged after the 10th day due to a state of dehydration secondary to short bowel syndrome. The patient is discharged with the intention of performing a second surgical intervention in an adequate nutritional state, to reconnect the patient and avoid chronic short bowel syndrome.
Discussion
SIO is defined as intestinal obstruction with compromised intestinal blood flow and can be caused by a fibrous cord, torsion, internal hernia, or adhesions due to previous abdominal surgery. OIE is a serious condition that requires early diagnosis and immediate surgery because intestinal ischemia due to strangulation of the intestine can lead to necrosis of the intestine and even perforation, which can cause septic shock4. In terms of OIE, a late intervention has a high risk of mortality, and the mortality rate is reported to be 16%4. Identifying patients with OIE is vital to understanding the severity and managing the deterioration of the condition, including perioperative intensive care4. Regardless of the experience or seniority of the surgeon, the physical examination for the detection of strangulation has a success rate of only 48%5.
Since internal hernias are rare and have nonspecific clinical features, preoperative diagnosis is difficult. Plain abdominal radiography may demonstrate a distended, fluid-filled stomach or reveal dilated loops of small intestine into an ovoid mass. CT can detect OIE with a sensitivity ranging from 73% to 100% and a specificity ranging from 61% to 100%5. The clinical presentation with vague signs of intestinal obstruction, abdominal pain, nausea, and vomiting in 80%, the obstruction can be immediate or intermittent, but it is the reason for consultation in almost 90% of cases6.
Ultrasound can assess the degree of intestinal dilation, the level of obstruction, the probable involvement of the large intestine, and the presence of peristalsis; however, it has no advantage over TAC. Imaging studies, such as a simple abdominal X-ray, show dilatation of the small intestine and air-fluid levels in most cases, non-specific findings and present in all cases of SBO of any origin6. Treatment of internal hernias requires reduction of the hernia and repair of the defect using a laparoscopic or open approach (Bandawar et al.). In a manual reduction surgery for an internal hernia, with repair of a mesenteric defect and resection of small intestine necrosis, they decided to perform a stoma taking into account the general and intestinal condition of the patient, which progressed with an uneventful recovery and because this procedure is preferred due to the state of intestinal hypoperfusion versus intestinal anastomosis6.
Early laparotomy is mandatory because trapped bowel obstruction can lead to ischemia and perforation with high mortality. The steps of the operation include adequate incision, reduction of the hernia content, repair of the defect, and avoiding injury to the mesenteric vessels7.
Emergency exploratory laparotomy is mandatory to avoid the high risk of death. Surgical intervention is indicated for patients with intestinal obstruction or high risk of incarceration. Early diagnosis and timely treatment prevent additional complications and prolonged hospitalization8.
Conclusions
Internal hernias are not a frequent cause of intestinal occlusion, however, it is important to take it into account as a cause of it, especially in elderly patients with comorbidities and a history of previous surgeries with data of septic shock, to make a relevant diagnosis and avoid intestinal ischemia. Whenever there is suspicion of low viability of the small intestine, resection should be performed to avoid intestinal necrosis and perforation.











 nueva página del texto (beta)
nueva página del texto (beta)



