Introduction
The mediastinum is the anatomical compartment located in the center of the chest. Limited by both pleuras on their side faces, sternum and chondrocostal joints at the front and back by the anterior areas of the vertebral bodies and ribs. The lower limit is given by the diaphragm and the upper limit by the upper chest narrow. The anatomical division and the structures they contain are described in Table 1.
Table 1 Mediastinal anatomical division with its limits and structures containing
| Division | Limits | Structures |
|---|---|---|
| Anterior | Anterior: posterior sternum, Posterior: anterior pericardium margin, aorta y brachycephalic. | Timus Linfatic nodules Grease Internal Breast vessels |
| Medium | Anterior: posterior margin of the division anterior
subsegment. Posterior: anterior margin of posterior division. |
Heart and pericardium Aorta ascending and y transverse. Brachyphthalic vessels. Upper and lower cava vessels. Mains Pulmonary vessels and Bronchus. Lymph nodes and grease |
| Posterior | Anterior: pericadium. Posterior: pre-vertebral fascia and anterior longitudinal ligament. | Descending Aorta Esophagus Chest conduit Acigos and hemiacigos vein, autonomic nerves, Lymph nodes, grease. |
Case Report
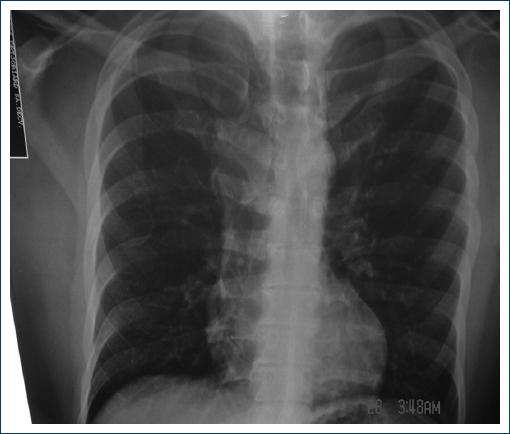
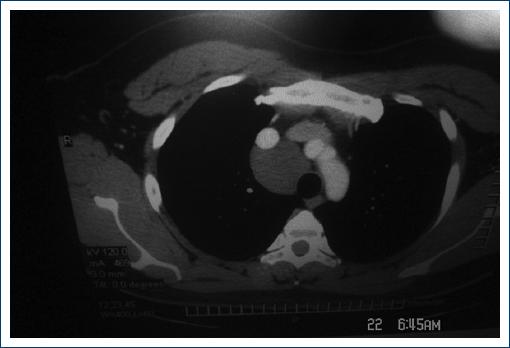
32-year-old male patient, Bachelor of Computer Science who goes to medical review at the company where he works for dizziness, cardiac arrhythmia that increased when lying left, face up and sitting so he is prescribed telmisartan 40 mgs., every 24 hrs. The Chest x-ray as a finding mediastinal widening of right dominance and based on this he was taken chest CT scan where a mediastinal cystic injury was demonstrated so it was proposed that it should be resection (Figs. 1-3).

Figure 2 Chest Tomografy. Mediastinal cystic between braquiocefalic arterial trunk and superior vena cava.
It was programmed for chest surgery through two ports, with the patient sedated in the seated position, without being intubated with nasal catheter at 3 liters per minute, it was proceeded to infiltative with local anesthetic combining 9 mls., ropivacaine at 7.5%, 9 mls., of xylocaine 2% with epinephrine and 2 mls. of sodium bicarbonate, 2 mls. for each intercostal nerve in the five and six intercostal space. Skin is inserted in five intercostal space is inserted chestscope observed which was punctured, to empty into its contents, pull it with a Gasper Clamp and cut almost completely leaving only a small part to attached to the mediastinum to vascular structures. He was left with a Nelaton 26 tube and the next day after chest x-ray, which showed total pulmonary re-expansion and no pleural effusion, the pleural tube was removed.
Discussion
Within mediastinum tumors, mediastinal cysts make up 20% of the masses affecting that space1. They usually occur as a mass in asymptomatic patients, identified in a chest screening x-ray, or with symptoms generated by the condition to the different mediastinal structures (hypoxia, facial swelling and acute respiratory failure)2. In the case presented the patient had symptoms when changing position, which caused the patient to go to the doctor.
The most common mediastinal tumors in adults are: thymo and thymic cysts (26.5%), neurogenic tumors (20%), other cysts (16.1%), germ cell tumors (13.8%) lymphomas (12.7%)1 (Table 2). In a series of 1814 cases of chest tumors reported at a third-level University Hospital in Mexico City, a ratio of 50.8% was made up of Bronchogenic Carcinoma, Pleuropulmonary Metastasis (39.1%), Mediastinal Tumors (7.3%), Pleura Tumors (1.9%) chest wall tumors (0.5%)3.
Table 2 Classification of mediastinun tumors
| Thymoma Benig Malignant |
Lymphoma Hodgkin×s disease Linfoblastic Lymphoma Large Cell Lymphoma |
| Germ cell tumors Teratodermoid (benign/malignant) Seminoma No seminomatous: Embryonic Choriocarcinoma Endodermic |
Primary Carcinomas Mesenchymatous tumors Fibroid/fibrosarcoma Lipoma/liposarcoma Leiomioma/leiomiosarcoma Rhabdomyosarcoma Xantogranuloma Myxoma Mesothelioma Hemanioma Hemangioendotelioma Hemangiopericitoma Lynfangioma Lynfangioperycitoma Endocrine tumors Intratoracic Thyroid Adenoma/carcinoma parathyroid Carcinoid |
| Cystic Broncogenic Pericárdial Entéric Thymic Chest duct No-specífic |
Giant lymph node Castelman×s Disease |
| Condroma Neurogen Tumors Neurofibroma Neurilemoma Paraganglioma Ganglioneuroma Neuroblastoma Chemodectoma Neurosarcoma |
Extramedullary Hematopoiesis |
Mediastinal cysts are a heterogeneous group of neoplastic, congenital and inflammatory lesions, rare in clinical practice and a number of them are found casually during a radiological examination by other indications3. They occur in both adult and child populations, and their classification is based on the cause3,4. In a series of 105 patients with mediastinal tumors at a University Hospital in Turkey, 34 cases were found that accounted for 33% of all tumors, with 94% congenital origin and 4% hydatid disease5,6, the latter perhaps because of the living conditions they have in that area of the world.
Primary mediastinal cysts probably correspond to embryonic developmental abnormalities in the proximal intestine region, at the time of separation of esophageal and pulmonary buds. They are characterized by the organ of origin and can be bronchogenic, pericardial, enteric, timid or nonspecific (Tables 3 and 4)7,8.
Table 3 Cyst Mediastinic Classification by location
| Anterior | Medium | Posterior |
| Mediastinum | Mediastinum | Mediastinum |
| Cystic hygromas | Cystic | Gastroenteriic |
| Cystic Tymus: | Pericardic pleura and pericardic | Cystic and duplications |
| Congenic and acquired | Bromchogenic Cystic | Neuroenteric cystic |
Table 4 Classification of common mediastinum tumors by anatomical compartment
| Anterior Mediastinum Thymic tumors Lymphomas Germ cell tumors Intrathoracic thyroid Intrathiracic parathyroid adenoma Mesenquimal tumors: lipoma, hemangioma. |
Medium mediastinum Adenopathies: benign or malignant Cysts pleuro-pericardic Bronchogenic Cystis |
Posterior Mediastinum Neuogenic Tumors Cysts/duplicatons hiatal or parahyatal esophageal hernial or gastroenteric. Esophageal diverticulosis Abscesses vertebral or paravertebral. Meningoceles Vertebral Metastasis Lung Abductions |
The bronchogenic cyst is a part of the tracheobronchial tree that is separated during the bronchial branching process and does not continue its development. Commonly rounded shape, thin and unique wall. It contains serous-mucous liquid, a few cases open to bronchi showing a hydro-air level inside9.
Followed in order of frequency, after bronchogenic cysts are pericardial cysts, which are located at the cardiophrenic angle, usually on the right side (70%), which may have communication with the pericardium and usually contain clear liquid, are smooth-edged and a water-like cystic liquid attenuation. Fine needle aspiration and routine follow-up are sufficient for handling3-7.
Enteric or duplication cysts derive from the anterior primitive intestine, which are usually attached to the esophagus and cause compression symptoms7,8,9.
Clinical presentation and diagnosis is sometimes complex, as symptoms lack specificity and most are mainly due to compression of adjacent structures, as was the case in this article. Dysphagia, weight loss, anorexia and cough make you think of underlying malignancies5,10-15.
Chest tomography is the technique of choice in the diagnosis of mediastinum tumors.
Cystic lesions generally show attenuation close to or greater than water density, solid lesions have greater attenuations than water, treatment in most cases tends to be complete resection or drainage of the injury16,17.
In the management of some lesions of the mediastinum it is possible to do so with the thorachoscopy technique and these, with the variant of two ports without intubating the patient, with which it is possible to address the chest, visualize the mediastinum and resectiont the lesions found, so we could say that it can be performed not in large injuries but in small lesions with the non-intubated patient, in well-selected cases or in patients at high surgical risk from general anesthesia and endotracheal intubation.
The pleurotomy tube is left to be able to observe the liquid or air outlet after the procedure, and may be removed the next day if the lung is inflated and there is no other complication18.











 nova página do texto(beta)
nova página do texto(beta)