Introduction
Liver rupture can occur due to different etiologies during pregnancy, including tumors, traumatic causes, and secondary rupture due to severe preeclampsia1, cases of rupture without any identifiable pathology are exceptional2. Some cases have been reported where only subcapsular hematoma is present, without total rupture, in which there is a less severe evolution3,4 also, there is cases reported where there is only rupture of the hepatic capsule but complicated with necrosis and fulminant liver failure with subsequent multi-organ deterioration mainly cerebral and pulmonary5. However, its clinical presentation is usually catastrophic6. The frequency of presentation varies from one in 45,000 to one in 250,000 pregnancies complicated by liver rupture7,8. In Mexico, the most numerous case reports were reported by Murillo and Hernández, a series of 79 patients from 1985 to 1999 in which a frequency of one in 128,927 births was documented9. Pathophysiology is usually explained by periportal hemorrhage, intravascular fibrin deposits, which cause sinusoidal obstruction, intrahepatic vascular congestion with increased tissue volume, ischemia, and tension rupture trapped with the hepatic capsule, of complicated preeclampsia with HELLP syndrome10,11.
The treatment described for liver rupture goes from packing12,13, selective hepatectomy14, patch use with omentum15, selective embolization with interventional radiology16, and liver transplantation in extreme cases17 generally, the combination of different techniques is more effective. Prognosis is variable, but usually fatal18 with mortality of 60-70% of reported cases19. Mortality may be higher if severe bleeding develops, shock state with liver necrosis and complications added to acute liver failure and others associated with the clinical phenomenon of preeclampsia20.
Clinical cases
We present the case of a 23-year-old patient, with 4 h of immediate puerperium, send from Texcoco General Hospital, on air ambulance occurred on March 2022.
Anthropometrics: weight 50.0 kg, Size 1.53 m, BMI: 24.6 kg/m2, Predicted weight 45.68 kg, Ideal theoretical weight 47.1 kg; Body surface area 1.53 m2. Mestizo ethnic group.
Obstetric history: a previous pregnancy complicated by early onset preeclampsia.
Motive of hospital transfer was HELLP syndrome and liver rupture. Important, mention a previous pregnancy end by cesarean section, indicated by severe preeclampsia at 38 weeks of gestational age, with total remission in puerperium period. No history of chronic diseases. History of sudden onset 10 h of evolution of the following symptoms: intermittent frontal and temporal headache, intense 10/10, pain in the upper right abdominal quadrant, pulsatile and very intense 10/10, associated with noninvasive high blood pressure 170/120 mm Hg, severe preeclampsia, HELLP syndrome, integrated by lactate dehydrogenase 918 UI/L, GOT 121 UI/L, GPT 108 UI/L, platelets 90,000/mm3. Pregnancy of 25 weeks of gestational age, fetal death Cesarean section and damage control surgery was performed trans cesarean section (liver packing) in her unit of origin, transfer was made by air transport. She was received in Shock area with sedation based in propofol, and midazolam, invasive mechanical ventilation in volume controlled mode, shock state, hemoperitoneum detected by FAST ultrasound, and evidence of bleeding by drainage type Penrose, protocol for mass transfusion was started, stabilization with quality volume and vasopressor support, because she was in hypovolemic shock status with MAP of 35 mm Hg, meriting new damage control surgery.
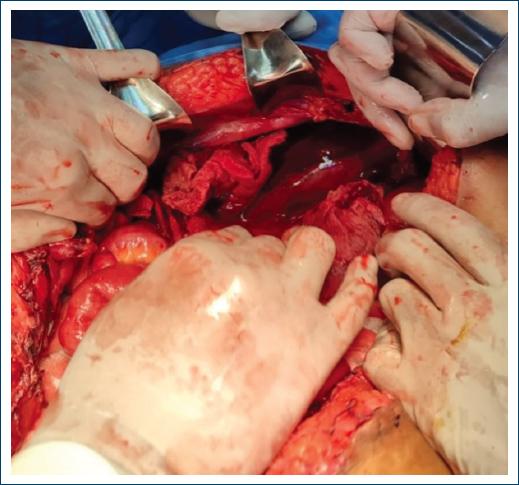
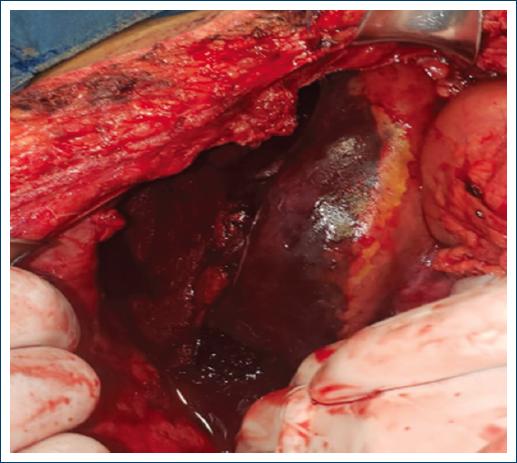
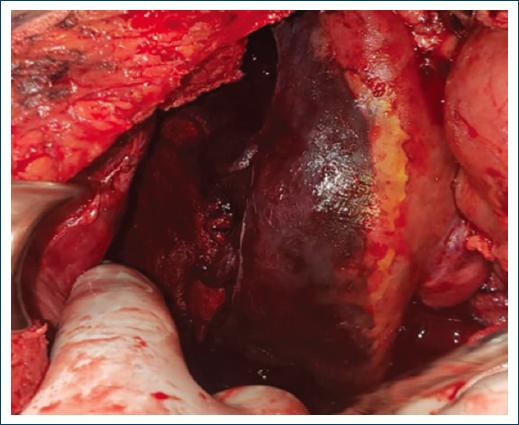
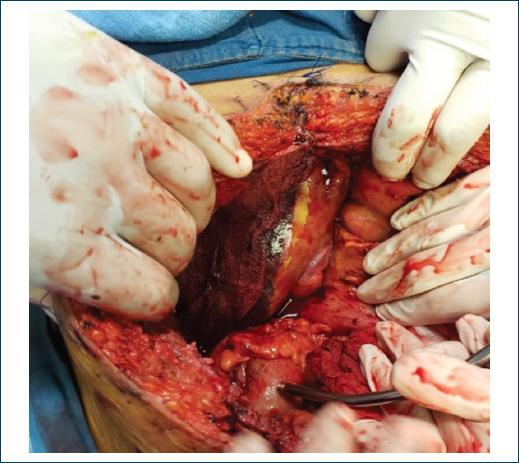
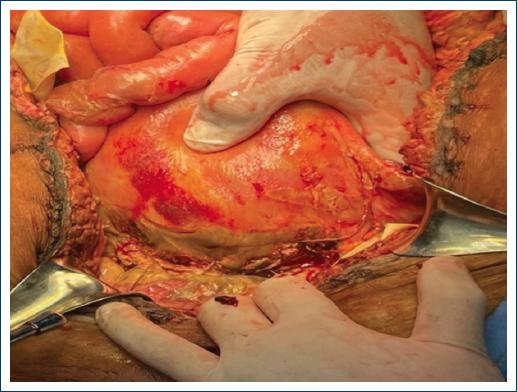
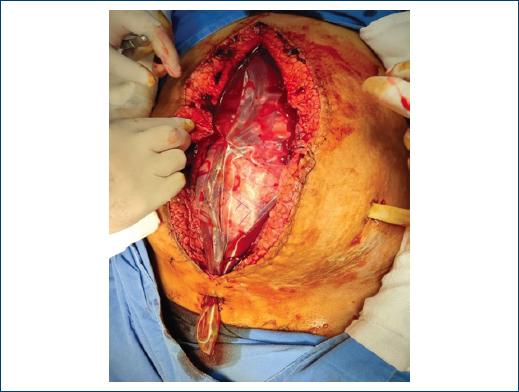
In the first surgical intervention performed in this hospital unit, hepatic rupture of segments V, VI, VI, and VIII was found, requiring packaging and placement of MALA bag with open abdomen. She presented torpid evolution, requiring a total of six interventions, with five packings and finally definitive closure with total abdominal hysterectomy, right oophorectomy, due to data of endomyometritis and unilateral salpingooophoritis (Figs. 1-11). The patient developed hepatic-metabolic failure, circulatory, renal, hematological, neurological failure, and septic shock (Tables 1-4). She was maintained with hemodynamic support, 18 days of mechanical ventilation, six renal sessions of hemodialysis, hematological (received total of 20 erythrocyte concentrates, seven platelet apheresis, 73 cryoprecipitates, 24 fresh frozen plasmas, 5 g of fibrinogen, 7000 mcg of recombinant factor VII, tranexamic acid 3 g), initially presented improvement of his state of coagulopathy, renal, hepatic, and circulatory failure between days 13 and 16 of hospitalization based on platelet values of 207,000/mm3, having previously been up to levels of 27,000/mm3, INR 1.39 previously reporting 1.88, hematocrit of 32.4%, with previous 20%, glucose controls of 85 to 140 mg/dL, with the previous hypoglycemia of up to 37 mg/dL, serum lactate 2 mmol/L, with previous 7-10 mmol/L. fibrinogen of 207 mg/dL, with previous up to 95 mg/dL. pH of 7.41, when previously presented acidemia with pH up to 7.2, bicarbonate of 22.9 mMol/L, with the previous of up to 16 mMol/L. creatinine of 1.5 mg/dL, with previous of up to 7 mg/dL. LDH of 515 IU/L, with preamps up to 10,813 IU/L, ast and ALT of 125 and 72 IU/L, with preamps up to 7000 IU/L both. Deterioration in her past 2 days of life with fatal outcome after 18 days of hospitalization with multi-organ failure induced by sepsis, demonstrated by result of culture of blood sample with the same germ as in peritoneal culture and hemodynamic profile (systemic vascular resistance 549 dyna-sec/cm5 and increased cariac output 12 L/min). Enterococcus faecium was isolated in peritoneal fluid culture and hematic sample, culture of bronchial secretions and urine were negative. Multidisciplinary treatment involved critical medicine, internal medicine, general surgery, anesthesiology, nephrology, infectiology, and nutrition staff.
Table 1 Arterial gasometry results
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ph | 7.29 | 7.24 | 7.36 | 7.26 | 7.3 | 7.3 | 7.39 | 7.4 | 7.37 | 7.44 | 7.38 | 7.35 | 7.31 | 7.41 | 7.49 | 7.37 | 7.35 | 6.9 |
| HCO3 | 17.2 | 16.9 | 19.5 | 19.4 | 21.1 | 21.7 | 16.7 | 20.7 | 21.1 | 21.1 | 19.6 | 20 | 21.8 | 22.9 | 22.6 | 22.3 | 20.7 | 6.7 |
| PCO2 | 34.2 | 40 | 35.2 | 44 | 44 | 46 | 20 | 30 | 37 | 27 | 30 | 34 | 44 | 34 | 26 | 38 | 32 | 36 |
| PO2 | 122 | 101 | 127 | 100 | 110 | 97 | 96 | 88 | 72 | 77 | 70 | 95 | 111 | 122 | 104 | 47 | 38 | 61 |
| D base | 8 | 9.4 | 4.8 | 7.8 | 5.1 | 2.4 | 12.2 | 6.2 | 5.3 | 4.9 | 7.4 | 6.9 | 4 | 3.1 | 3.5 | 3.3 | 5.2 | 25 |
| Lactate | 4 | 7 | 4 | 2 | 3 | 2 | 3 | 4 | 2 | 3 | 2 | 2 | 3 | 4 | 2 | 2 | 4 | 10 |
Source: Clinical record.
Table 2 Hematological results
| Día | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| INR | 1 | 1.33 | 1.66 | 1.88 | 1.85 | 1.59 | 1.63 | 1.55 | 1.59 | 1.59 | 1.5 | 1.59 | 1.55 | 1.44 | 1.39 | 1.49 | 1.43 | 1.59 |
| PT | 14 | 15.2 | 11.6 | 20.7 | 20.4 | 17.8 | 18.2 | 17.3 | 17.8 | 16.8 | 17.8 | 17.3 | 16.2 | 11.6 | 16.2 | 16.7 | 16.3 | 17 |
| PTT | 34 | 60 | 30 | 25 | 32.5 | 32.3 | 35.8 | 49.3 | 34.3 | 33.6 | 37.1 | 42 | 44 | 75.5 | 25.6 | 25.6 | 40.2 | 32.6 |
| Hematocrit | 37 | 31.5 | 25.7 | 25.7 | 23.1 | 22.9 | 21.6 | 25.1 | 29.1 | 29.5 | 21.6 | 30.6 | 32.4 | 31.5 | 19.1 | 21.6 | 34.7 | 31.3 |
| Platelets | 90 | 75 | 26 | 66 | 51 | 57 | 69 | 67 | 56 | 63 | 60 | 67 | 207 | 75 | 78 | 100 | 102 | 120 |
| WBC | 12 | 15.1 | 5 | 5.4 | 8.9 | 11.5 | 9.4 | 8 | 8.8 | 8.4 | 9.4 | 7.5 | 21.1 | 15.1 | 22.4 | 11.6 | 7.7 | 2.7 |
Source: Clinical record.
Table 3 Blood chemistry results
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Glucose | 87 | 158 | 82 | 84 | 37 | 147 | 68 | 53 | 89 | 121 | 83 | 108 | 148 | 85 | 133 | 118 | 95 | 105 |
| Creatinin | 0.8 | 1.17 | 1.85 | 3.09 | 5.15 | 3.09 | 5.15 | 6 | 6.42 | 6.42 | 7.15 | 3.84 | 2.26 | 2.07 | 2.22 | 1.59 | 1.58 | 2.73 |
| BUN | 10 | 26 | 26 | 34 | 43 | 53 | 67 | 81 | 81 | 99 | 111 | 140 | 121 | 82 | 94 | 126 | 122 | 70 |
| Urea | 21 | 32 | 52 | 72.8 | 92 | 113 | 143.4 | 173 | 173 | 211 | 237 | 299 | 258 | 175 | 201 | 269 | 149 | 218 |
| Bilirrubin | 0.4 | 3.28 | 3.9 | 4.58 | 5.55 | 5.15 | 5.81 | 6.12 | 7.08 | 7.27 | 8.51 | 5 | 11.5 | 12.89 | 10.15 | 13.72 | 13.9 | 12.9 |
| AST | 121 | 1000 | 1000 | 6000 | 7336 | 2800 | 846 | 450 | 227 | 144 | 125 | 121 | 162 | 167 | 125 | 166 | 131 | 138 |
| ALT | 108 | 1100 | 1100 | 7000 | 4366 | 2524 | 881 | 398 | 229 | 130 | 87 | 80 | 80 | 72 | 72 | 66 | 97 | 11 |
| LDH | 918 | 1343 | 750 | 4500 | 10813 | 4500 | 1036 | 870 | 704 | 947 | 1250 | 886 | 860 | 515 | 663 | 652 | 690 | 688 |
Source: Clinical record.
Table 4 Seric electrolytes
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sodium | 137 | 137 | 139 | 141 | 142 | 141 | 142 | 142 | 137 | 138 | 139 | 139 | 141 | 140 | 140 | 141 | 142 | 142 |
| Potassium | 6.3 | 6.13 | 7.18 | 7.18 | 6.26 | 6.47 | 6.19 | 6.19 | 7.65 | 6.78 | 6.57 | 5.1 | 4.6 | 4.26 | 4.78 | 4.77 | 4.77 | 4.53 |
| Chlorine | 108 | 106 | 107 | 108 | 108 | 107 | 108 | 106 | 106 | 106 | 107 | 103.37 | 108 | 109 | 108 | 108 | 104 | 103 |
| Calcium | 7.3 | 8.2 | 7.9 | 7.8 | 7.3 | 6.6 | 6.8 | 6.7 | 6.8 | 6.9 | 6.7 | 7.5 | 8.41 | 7.6 | 8.2 | 8.1 | 7.9 | 7.9 |
Source: Clinical record.
Discussion
It has been documented since the nineties that liver rupture due to preeclampsia is a condition of very low incidence but high mortality, as described in numerous clinical case reports above1-6, This case is one of the few that have been documented in the world, since its incidence is very low, generally the reported cases are hematomas and not complete rupture7-9.
In the example mentioned, it initially evolved with severe hypertension and later with hemorrhagic shock, due to the massiveness of bleeding after liver rupture and consequent bleeding10,11.
In the reported case, a damage control surgery protocol was made with six interventions in total, which were performed by the most trained personnel; however, there were some of the available options known in the literature, such as selective embolization, liver transplantation, interventional radiology measures, etc.12-17.
However, due to the complications of concomitant preeclampsia, such as disseminated intravascular coagulation and the massive endothelial lesion developed, a series of events occurred that led to the need for multiple surgical reinterventions and with it the fearsome complication of intra-abdominal sepsis, which was finally the cause of her death, resulting similar to that described in multiple case reports and literature reviews cited18-20.
Conclusion
Liver rupture is a deadly complication of preeclampsia and represents a challenge for the surgeon facing this clinical entity, as well as for the multidisciplinary team that performs the organic support during hospitalization in intensive care. The case of the patient presented had a fatal outcome; however, all possible medical and surgical interventions were performed, as well as multidisciplinary management of each of the organic failures that manifested themselves during the clinical course of her condition. Early detection of preeclampsia and its timely treatment can prevent such tragic and costly social and economic outcomes.











 nueva página del texto (beta)
nueva página del texto (beta)