Introduction
In adults, popliteal artery aneurysm is the second most common type of peripheral arterial aneurysm after aortoiliac aneurysm. Atherosclerosis is its most common etiology, while less common causes include trauma, congenital popliteal aneurysm, mycotic aneurysm, and inflammatory arteritis1. While 70% of peripheral aneurysms in the adult population are popliteal, the prevalence within the pediatric population remains at only 1%2. Non-traumatic arterial aneurysms in the pediatric population are very rare and usually associated with inflammatory or degenerative conditions3. The most frequent location is the thoracic or abdominal aorta, being rare in other locations4. Peripheral aneurysms and pseudoaneurysms have been described in patients with inherited connective tissue diseases that weaken the structure of vascular tissue, such as Ehlers-Danlos and Marfan syndrome5. Aneurysm formation is also described in cases of trauma or in diseases such as fibromuscular dysplasia, osteochondroma, infection, and vasculitis6-8. However, isolated idiopathic popliteal artery aneurysms are exceptionally rare in the pediatric population. If surgical repair is not performed, popliteal artery aneurysms can lead to several severe complications. This is the sixth case reported and the youngest patient.
Case report
A 5-year-old male patient, a 1st-time pregnancy offspring, mother was 18 years old at the time. No complications during gestation and born at term by caesarean section due to cephalopelvic disproportion; presenting clinical signs from the age of 3 months, with alterations in the morphology of the right lower limb such as an increase in the diameter of the limb, purplish coloring, and dilation of the venous system, becoming visible. The first study performed was an arterial and venous Doppler ultrasound of the lower limbs; no pathological findings were found, but the result was not compatible with the patient’s clinical condition. Other extension studies were considered necessary to guide the diagnosis and explain the anatomical alterations present in the patient’s limb.
When the patient was 2 years old, computed tomography angiography (CTA) of the lower limbs was performed, which reported fusiform dilatation of the right popliteal artery in length at 47 mm, anteroposterior and transverse diameter of 12 × 11 mm and permeable, aneurysm only affects the popliteal artery. The patient was followed up periodically at an outpatient clinic.
At 5 years of age, patient underwent another CTA, confirming the existence of popliteal aneurysm, without significant variations in the size of the aneurysm described (Fig. 1); the patient was admitted to the institution referred by his attending physician, who reported an increase in the perimeter of the limb involved in the previous year. Physical examination revealed a congestive, purplish-colored right lower limb with increased circumference, distal pulses present, popliteal pulse more evident than the left, with no gait disturbance, or intermittent claudication (Fig. 2).
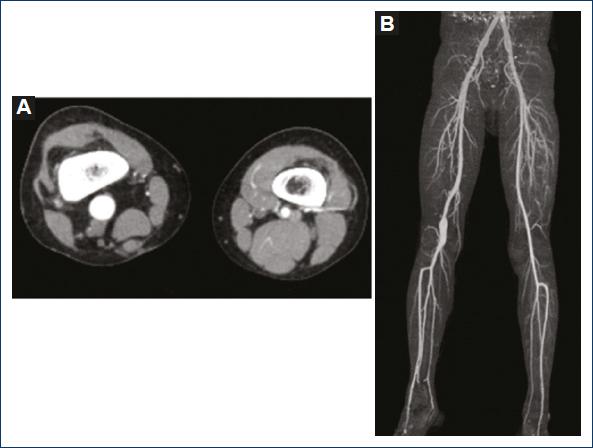
Figure 1 A: computed tomography angiography (CTA) of lower limbs, cross-section showing difference in diameters between the right popliteal artery and the normal left popliteal artery. B: 3D reconstruction of lower limb - CTA.

Figure 2 Right lower limb with purplish discoloration, visible superficial venous system, and increased circumference.
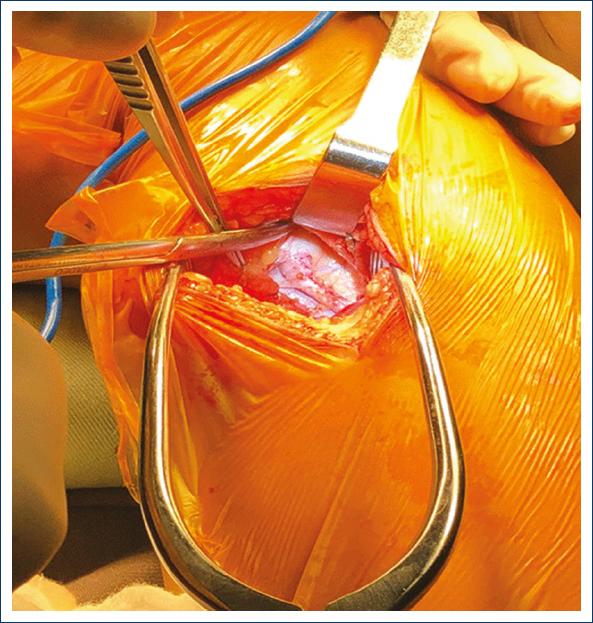
During the surgery, a longitudinal incision was made in the inner side of the left thigh to extract the supragenicular left greater saphenous vein, which was prepared as a bypass graft. A longitudinal incision was made in the distal third of the right thigh, medial aspect along the anterior edge of the sartorius muscle, on the lower edge of the vastus medialis muscle. Adequate visualization was achieved without releasing muscle bundles, dissection, and repair of the supragenicular right popliteal artery, identifying the start of the aneurysm (Fig. 3). Similarly, a longitudinal incision of 1-2 cm was performed posterior to the medial edge of the tibia. Dissection and repair of the same artery at the infragenicular level. Tunneling was performed inferior to the muscle fascia to interpose reversed greater saphenous vein between the popliteal segments described (Fig. 4). Proximal and distal veno-popliteal end-lateral anastomosis was performed with continuous Prolene stitches (7:0), thus completing popliteal bypass9. Proximal and distal ligation of the popliteal aneurysm was performed. Hemostasis was also performed with teseel 4 ml, and a sample of the aneurysm was obtained for pathological study. It was decided not to conduct total resection of the aneurysm as it would result in increased surgical time, risk of injury to surrounding structures, the need to release muscle bundles and because it would not bring benefits to the patient.
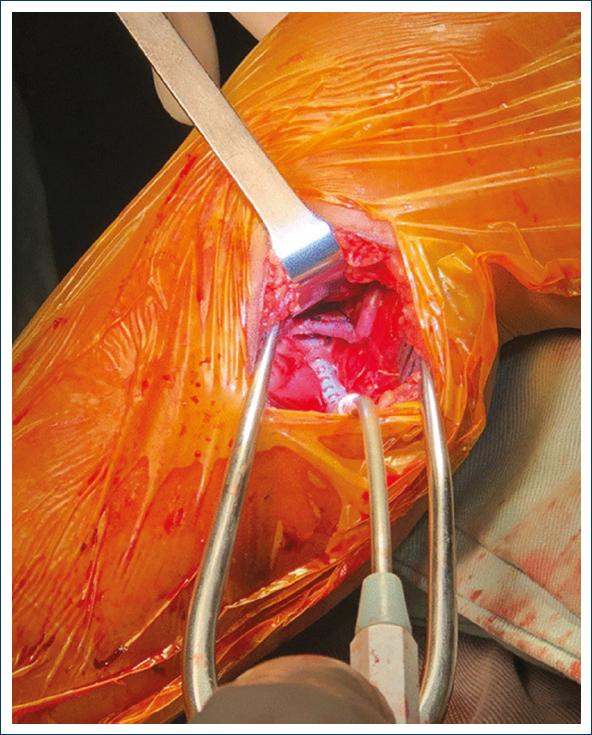
Figure 4 Bypass with redundant reverse great saphenous vein, considering the normal growth of the patient and therefore of the limb, prolonging the life of the bypass.
The patient evolved satisfactorily in the immediate postoperative period at the pediatric intensive care unit, where recovery protocols continued and 2 days after surgery patient was transferred to the hospital ward. On physical examination, the pediatric pulses were present, capillary filling and temperature of the extremity were preserved, the gait was antalgic and there were no alterations in mobility.
Finally, the pathology report of the biopsy taken from the aneurysm does not describe any pathological findings.
Discussion
Arterial aneurysm is defined as an abnormal dilation of a blood vessel. A true aneurysm involves symmetrical dilation of all three layers of blood vessels while preserving the histological structure. When a diagnosis of an aneurysm is made, a complete work-up of abdominal aneurysms or additional aneurysms of the extremities should be performed. False aneurysm, or pseudoaneurysm, is a solution of continuity of an arterial structure, which is contained. Pseudoaneurysm is caused by a rupture in the arterial wall, which leads to extravasation of blood into the surrounding connective tissue and usually follows injury or iatrogenic trauma. Both true and false aneurysms can occur in any blood vessel in the body, although they are most common in the central and intracranial major vessels10.
True aneurysms are commonly caused by atherosclerosis and hypertension; however, this only applies to the adult population10. In 1991, the clinicopathological classification of nine categories of arterial aneurysms in pediatric patients was published: (I) arterial infection; (II) giant cell arteritis; (III) autoimmune vasculitis; (IV) Kawasaki disease; (V) medial layer degeneration (Ehlers-Danlos or Marfan syndrome); (VI) other forms of medial layer degeneration; (VII) arterial dysplasia; (VIII) idiopathic congenital factors; and (IX) extravascular events leading to pseudoaneurysm11. Following this classification, the aneurysm of the patient under study was classified as type VIII, since he had no family history of connective tissue diseases, autoimmune vasculitis, history of trauma, and rheumatic fever or Kawasaki disease. This includes both signs and symptoms. In addition, no other aneurysmal lesion was evidenced in the extension studies. The pathology report of the biopsy taken from the aneurysm does not describe pathological findings, so it is compatible with this classification.
Aneurysms may manifest as asymptomatic or present as a pulsatile mass with shivering, local pain and ischemic pain10. In this case, the patient presented with venous congestion, visible superficial venous system and edema with increased circumference of the right lower limb with respect to the contralateral limb, clinical signs that had not been reported in the cases previously described so far in the literature3,4,8,12,13.
Diagnosis is made by clinical examination and complementary tests such as echo-Doppler, angiography, computed axial tomography or magnetic resonance angiography. Possible complications include rupture of the aneurysm, distal thrombosis, which can lead to loss or delayed growth of the limb, indicating that it should be managed surgically10.
Cases reported in the literature on true idiopathic popliteal aneurysms in children are very rare3,4,8,12,13. To the best of our knowledge, there are only five cases worldwide, two of which occurred in adolescent patients12,13. Of the five cases, one was repaired with a vascular prosthesis, which was motivated by aesthetic reasons, taking into account that the use of the greater saphenous vein for the shunt required an additional incision, altering the appearance of the contralateral limb12. However, the other cases have been performed with reversed greater saphenous vein, bearing in mind the technical considerations described in the literature, which emphasize the disadvantages of vascular prostheses, highlighting the deficiency in patency rates due to the lack of endothelium. This rate decreases as the length of the vascular prosthesis increases, which is counterproductive in pediatric cases, as it is recommended to perform the shunt with an additional length to favor adaptation to the patient’s growth, in addition to the risk of lifelong infection that is considered with these grafts11. Conversely, there are case reports describing durability of up to 44 years in bypasses, using greater saphenous vein in pediatric patients14; therefore, the use of greater saphenous vein grafts is argued based on their correct adaptation of the bypass to the growth of the limb and longer useful life than the synthetic vascular prosthesis.
In this case, the greater saphenous vein of the contralateral limb was taken because of venous congestion in the affected limb, which increases the risk of bleeding.
Endovascular repair of popliteal aneurysm with stenting is one of the most widely accepted surgical alternatives in recent years in the adult population; however, there are no reported cases of this technique in pediatric patients. Children, due to their high physical activity, perform extensive skeletal movements that could constantly produce exaggerated bending and twisting of the stent15. Therefore, it would be a risk to use stents in infants, given the imminent danger of stent fracture, increasing the likelihood of reoperation for stent repair.
Only in one of the five previously known cases, separate stitches were used for the anastomosis, following the technical considerations of vascular surgery in the pediatric population mentioned above, where they also suggest absorbable suture to allow better radial growth of the intervened vascular structure11. A hypothesis that has not been supported by studies in the literature; in the other cases of idiopathic popliteal artery aneurysm in the pediatric population mentioned, anastomosis was performed with non-absorbable suture and using continuous stitches, obtaining good results3,4,12,13.
In the cases reported in the literature, aneurysm resection is performed3,4,12,13. However, in the present case, it was decided not to perform such resection and it was managed with proximal and distal ligation, following the conduct taken in other cases reported in the literature8, seeking to obtain a shorter surgical time, less risk of injury to surrounding structures, and avoiding the need to release muscle bundles.
The present clinical case is relevant for several reasons; the first is the low frequency of this condition in the pediatric population, with scarce and limited information in the medical literature for its management, with a clinical presentation not previously reported and from a very early age. In addition, the importance of exhaustive anamnesis, thorough physical examination and an adequate diagnostic imaging study is emphasized, allowing for differentiation of this condition from other vascular pathologies. Finally, the aim was to highlight the surgical variations during management, considering those used in the cases already published; thus, widening the window of possibilities for progress in the treatment of these patients. Furthermore, depending on the clinical evolution, to document the long-term benefits of these modifications, considering the growth of the limb, the behavior of the bypass and the absence of complications, improving the patient’s living conditions, allowing us to propose this technique as the most appropriate for the management of this pathology, which is still under study at present.











 nueva página del texto (beta)
nueva página del texto (beta)