Introduction
The incidence of lateral hernias is low, which makes them an infrequent pathology in clinical practice. Due to this, their reconstruction is an issue that is often discussed, without having standardized management1. There are only around 250 cases reported in the literature to date1. The first reported case was described in 1906 by Clarence Selby2, in which he presents a patient with a hernia after a 2-meter fall as a 32-year-old construction employee. The current 2009 European Hernia Society (EHS) classification includes lateral abdominal hernias into 4 bilateral zones: subcostal (L1), flank (L2), iliac (L3), and lumbar (L4)3. Even having this classification with well-defined nomenclature, some case reports indiscriminately use the term "flank hernia", referring to hernias that are located lateral to the rectus muscle, which can create confusion in the data, however, the management and approach of flank, iliac, and lumbar hernias can generally be performed in the same way as the specific location has little impact on outcome4,5.
With respect to lateral hernias, about 80% are acquired and the remaining 20% correspond to congenital hernias, the latter frequently associated with other malformations6. Of the acquired hernias, these are frequently associated with renal, hepatic, and vascular surgery and, less frequently, trauma7. Identified risk factors for flank hernias are: high body mass index (BMI >30), end-stage renal disease, chronic obstructive pulmonary disease, smoking, diabetes mellitus, hypertension7, longer flank surgical incision at 15cm probably associated with nerve injury and prolonged immunosuppression in renal transplant patients1. The aim of the present manuscript is to report a case managed at the General Hospital of Mexico "Dr. Eduardo Liceaga" by the general surgery service in conjunction with plastic and reconstructive surgery.
Case report
This is a 30-year-old male, a bodybuilder by occupation prior to the current condition, with a BMI of 25 kg/m2, with no significant clinical or surgical history. The patient presents abdominal trauma caused by a motorcycle accident, he is admitted to an external hospital with a diagnosis of hypovolemic shock, fracture of the left iliac bone and lumbar displacement in L2-L3, at that time an exploratory laparotomy was performed in which an external iliac artery lesion was found and repaired and damage control surgery and abdominal packing with compresses to later be referred to another institution where he continued his management with surgical toilets and abdominal closure contained to the skin with an incision on the left iliac surface. Eight months after the closure, the patient is referred to our hospital, where the joint protocol of the general surgery service is carried out in the wall and soft tissue clinic and in the plastic and reconstructive surgery service.
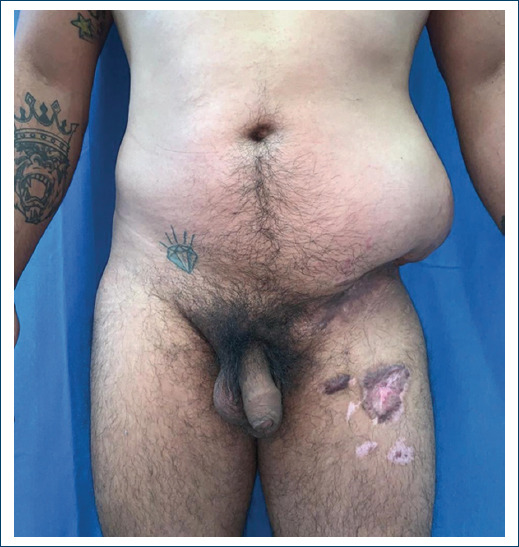
On physical examination, patient was found with abdominal asymmetry due to increased volume of the flank and left iliac surface, approximately 30x15x4cm, with hyperchromic coloration, skin with telangiectasias, skin and fat atrophy, localized hyperthermia, Intestinal peristalsis is palpable on the abdominal flank, it is not possible to delimit all the edges of the defect with palpation. A bone fragment corresponding to the anterosuperior iliac crest rotated lateral, anterior and caudal is palpated and above it, the hernia. There were no alterations in gait or sensory alterations in the area (Fig. 1). Computerized axial tomography shows (Fig. 2) the hernial sac containing the sigmoid colon and small bowel loops, the fracture of the anterior superior iliac crest, consolidated in an abnormal position, disinserted of the major and minor oblique muscles and retraction towards cephalic and posterior.

Figure 2 Coronal cut computed tomography showing the disinsertion of the left oblique muscles, the fracture of the iliac bone and the lateral hernia containing the sigmoid colon.
Surgery is performed in April 2021, starting the general surgery service, with an open preperitoneal approach on a previous scar on the left iliac surface, the skin is incised with a scalpel, the hernial sac is located towards the head, it is dissected at its edges caudal, medial and cephalic, towards the posterior surface, there is difficulty in continuing the dissection as it is close to the thoracolumbar fascia and it is necessary to open the sac to continue, the sigmoid colon is found and it is rejected with the help of compresses and a Deaver colon separator. Once the sac was completely dissected, repaired and reduced, the defect was identified, approximately 25x15cm;an attempt was made to approximate the oblique muscles towards the ipsilateral anterior superior iliac crest without success since the retraction and contracture did not allow it, in addition to the anomalous position due to its consolidation, it was decided to place a light macroporous polypropylene mesh 30x30cm, which is made to adjust to the defect and be fixed to the fascia of the oblique major towards the cephalad, the anterior sheath of the left rectus towards the medial, the anterior superior iliac crest towards the caudal and the thoracolumbar fascia towards the lateral (Fig. 3). Due to the significant cutaneous and fatty atrophy of the skin overlying the hernia, it was decided to take a strip of lata fascia from the left leg, approximately 25x7cm, which allows the mesh to be covered to reduce the risk of its exposure to the skin, as well as to give continuity from the fascia of the greater oblique to the anterior superior iliac crest and fix it to the same anatomical sites mentioned above with 0 polypropylene suture (Fig. 4). A closed drain is placed and the skin that surrounds is remodeled. Subcutaneous fatty tissue decreased and closure was performed in three planes.
In the immediate postoperative period, the reduction (Fig. 5) and containment of the hernia was evident, the patient continued walking without difficulty or pain and was discharged having adequate pain control with oral medications. He continues with follow-up by external consultation 48 hours after the intervention. The drain is removed one week after discharge, once it has output of less than 30 ml/day and serous characteristics, the patient is kept without physical exertion for 6 months to avoid recurrence.
Discussion
Post-traumatic hernias are rare pathological entities, usually caused by car crashes (60%), motorcycle accidents (20%), falls (13%), pedestrian collision with a motor vehicle and injuries associated with bullfighting (7%)8,9,10. Despite the low incidence in blunt trauma (0.17%-1.5%), suspicion of hernia must be present when performing general and directed abdominal exploration. Clinical examination, in this type of hernia, has a sensitivity between 29-42%11 and the most frequent findings are ecchymosis (49%), localized volume increase or bulge (39%)12. Frequently, the patient with post-traumatic hernia presents associated intra-abdominal or vascular lesions (25-70%) that require an urgent laparotomy, coupled with the low sensitivity of the clinical examination, it is imperative to have a computed tomography in case of clinical doubt11. Early treatment is defined when it is carried out in the context of the first hospitalization during the trauma intervention and up to two weeks later, and late treatment when it is carried out in another hospitalization, after a period of two weeks, with most cases being after 6 months after the trauma. triggering event13.
Management, as in the rest of hernias, consists of dissecting the sac to free it from the edges of the defect, reducing the sac with its contents, and repairing the defect. It is important to mention that, up to now, there is no consensus to determine the best management In most of the reported cases open approaches (preperitoneal) have been performed, through the midline in the case of blunt trauma or by extending the wound in the case of open trauma or post-incisional hernias14-19 and laparoscopic approach in fewer cases20,21. The only indication found in the review for performing a laparoscopic approach is in the case of patients who did not receive immediate surgical treatment and developed symptomatic lateral hernias. Up to now, there is no evidence to suggest that laparoscopic management is better than open in the context of late repair 21.
With respect to the materials used for the repair, most of the reconstructions are with polypropylene mesh to cover the defect and few with large biological meshes. Other authors close the defect with sutures or mesh strips9. In one case, approximation of the lateral wall muscles was successfully performed with suture anchors22. In case reports or small series in which no mesh was used (the largest study is 280 patients), the recommendation is to use a mesh, preferably polypropylene, to perform abdominal reconstruction23.
Conclusion
The case presented is unique in its kind because the consolidation in an anomalous position of the most cephalic portion of the iliac bone prevented the reinsertion of the muscles with the techniques described, since it was displaced anteriorly, laterally and caudally. The polypropylene mesh placed in the preperitoneal plane did not have adequate coverage, since the skin that was overlying the defect. The mesh had been expanded by the hernia and thinned and had little subcutaneous fatty tissue. Being a young patient who previously worked in bodybuilding and with little fatty tissue, the risk of the mesh eroding the skin and exposing was latent, so the solution was to take the fascia lata graft to cover the skin mesh and at the same time give continuity to the abdominal wall, the result was successful.
Due to the low incidence of these hernias, systematizing management is complicated; however, the best time to perform the procedure must be recognized, taking into account that by performing it early, the probability of reinserting the muscles, with the chosen technique, is more likely to be successful. The use of mesh in early reconstructions is limited by contamination of the abdominal cavity in cases of intestinal lesions, leaving the management of these patients for late reconstructions, which is valid and with good results.
The management of this pathology must be individualized and the best option chosen taking into account the injuries caused by the trauma, without fearing to leave the abdominal reconstruction in a second stage in case of presenting other injuries that endanger the patient’s life or compromise the result. A case report is statistically limited, however, the technique is considered innovative since up to now there are no case reports in which an autograft is used to cover the mesh in the reports found in the literature.











 nueva página del texto (beta)
nueva página del texto (beta)