Introduction
Neuroblastomas are malignant tumors derived from cells of the primitive neural crest, they represent the fourth most common extracranial malignant tumor in childhood1, approximately 90% of patients present them before 5 years of age, while being extremely rare during adulthood, especially after the third decade of life2, with an incidence of 0.12 cases/million3, and equal distribution among female and male adults4. Reports on adult-onset neuroblastomas can be found in large electronic registries such as the Surveillance, Epidemiology, and End Results (SEER) and the International Neuroblastoma Research Group (INRG) databases. The SEER database, between 1973 and 2002, identified 144 patients ≥ 20 years old at diagnosis, accounting for 6.1% of all neuroblastoma patients (n = 2054). The INRG database identified 200 patients (2.3%) between ages 10 and 21 years, from 1990 to 20024.
When found in adults, symptoms are non-specific4 often delaying diagnosis, besides, laboratory tests are usually normal, and imaging studies show an undetermined adrenal mass, which may be a functional or non-functional adenoma, pheochromocytoma, adrenal carcinoma, sarcoma, T4 renal tumor, and metastasis, among others, therefore wrongful diagnosis is easy to conjecture. The latter is highly relevant because diagnosis is often delayed and disease stage determines the prognosis.
Case report
A 35-year-old female, without medical history, seeks medical consultation at the emergency department with intermittent, 3-month, mild left lumbar pain, with irradiation to ipsilateral thigh. Contrast-enhanced abdominal computed tomography (CT) was performed (Fig. 1), finding a large, lobulated, solid left adrenal mass with heterogeneous enhancement. Blood analysis excluded a functional adrenal tumor.

Figure 1 Contrast-enhanced abdominal computed tomography showing. A: axial view of a heterogeneous retroperitoneal large mass (measuring 15 × 14 × 12 cm). B: giant adrenal mass crossing the midline and displacing adjacent organs and vessels seen in a sagittal view.
The patient underwent left open radical adrenalectomy without complications. Pathology report: 14 × 11 × 10 cm tumor, 1100 g, poorly differentiated neuroblastoma, positive lymphovascular invasion, with non-disrupted capsule (Figs. 2 and 3) confirmed by immune histochemical assay (Table 1).

Figure 2 A: surgical specimen. B: hematoxylin and eosin stain ×10, confined malign neoplasm of neuroblastic origin, composed of cell nests surrounded by fibrous septa.
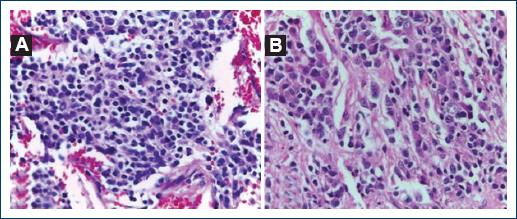
Figure 3 A: hematoxylin and eosin (H-E) stain × 40, cellular characteristics are identified, a large number of neuroblasts are seen at different stages of cellular maturation, ranging from small cells with salt and pepper nucleus to larger cells with an eccentric nucleus and a prominent nucleolus as well as abundant eosinophilic cytoplasm. B: H-E stain × 40, a large number of neuroblasts are seen in different cellular maturation stages in addition to neuropil.
Table 1 Immunohistochemical assay result confirms neuroblastoma diagnosis. immunohistochemical assay
| Antigen | Result |
|---|---|
| Synaptophysin | Positive |
| Chromogranin | Positive |
| Ki67 | Positive |
Metaiodobenzylguanidine single-photon emission CT/CT was performed at 6-month follow-up (Fig. 4), no local recurrence or metastasis found.
Discussion
Very rarely, neuroblastomas can be diagnosed in adults2. Teenagers and adults with neuroblastoma have a worse outcome than children5.
As in the case described above, symptoms are typically non-specific, with back and abdominal pain being the most common4. Persistence of these symptoms especially in young adults without relevant medical history, as our patient, should be followed by appropriate imaging studies in an attempt to make an appropriate diagnosis. Laterality of the mass, its size, and the presence of calcifications can be observed by abdominal CT, the latter are seen in 80-90% of cases6, although heterogeneous enhancement was found in our patient, no calcifications were identified. As compared to children, a higher proportion of adults have metastatic disease at diagnosis: 75%, whereas in children, only 40-55% have Stage 4 disease at diagnosis7. This might be related to the delay in diagnosis of adult-onset neuroblastoma. Although our patient presented with a huge tumor, no metastases were found.
Amplification of MYCN oncogene, mutations in anaplastic lymphoma kinase, and segmental chromosomal alterations are genetic alterations that can be found in neuroblastoma cells8. Definitive diagnosis requires histopathological examination, the finding of sheets of Homer-Wright pseudorosettes, consisting of neuroblasts surrounding eosinophilic neuropil, is a pathognomonic feature9. Differential diagnosis of large retroperitoneal masses includes retroperitoneal sarcoma, adrenal myelolipoma, retroperitoneal teratoma, and mesenchymal tumors.
A study by the Memorial Sloan Kettering Cancer Center analyzing the largest follow-up cohort of neuroblastoma in adults was carried out between 1979 and 2015, including 44 adult patients, between ages 18 and 71 years. Patients were classified according to the International Neuroblastoma Staging System (INSS), five patients were classified as Stage 1, 1 as Stage 2, 5 as Stage 3, and 33 as Stage 4. The study revealed that locoregional disease (INSS Stages 1, 2, and 3) had a 10-year progression-free survival (PFS) of 35.4% and an overall survival (OS) of 61.4%; while patients with metastatic disease (INSS stage 4) at diagnosis had a 5-year PFS of 9.7%, being statistically significant3. For those patients with localized, resectable disease, surgical resection alone is usually curative, and chemotherapy is an effective salvage therapy for those with relapse after resection7. Furthermore, the COG P9641 study demonstrated a 5-year OS rate after surgical resection alone of 99% for patients with INSS Stage 1 and 96% for those with asymptomatic INSS 2A or 2B tumors10.
Taking into account that our patient was classified as INSS Stage 1 (low risk), we should expect a favorable prognosis in the short and medium term. Both, clinical suspicion and carrying out an adequate and complete diagnostic work-up are of utmost importance considering that prognosis is determined by tumor stage and presence of metastases, and when feasible, surgical resection is the treatment of choice.











 text new page (beta)
text new page (beta)



