Introduction
Appendicitis is the inflammation of the vermiform appendix and represents the most common cause of acute and emergency abdominal surgery in the world1.
Inguinal hernias represent the most frequent cause of abdominal wall defect. Nearly 75% of hernias occur in this region. Their incidence is approximately 15/1000 inhabitants; the lifetime risk of developing inguinal hernias is 27% for men and 3% for women2.
The use of mesh in inguinal hernia repair carries the risk of delayed rejection, migration, or foreign body-related infectious complications3.
The case of an 87-year-old male is presented here, who was diagnosed with acute appendicitis, probably complicated, and during exploratory laparotomy, a migrated prosthetic mesh was found, causing the appendicular condition, as a complication of a previous inguinal hernia surgery.
Case study
An 87-year-old male patient with a history of right inguinal hernia surgery that took place in 2012. He presented with a 4-day history of symptoms previously treated with antibiotics and non-steroidal anti-inflammatory drugs, diagnosed with urinary tract infection, with no improvement.
Physical examination revealed tachycardia, flat abdomen with absent peristalsis, with voluntary muscular resistance, depressible, McBurney's point and Rovsing's sign present, mild pain on palpation in the right flank, well localized, with no evidence of peritoneal irritation.
Laboratory studies were performed and found to be within normal parameters. In addition, a simple computed tomography scan of the abdomen showing an image corresponding to an enlarged appendix, free fluid, and plastron (Fig. 1). A diagnosis of acute appendicitis modified by medication was established and surgical intervention was elected
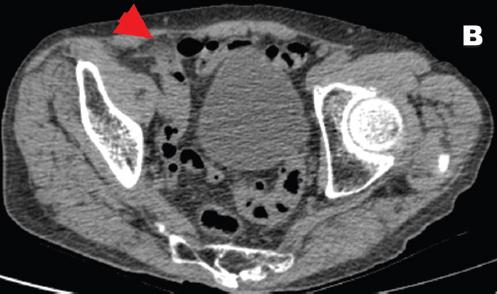
Figure 1 Computed tomography scan of the abdomen in cross-section showing the mesh eroding the parietal peritoneum, interpreted as a plastron (red arrow). No cecal appendix is identified.
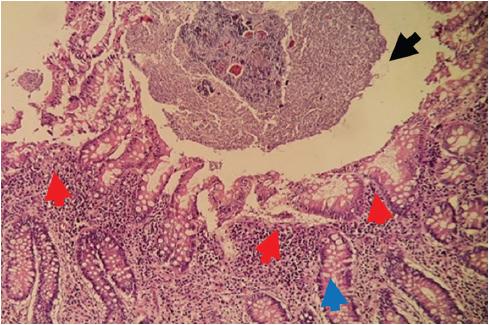
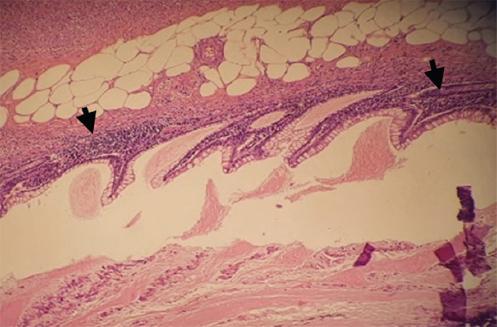
Exploratory laparotomy was performed, finding cone-shaped surgical mesh eroding the parietal peritoneum, with adhesions to the omentum, cecum, and cecal appendix (Fig. 2). A 10x1 cm erythematous, edematous, and hyperemic cecal appendix, with the presence of appendicolith at the tip. Finally, an appendectomy was performed by dismantling the surgical mesh cone and closure of the peritoneum. The mesh was placed using the Lichtenstein technique in its entirety. The patient evolved favorably and was discharged 24 h after surgery. Pathology revealed cecal appendix with reactive lymphatic hyperplasia and passive congestion (Figs. 3-5).
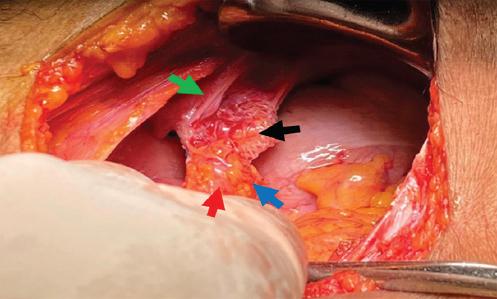
Figure 2 Surgical mesh (black arrow) eroding parietal peritoneum (green arrow), cecal appendix (red arrow), and mesoappendix (blue arrow).
Discussion
Inguinal hernia repair remains a challenge for the surgeon due to the frequency of complications, which occur in all techniques described so far. They range from pain at the incision site to migration with bowel occlusion4,5. Although the patient was unaware of the technique used in the previous inguinal hernia surgery, the finding of a cone-shaped mesh suggested a Rutkow and Robbins technique.
The Rutkow and Robbins technique for the repair of inguinal hernias was introduced in 1989 by these authors, based on the Gilbert technique. From 1989 to 2003, they performed this technique in 4404 patients, of whom < 1% presented recurrence, with a notable decrease in postoperative complications and early return to work6. Some studies report similarities with the classic Lichtenstein technique in terms of immediate and intermediate post-operative results7. However, relevant complications associated with mesh migration regarding the Rutkow and Robbins technique have been reported, such as chronic pain, bowel occlusion, intraperitoneal meshes, and adhesion to intraperitoneal structures such as the iliac vein, deep vein thrombosis due to fibrosis around the vessel, recurrence with migration to the scrotum, and small bowel fistula.4,5,8-11.
Mesh migration can be divided into primary and secondary migration. Primary migration consists of mesh movement over pathways of least resistance into contiguous anatomical spaces, due to either inadequate mesh fixation or external forces. Secondary mesh migration consists of slow, gradual movements of the mesh across trans-anatomic planes and is secondary to erosion induced by foreign body reaction. This depends on the nature of the mesh biomaterial and the type of fixation. Thus, the mesh may initially be displaced and subsequently erode adjacent tissue4,11.
Since the anatomopathological findings do not coincide with the time of evolution of the clinical condition, it can be assumed that the symptoms were secondary to the erosion of the cecal appendix by the migrated mesh, with subsequent histological changes, thus being a primary type of migration.
The relevance of this clinical case lies in the infrequency of this complication, as there are a limited number of similar cases reported in the literature. Visceral complications associated with mesh migration are considered rare and their publication occurs only as a case report. Some authors consider that these complications are not so uncommon and represent only the tip of the iceberg, both in open and laparoscopic surgeries. Hence, it is difficult to define which technique is most associated with these complications4.
In 2019, Gossetti et al. conducted a literature review of case reports of visceral complications associated with mesh migration, finding in 97 cases that the highest incidence was related to laparoscopic repair, and the lowest to the Lichtenstein technique4.
Further serial studies on long-term complications associated with this technique are needed to determine its true usefulness and develop modifications to reduce their incidence, as there are still insufficient literature and reported statistics.











 nueva página del texto (beta)
nueva página del texto (beta)