Background
Thrombolytic therapy is a vital reperfusion strategy in ST-segment elevation myocardial infarction where primary percutaneous coronary intervention cannot be offered promptly but is well known for its hemorrhagic complications1-3. The incidence of major bleeding in patients who receive thrombolytic therapy has been reported at 3.6%, gastrointestinal bleeding the most common site (31.5%), followed by vascular access bleeds (23.8%)4. Peptic ulcer disease is the most typical cause of gastrointestinal bleeding after thrombolytic therapy5. In the literature, few reports of thrombolytic therapy reveal undiagnosed colonic carcinoma5,6. We report the case of a colonic adenocarcinoma diagnosed following thrombolytic therapy on myocardial infarction.
Case report
An 82-year-old man presented to the emergency department with severe, acute precordial chest pain. His past medical history included heavy smoking for 20 years (1 pack/day). An electrocardiogram showed an acute posteroinferior epicardial injury (Fig. 1).
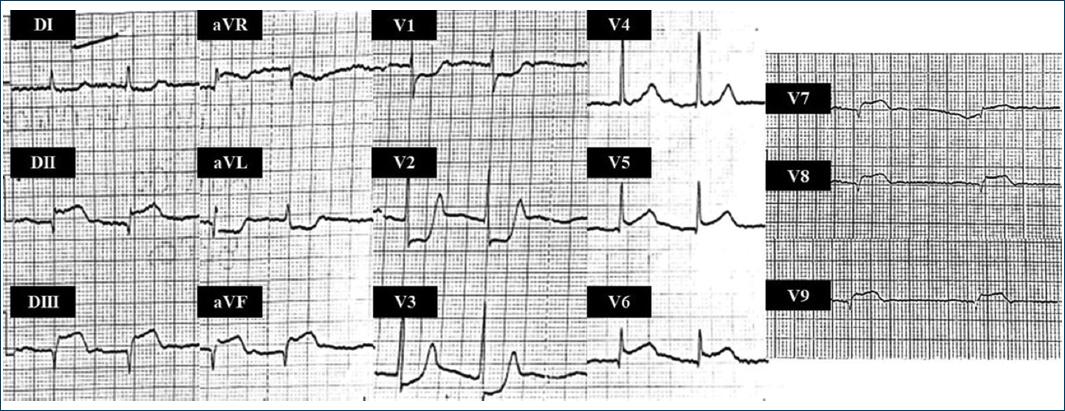
Figure 1 Initial electrocardiogram: elevation of ST-segment in leads DII, DIII, aVF, V7-V9, depression of ST-segment in leads aVL, and V1-V3 (posteroinferior epicardiac injury).
Acetylsalicylic acid 300 mg PO, atorvastatin 80 mg PO, Clopidogrel 75 mg PO, and enoxaparin 60 mg SC with tenecteplase 20 mg IV were administered. The patient's clinical condition improved, and the electrocardiogram showed reperfusion criteria (Fig. 2).
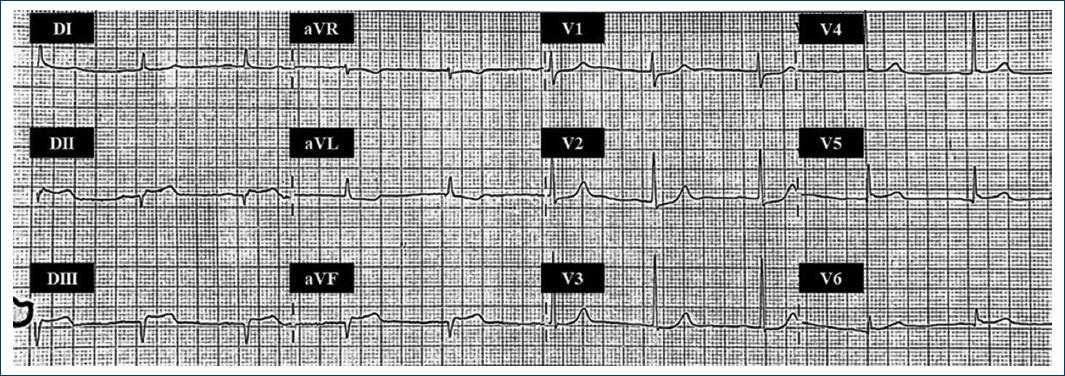
Figure 2 2 h post-thrombolytic therapy electrocardiogram: depression of ST-segment in leads DII, DIII, aVF with normalization of ST-segment in leads aVL, and V1-V3.
Approximately ten hours later, he experienced hematochezia; blood tests were relevant due to a descent of hemoglobin (Table 1). He denied no gastrointestinal symptoms before hospital admission. Abdominal and rectal physical explorations were normal. He received a blood transfusion, and a colonoscopy with biopsy revealed adenocarcinoma in the ascending colon (Fig. 3). We continued antiplatelet therapy without recurrent bleeding. He recovered and was discharged home symptom-free 4 days after hospital admission.
Table 1 Laboratories on hospitalization
| At admission | At the hemorrhagic event | At hospital discharge | Reference range | |
|---|---|---|---|---|
| Leukocytes, mm3 | 8,390 | 9,790 | 8,130 | 5,000-10,000 |
| Platelets, mm3 | 222,000 | 192,000 | 166,000 | 130,000-400,000 |
| Hemoglobin, g/dl | 13.2 | 9.9 | 10.7 | 14-18 |
| Hematocrit, % | 40.7 | 30 | 32.7 | 42-52 |
| Sodium, mEq/L | 129 | 132 | 135 | 136-145 |
| Potassium, mEq/L | 3.9 | 4.1 | 3.8 | 3.5-5.1 |
| Chlorine, mEq/L | 99 | 104 | 102 | 98-117 |
| Magnesium, mg/dl | 1.8 | 1.9 | 1.9 | 1.9-2.7 |
| Glucose, mg/dl | 111 | 106 | 86 | 74-106 |
| Creatinine, mg/dl | 1.12 | 1.1 | 0.75 | 0.7-1.3 |
| Urea, mg/dl. | 53 | 54 | 24 | 18-50 |
| Blood urea nitrogen, mg/dl | 24 | 25 | 11 | 9-23 |
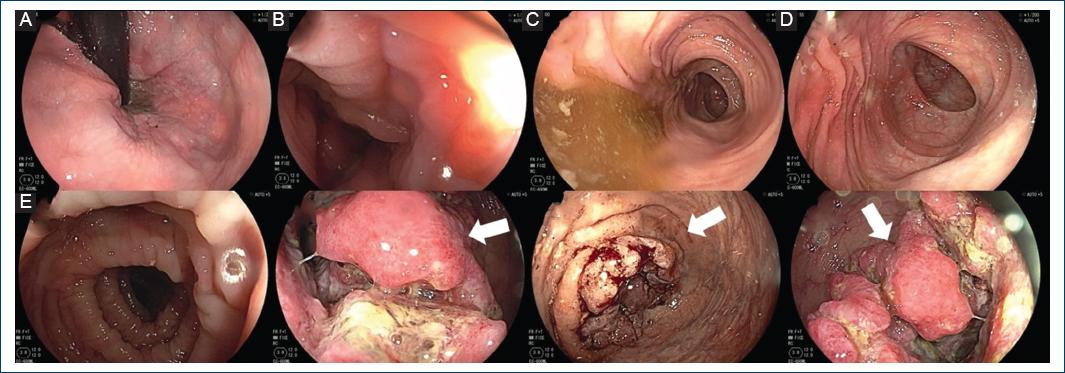
Figure 3 Colonoscopy. A, B, C, and D: rectum, sigmoid colon, descending and transverse colon preserved shape and architecture, mucosa of normal appearance. E: ascending colon: exophytic, ulcerated lesion with irregular edges that occlude 70% of the colonic lumen (arrows).
He underwent a right hemicolectomy 1 month later. Further, workup confirmed the cecum's invasive adenocarcinoma (T4aN0M0, stage IIB). The tumor was successfully removed, and chemotherapy was initiated.
Discussion
Bleeding is a frequent complication of managing coronary artery disease (CAD) patients, especially those presenting with acute coronary syndromes (ACS). Studies have shown a risk of major bleeding of 1-8% at 30 days in ACS patients. The gastrointestinal tract is one of these patients' most frequent bleeding sources7. The literature reports that patients who experience gastrointestinal bleeding while on anticoagulation or antiaggregant therapy positively diagnose colonic cancer at early stages (Stage I, II)8-11.
Proximal colon cancer has a poorer prognosis than left colon cancer due to late-stage diagnosis and advanced patient age. Distal colon and rectum cancer symptoms include changing defecation habits, fresh rectal bleeding, mucoid discharge, and obstruction. In addition, proximal colon cancer is associated with anemia and non-specific symptoms. Due to non-specific symptoms such as anemia, abdominal pain, fatigue, and weight loss, it is difficult to diagnose the disease efficiently, resulting in a low survival rate10.
One-hundred and thirty-five cases of colonic cancers during thrombolytic, anticoagulation, or antiaggregant therapy have been reported in five studies (Table 2). Of the reported cases, 83 patients were diagnosed with the early-stage colonic cancer5,6,9-11.
Table 2 Clinical characteristics of cases of colonic cancer diagnosed due to hemorrhagic complication following thrombolytic, anticoagulation, or antiplatelet therapy
| Author | Year | Country | Number of cases | Sex | Age (years) | Therapy type | Dosage | Site | Histology | Colonic cancer stage | Clinical outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baker et al5 | 2002 | United Kingdom | 1 | Male | 68 | Thrombolytic | Not specified | Descending colon | Not specified | Dukes's B carcinoma (Stage II) | Not specified |
| Schellhammer et al6 | 2007 | Germany | 1 | Female | 57 | Thrombolytic | Alteplase; 20 mg | Rectosigmoid colon | Adenocarcinoma | Stage IIIa | Not specified |
| Norton et al9 | 1997 | United Kingdom | 8 | Not specified | 61 to 79 | Anticoagulation | Warfarin; Not specified | 6 in Caecum 2 in Proximal transverse colon | 7 Adenocarcinoma 1 Non-Hodgkin lymphoma | 2 Dukes's A carcinoma (Stage I) 4 Dukes's B carcinoma (Stage II) 1 Stage IV Non-Hodgkin lymphoma: Not specified | Alive and well with follow-up ranging from 2 years (lymphoma) to 4 years (Stage IV) |
| Aday et al10 | 2017 | Turkey | 27 | 14 Males 13 Females | 34 to 88 | Antiplatelet | 8 only clopidogrel 9 only aspirin 10 Aspirin + Clopidogrel | Proximal colon | Not specified | 20 Stage I/II (74%) 7 Stage III/IV (26%) | Not specified |
| Symeonidis et al11 | 2012 | Greece | 98 | Not specified | 71 (range 52-91) | Antiplatelet | 65 Aspirin: 100 mg/d for 15.3 ± 6.51 years. 17 Clopidogrel: 75 mg/d, 5.85 ± 3.46 years 6 Ticlopidid: 250 mg twice daily, 5.85 ± 3.46 years 4 Dipyridamole: 200 mg twice daily, 5.85 ± 3.46 years. 6 Dual therapy; Not specified. | 42 Right colon 33 Left colon 23 Rectum | Not specified | 56 Stage I/II (57%) 34 Stage III (35%) 8 Stage IV (8%) | Not specified |
| Alanís et al. (present case) | 2022 | Mexico | 1 | Male | 82 | Thrombolytic | Tenecteplase; 20 mg | Ascending colon | Adenocarcinoma | Stage IIB | Alive and well during the first year follow-up |
The concomitance of very high thrombotic and hemorrhagic risks in a patient with bleeding poses complex treatment decisions7. Mehran et al. proposed an objective, hierarchically graded bleeding classification that serves the clinical community as helpful guidance on managing patients with antithrombotic or anticoagulant drugs who suffer any bleeding. (Bleeding Academic Research Consortium [BARC] Definition for Bleeding) (Table 3)12. When the thrombotic risk is higher than the risk of recurrent bleeding in a patient who develops minor (BARC type 2) or major bleeding (BARC type ≥ 3)12, it is suggested to continue antithrombotic therapy, as long as the bleeding event is not a life-threatening bleed7. In the case of resuming antiplatelet therapy after gastrointestinal bleeding, it is recommended to restart a single treatment with low-dose aspirin with restarting the second antiplatelet agent as soon as possible7.
Table 3 Bleeding academic research consortium (BARC) definition for bleeding
| Type | Definition |
|---|---|
| 0 | No bleeding |
| 1 | Bleeding that is not actionable and does not cause the patient to seek unscheduled performance of studies, hospitalization, or treatment by a health-care professional; may include episodes leading to self-discontinuation of medical therapy by the patient without consulting a health-care professional |
| 2 | Any overt, actionable sign of hemorrhage (e.g., more bleeding than would be expected for a clinical circumstance, including bleeding found by imaging alone) that does not fit the criteria for type 3, 4, or 5 but does meet at least one of the following criteria: (1) requiring non-surgical, medical intervention by a health-care professional, (2) leading to hospitalization or increased level of care, or (3) prompting evaluation |
| 3 a | Overt bleeding plus hemoglobin drop of 3-< 5 g/dL (provided hemoglobin drop is related to bleed) Any transfusion with overt bleeding |
| 3 b | Overt bleeding plus hemoglobin drop ≥ 5 g/dL (provided hemoglobin drop is related to bleed) Cardiac tamponade Bleeding requiring surgical intervention for control (excluding dental/nasal/skin/hemorrhoid) Bleeding requiring intravenous vasoactive agents |
| 3 c | Intracranial hemorrhage (does not include microbleeds or hemorrhagic transformation, does include intraspinal) Subcategories confirmed by autopsy or imaging or lumbar puncture Intraocular bleed compromising vision |
| 4 | Coronary artery bypass graft-related bleeding Perioperative intracranial bleeding within 48 h Reoperation after closure of sternotomy for the purpose of controlling bleeding Transfusion of ≥ 5 U whole blood or packed red blood cells within a 48-h period Chest tube output ≥ 2 L within a 24-h period |
| 5 a | Probable fatal bleeding; no autopsy or imaging confirmation but clinically suspicious |
| 5 b | Definite fatal bleeding; overt bleeding or autopsy or imaging confirmation |
We present a patient with a colonic carcinoma been revealed due to a thrombolytic therapy complicated by a gastrointestinal major bleeding event (BARC type 3a: Overt Bleeding plus Hemoglobin drop > 3 to < 5 g/dL), a situation few documented in the literature. A colonoscopy with biopsy was performed for further evaluation, showing adenocarcinoma in the ascending colon. After stabilization of a patient with a moderate risk of recurrent bleeding risk (Extracranial major bleeding) but with a very high thrombotic risk (ACS <8 days), antithrombotic therapy was restarted without recurrent bleeding or hemoglobin drop.
Conclusion
This case illustrates a complication of thrombolytic therapy that led to the discovery of undiagnosed colon cancer. Patients with proximal colon cancer have a poorer prognosis due to non-specific symptoms, resulting in a low survival rate. Early-stage diagnosis rates are higher in patients with rectal bleeding and melena. As a result of thrombolytic therapy, occult bleeding from colonic cancer becomes apparent. Increasing awareness of this fact may result in earlier detection of colonic cancer in asymptomatic patients and a greater likelihood of survival. In addition, an examination of the digestive tract should be conducted for patients who develop gastrointestinal bleeding after thrombolytic therapy to exclude serious but potentially curable conditions.











 nueva página del texto (beta)
nueva página del texto (beta)


