Introduction
Swallowing is a sensorimotor act involving a diverse neural network, which requires coordination of cortical and brainstem regions for the safe and efficient transport of liquids and food from the mouth to the stomach1-3. Swallowing disorders are a medical disability that affects the digestive system and is associated with increased mortality and health-care costs, without the psychosocial consequences that this generates on patients, such as depression and isolation4-8. These functional disorders are usually due to alterations in the physiological processes of the oral and pharyngeal phase of swallowing, including the reflex of absent swallowing, reduced peristalsis and pharyngeal pressure, and coordination problems due to the reflex of late swallowing8-12.
Acute, subacute, or chronic interruption of arterial blood flow in any spinal territory commonly developed medullary ischemia (anterior and posterior spinal artery syndrome) or stroke; and less prevalent transient ischemic accidents (TIAs), spinal claudication, and hypoxic-ischemic myelopathy from global hypoperfusion13,14.
Approximately 25-50% of stroke patients experience dysphagia. In comparison, the incidence increases exponentially in patients with lateral spinal infarction with about 51-100%, as significant swallowing centers such as the ambiguous nucleus and solitary tract are found in the dorsolateral spinal bulb14-16.
Wallenberg syndrome, the most common cause of lateral spinal infarction, is also known as posteroinferior cerebellar artery syndrome caused by damage to the lateral segment of the posterior marrow to the lower olive nucleus17,18. There is no exact described prevalence of this syndrome; in the United States, approximately 800,000 people have an acute stroke each year, 20% occur in the posterior circulation, leading to an estimated 60,000 new cases of Wallenberg syndrome each year19. Its primary etiology is given by atherothrombotic occlusion of the vertebral artery and the posteroinferior cerebellar artery. The main most prevalent risk factor is hypertension followed by smoking and diabetes20,21. Dysphagia has been reported in 51-94% of these patients; in most cases, it is initially severe but often improves rapidly. However, some patients may not recover in months or years21. Patients with the complete syndrome are rare, have Horner syndrome, cross hemisensory alteration, and ipsilateral cerebellar signs such as vertigo, central nystagmus, dysarthria, and dysphagia22,23.
Although Wallenberg syndrome has a broad clinical spectrum, swallowing disorders are a common finding in these patients; unfortunately, swallowing disorders related to Wallenberg syndrome have been described only as case reports or in limited patients. This article describes the characteristics of the spectrum of oropharyngeal dysphagia presentation in patients with Wallenberg syndrome and our experience within a national reference center.
Methodology
We describe eight patients with ischemic spinal injury treated in the Phoniatrics Department of the General Hospital of Mexico “Dr. Eduardo Liceaga.” The series of cases were conducted from January 2016 to November 2020, including patients between 18 and 80 years, with magnetic resonance imaging of the skull showing lateral spinal ischemic injury plus swallowing evaluation with the Fiber-optic Endoscopic Evaluation of Swallowing (FEES) twice, the first during hospitalization and the second after discharge. The swallowing was assessed in the oral and pharyngeal phases through four textures in the following order: pudding, nectar, liquid, and solid (cookie), mixed with blue dye to improve visualization. The FEES protocol consisted in administer 2.5 ml of pudding with an increase to 5 ml in case of no aspiration, followed by nectar and water at the same volumes mentioned; finally, 1/4 cookie was offered as solid. The protocol was modified for patient safety, stopping the test if at any time patients had intrusion to the airway. Aspiration was defined as the passage of food to the lower airways, below the vocal folds. Penetration was defined as the entry of food into the larynx above the vocal folds; and pharyngeal residue as the residual material presents in the pharynx after completing the pharyngeal phase of swallowing11,22,23. The severity of dysphagia was classified as mild, moderate, and severe, based on O’Neil’s severity scale24,25.
Results
We included eight patients, four women and four men, randomly caught, aged 28-74 years (average 40 years). Six of the patients (75%) suffered from high blood pressure, one patient had alcoholism (12.5%), and three had a smoking habit (37.5%).
With respect to the magnetic resonance imaging, the T2-weighted sequence shows four patients with lesion with low signal intensity in the right lateral medullary area (Fig. 1A), three patients with the left lateral lesion (Fig. 1B), and one last patient had two hypointense areas, one right upper and anterior medulla and the other in the left lateral and posterior medulla (Fig. 1C).
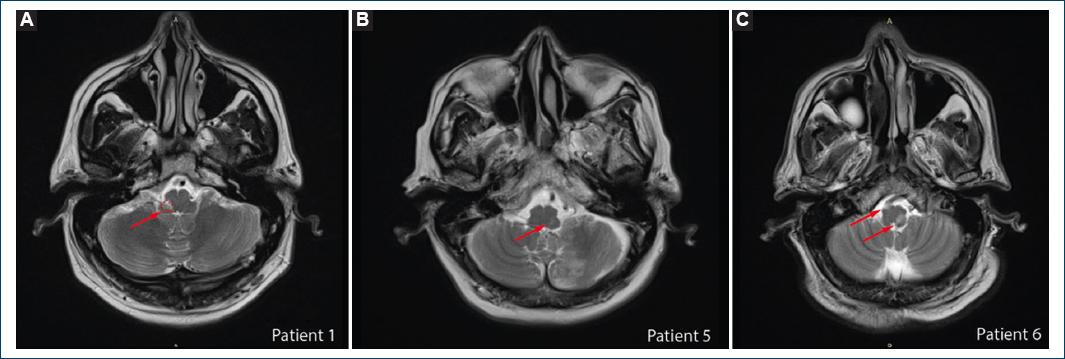
Figure 1 T2-weighted magnetic resonance imaging (MRI). A: demonstrating a hyperintense lesion in the right lateral and posterior medulla. B: demonstrating a hyperintense lesion in the left lateral and posterior medulla. C: demonstrating two lesions, one hyperintense lesion right upper and anterior medulla and other in the left lateral and posterior medulla.
Concerning the characteristics of the oral phase FEES study in the first evaluation, we found five patients had difficulty bolus propulsion, six posterior spill, and two patients had delayed reflex swallowing, finding more than 1 alteration in one patient. However, in the second evaluation, the oral phase was described as normal in all the patients.
The pharyngeal phase in the FEES study demonstrated in the first evaluation was tolerated by the eight patients who could handle the survey in the passage of pudding, seven nectar consistency, three patients achieved liquid texture, and none could be evaluated for solid. In the second evaluation, all patients were evaluated with nectar and pudding; six patients achieved liquid consistency and one to solid texture. Aspiration was found in seven of eight patients at the first evaluation (Fig. 2), this number was reduced to two of eight patients at the second evaluation.
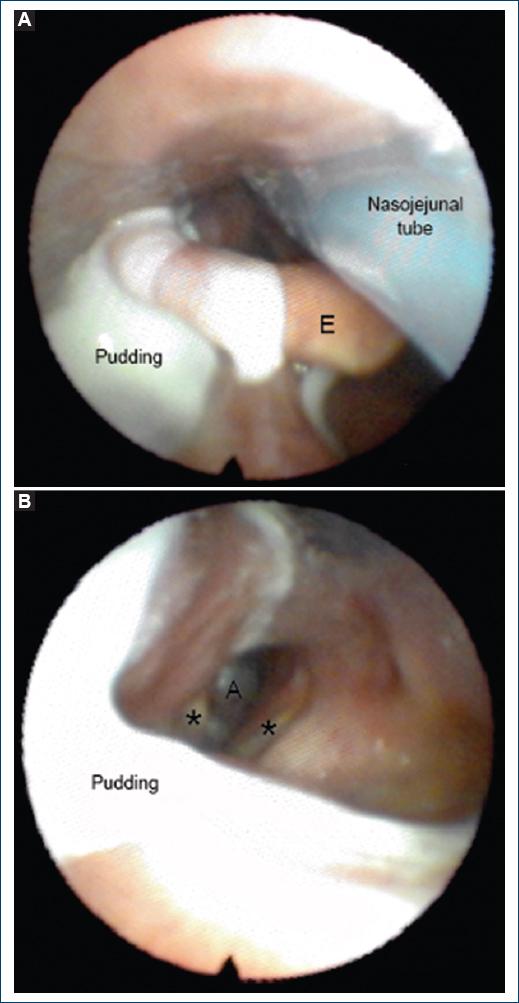
Figure 2 A-B: fiber-optic Endoscopic Evaluation of Swallowing (FEES): penetration and aspiration of bolus. E: epiglottis; A: aspiration; *: vocal folds.
Phoniatric diagnosis in the first evaluation was severe oropharyngeal dysphagia in 7 of the 8 patients (87.5%). The other patient had mild dysphagia; one patient had left vocal fold paralysis, other patients with severe dysphagia had bilateral palsy, and one patient had flaccid dysarthria. Phoniatric diagnosis in the second evaluation was four patients with mild oropharyngeal dysphagia and four patients with severe oropharyngeal dysphagia; none of the patients had vocal fold paralysis. The individual characteristics of the patients and clinical evolution are mentioned in Table 1.
Table 1 Clinical evolution of patients included in the study
| Patient | Age | Gender | Days of evolution | Oral phase | Pharyngeal phase | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| difficulty bolus propulsion | Anterior spill | Posterior spill | Difficulty for bolus propulsion | Pudding | Nectar | Liquid | Solid | Delay reflex swallow | ||||
| 1 | 29 | F | 10 | Y | Y | Y | N | Normal | Aspiration (2.5 ml) | Not tested | Not tested | N |
| 2 | 28 | F | 30 | Y | Y | Y | N | Normal | Penetration (2.5 ml) | Aspiration (2.5 ml) | Not tested | Y |
| 3 | 74 | F | 30 | N | N | N | N | Postswallowing residue | Posdeglutory residue | Aspiration (2.5 ml) | Not tested | N |
| 4 | 44 | M | 365 | Y | N | Y | Y | Normal | Aspiration (5 ml) | Not tested | Not tested | N |
| 5 | 47 | M | 15 | N | N | Y | Y | Penetration (2.5 ml) | Penetration (2.5 ml) | Aspiration (2.5 ml) | Not tested | N |
| 6 | 62 | M | 60 | N | N | Y | N | Penetration (2.5 ml) | Aspiration (2.5 ml) | Not tested | Not tested | N |
| 7 | 36 | M | 60 | Y | N | N | N | Penetration (2.5 ml) | Aspiration (2.5 ml) | Not tested | Not tested | N |
| 8 | 56 | F | 7 | Y | Y | Y | Y | Aspiration (2.5 ml) | Not tested | Not tested | Not tested | N |
| Dx | 2nd evaluation (days after) | Oral phase | Pharyngeal phase | Dx | ||||||||
| Pudding | Nectar | Liquid | Solid | |||||||||
| 1 | Severe dysphagia + left vocal fold paralysis | 30 | Normal | Penetration (2.5 ml) | Aspiration (2.5 ml) | Not tested | Normal | Severe dysphagia | ||||
| 2 | Severe dysphagia + bilateral vocal fold paralysis | 15 | Normal | Normal | Normal | Penetration (2.5 ml) | Not tested | Mild dysphagia | ||||
| 3 | Mild dysphagia | 25 | Normal | Normal | Normal | Penetration (2.5 ml) | Not tested | Mild dysphagia | ||||
| 4 | Severe dysphagia | 30 | Normal | Normal | Penetration (2.5 ml) | Penetration (2.5 ml) | Not tested | Severe dysphagia | ||||
| 5 | Severe dysphagia + Flacid dysarthria | 27 | Normal | Penetration (5 ml) | Penetration (5 ml) | Penetration (5 ml) | Not tested | Severe dysphagia | ||||
| 6 | Severe dysphagia | 30 | Normal | Normal | Normal | Aspiration (5 ml) | Not tested | Mild dysphagia | ||||
| 7 | Severe dysphagia | 16 | Normal | Penetration (5 ml) | Penetration (5 ml) | Not tested | Not tested | Severe dysphagia | ||||
| 8 | Severe dysphagia | 29 | Normal | Normal | Normal | Penetration (5 ml) | Not tested | Mild dysphagia | ||||
Discussion
The typical signs and symptoms of Wallenberg syndrome are vertigo or dizziness, ataxia, nystagmus, Horner sign ipsilateral weakness of the palate and vocal folds, decrease in the gag reflex, and oropharyngeal dysphagia20,22,26,27, the last one is the least studied, nevertheless is a common symptom which can be found in 51-94% of patients14,28-30. All the patients studied in our center had swallowing disorders with a wide clinical spectrum as demonstrated.
Hypertension was comorbidity found in 75% of our patients; it is a common risk factor as seen in a cohort of acute ischemic stroke patients studied by Flowers et al. included 160 patients with a mean age of 66.7 years, of which 111 (69.4%) had hypertension31-35.
There are many studies regarding stroke related to dysphagia, but our study is the only one in which dysphagia is evaluated specifically at the time of diagnosis and after a month in patients with Wallenberg syndrome. Regarding the oral phase in the first evaluation, the trouble with bolus propulsion was observed in 5 patients (62.5%), posterior spill in 6 patients (75%), and 2 patients had delay reflex swallow (25%); but in the second evaluation, the oral phase improved to normal in all patients. With these findings, we could say that the oral phase has a fast recovery; there is poor information about the description or evolution of the oral phase in the literature to compare. Despite an apparent good recovery in the oral phase, combining these alterations with the observed in the pharyngeal phase at FEES means for the patient, especially during the 1st weeks of the disease, that at the moment of swallowing will be an action even more difficult. Furthermore, if alterations at pharyngeal phase are persistent, the degree of dysphagia will still be severe, passing the month after disease installation.
The literature says that the severity of dysphagia will depend on the extent of involvement of the swallowing-related structures in the infarct lesion because all the central control of the swallowing is located in the lateral medulla32,35-39. In our study, most of the patients do not follow the rule that says severity will depend on the location or extent, because even patients with right or left lateral lesions present the same evolution, and some patients with one lesion present better evolution than the patient with 6 with two different lesions.
Nearly, all the case reports of dysphagia related to Wallenberg syndrome mentioned that the evolution of the dysphagia will be toward improvement almost back to normal14,17,21,23. In our case, almost all the patients remained in severe dysphagia, and only three patients showed improvement.
The nucleus ambiguous controls the muscles of the palate, pharynx, and larynx so a lesion also results in vocal fold paralysis28,33,39. This, in addition to explaining the variation in the severity of dysphagia in our patients, could explain the two patients with vocal fold palsy.
Conclusions
The evolution of dysphagia related to Wallenberg syndrome could be more severe than expected, especially passing the 1st month after establishing the disease. Therefore, evaluation of dysphagia is essential, since a prompt diagnosis will allow their early rehabilitation reducing the risk of complications, such as aspiration pneumonia, malnutrition, and increased mortality4,6,40,41. Furthermore, patients follow-up should be more strict, given the apparent probability of maintaining severe dysphagia. The presence of other clinical findings like vocal fold palsies should be investigated, to offer an oriented therapy and rehabilitation. Because of being a rare syndrome, further studies describing the evolution of related dysphagia are needed to establish a long-term prognosis.











 nueva página del texto (beta)
nueva página del texto (beta)


