Introduction
Vascular trauma remains a major cause of morbidity and mortality in both civilian and military populations. These injuries constitute 3% of civilian injuries and about 7% of combat-associated trauma. Early recognition of vascular injuries is essential for immediate management. When delayed, it can cause irreversible ischemic injuries that may result in impaired function or loss of limb. Associated orthopedic and nerve injuries contribute as an additional factor to morbidity and mortality in patients with vascular trauma1. It is recognized that patients with extremity injuries and hard signs of arterial injury should undergo immediate surgery without imaging, except in certain situations (shotgun wound and multilevel fracture of an extremity). Hard signs include the following: external bleeding; a rapidly expanding hematoma; any classic signs of arterial occlusion (weak or absent pulse, pallor, paraesthesia, pain, and paralysis); and a palpable murmur. In 1906, Spanish surgeon J. Goyanes used the saphenous vein for an aneurysm of the popliteal artery. Since then, reverse autologous saphenous vein graft from an uninjured lower extremity has been the interposition graft of choice to replace segmental defects in peripheral arteries. The reasons are that the saphenous vein is a readily available endothelial conduit, it can be retrieved in one segment in 5-10 min in individuals of reasonable size, and the size fits most peripheral arteries. Denudation of 60-70% of endothelial cells occurs within 48 h. However, re-endothelialization is 80-90% complete within 4 weeks and 100% complete by 6-8 weeks. Both short- and long-term results with the use of saphenous vein grafts placed in the peripheral arteries of young trauma patients are excellent2.
Case report
Male patient
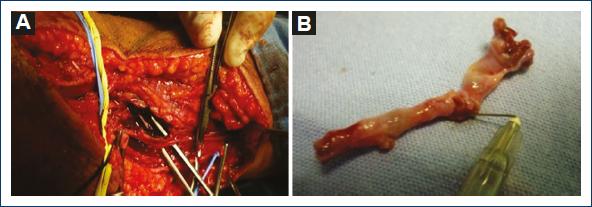
Patient with a case of gunshot wound to the right arm that occurred 1 month before. Since then, he reported paraesthesia in the fingers of his right hand and a drop in temperature. He was assessed at a family medicine unit in a community in Oaxaca and sent to a hospital in Mexico City. The patient was seen at the outpatient clinic of the hospital, where he was referred to the orthopedic service for a suspected fracture of the arm. On reviewing the orthopedic films, the patient was referred to the angiology service, which, on physical examination, observed gunshot wounds in the upper third of the external lateral face of the right forearm, healed as an entrance wound with an exit wound in the lower third of the internal lateral face of the arm with a healed wound. It also revealed increased volume in the elbow with ecchymosis, absence of radial and ulnar pulses, hand pallor, and distal hypothermia (Fig. 1). Doppler and duplex ultrasound was performed, where a total section of the humeral artery with collateral flow was reported. The patient was admitted for arteriography, which reported a lesion of the right humeral artery with flow through collateral circulation, permeable ulnar and interosseous arteries, and absence of flow of the radial artery (Fig. 2). A vascular exploration was scheduled for an inverted S incision on the humeral artery with extension to the forearm, locating extensive hematoma infiltrated in muscle tissue, humeral artery with irregularities in its wall, secondary to firearm burns, 50% laceration of the arterial wall with intra luminal hematoma without palpable flow (Fig. 3). After verifying good proximal humeral flow by thrombectomy with Fogarty catheter 4 and distal with Fogarty catheter 3 with excellent reflux of the distal humeral artery, a reversed saphenous vein graft was placed. Once the procedure was finished, the patient recovered proximal and distal pulses and was sent to the orthopedic unit to continue management of the bone lesion (Fig. 4). Post-operative management continued with unfractionated heparin with a timetable after discharge from the orthopedic unit and was managed with platelet antiaggregants for 3 months. Patient's evolution was satisfactory, medication was suspended, and he was discharged due to improvement.
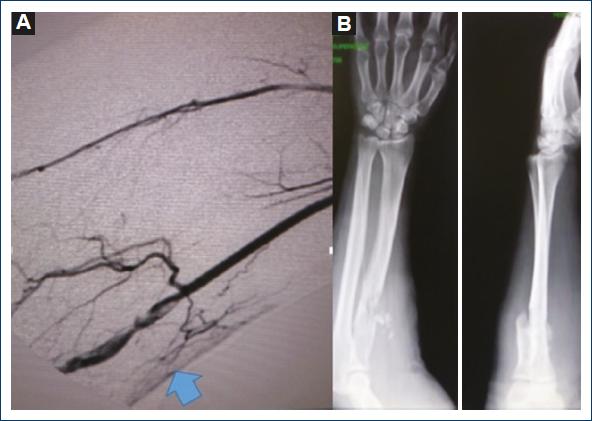
Figure 2 A: arteriography of the humeral artery with occlusion and lesion of the intima with collateral circulation. B: fracture of the upper third of the right radius.
Discussion
Although relatively uncommon, upper extremity arterial injuries are serious and have the potential to significantly impact trauma patient outcome. If not managed or treated promptly, such injuries can lead to limb loss or death. Because the duration of ischemia is critical to the overall outcome, arterial repair usually precedes orthopedic stabilization to restore limb circulation. Before final wound closure of the orthopedic procedure, vascular reconstruction should be inspected to verify patency of the repair. An exception to this in surgical sequence is when external fixation is required immediately to stabilize the brachial arteries normally repaired to maintain the limb after massive musculoskeletal trauma. Brachial arteries are normally repaired to maintain the blood supply to the arm. Rapid diagnosis by physical examination and imaging, when necessary, together with early restoration of blood flow were critical aspects of the vascular surgery protocol contributing to the limb salvage rate, absence of morbidity and avoidance of functional deficit caused by arterial injury3. Firearm injuries in the civilian population are becoming increasingly serious due to the use of high velocity projectiles. The present case helps us to re-evaluate those patients with vascular trauma with proximity of the injury to a vessel plus bone fracture, which in its initial stages, can pass as asymptomatic, thanks to collateral circulation. In these cases, observation and extension studies are of paramount importance.
Some patients may present with "soft signs" of vascular injury, which refer to a non-expansive hematoma, history of arterial bleeding, proximity of the wound to an artery, and neurological deficit. The ankle-brachial index (ABI) or arterial pressure index (API) can be used as an adjunct to physical examination for rapid triage of patients without hard signs of vascular injury. This is useful in situations where physical examination is equivocal or where practitioners with varying levels of experience are performing the physical examination4. A fracture or dislocation of a joint in the injured limb should be realigned or repositioned; first, by palpating distal pulses during the secondary survey to document a difference between the injured limb and the contralateral limb in a hemodynamically stable patient. A patient with decreased pulses at the wrist or ankle as compared to those in the contralateral uninjured limb or with an API of 0.9 in an injured limb should undergo imaging to document the presence of a possible arterial lesion. The choice of imaging study varies with local experience, but most data are available from arteriography, CT angiography or duplex Doppler ultrasound5. In those patients, where it is less clear that a definite arterial lesion is present, ancillary studies including API may be helpful. An API of < 0.9 is indicative of vascular injury and warrants further investigation. The negative predictive values of an API 0.9 are a remarkable 99% making it a good screening test. Alternatively, ABI is the ankle systolic pressure divided by the highest arm systolic pressure with the same connotation as ABI6. The only drawback of API is the need for a linear Doppler ultrasound, but in the absence thereof, suspicion and above all vigilance of these patients are very important. The sum of clinical data that are not indicated as soft signs such as pain in the limb on exertion (claudication), the difference in pulses and blood pressure between the two arms, and the severity of the injury (fracture) should indicate the need for extension studies to rule out or confirm arterial damage.
In a damage control situation, a temporary shunt can be quickly placed. Common brachial artery ligation carries a 55% amputation rate compared to 25% below the deep one. Small lacerations are repaired with interrupted 6-0 polypropylene. Injuries that are more extensive are repaired with venous patch, end-to-end anastomosis or vein graft interposition7. As modern technology has become a mainstay in trauma centers, computed tomography angiography (CTA) is increasingly used in place of conventional angiography diagnostics in patients with penetrating extremity injuries. Compared to CT, conventional angiography is associated with higher levels of ionizing radiation, higher incidence of hematoma, and infection, as well as risks of iatrogenic vascular injury. A 10-year retrospective review of 64-detector CT scanners was reported in 446 patients. In 131 patients (29.4%) with penetrating trauma, it demonstrated major vascular injury on CTA of those who underwent subsequent repair surgery. None of the patients without vascular injury on CTA underwent subsequent vascular intervention. We conclude that extremity CTA is an accurate tool for surgical triage in patients with penetrating vascular trauma8. Particle-based computational methods are adapted to simulate injury and bleeding in the human body. To ensure anatomical fidelity, a three-dimensional model of a specific part of the human body is reconstructed from a dense sequence of CT scans of an animated patient. A geometry of the lesion is then generated by simulating the mechanics of a ballistic projectile passing through the anatomical model with the material point method. From the injured vascular segments, we identified the resulting geometry. Smoothed particle hydrodynamics is used to simulate bleeding, based on input boundary conditions obtained from a network model that is based on virtual representations of injury and treatment9. Growing technology will allow us to recreate the projectile trajectory in the future and better define those patients with vascular damage. It is worth remembering that vessels are not static depending on the flexion of the limb, at some moments the artery may be linear and at others present a capricious figure like an S. Furthermore, if we take into account that the bone structure plays a transcendental role in changing the projectile course in one or several trajectories, it is difficult to predict the trajectory accurately.
From September 1, 2004, to August 31, 2006, all vascular injuries treated at the Iraq Level III Air Force Theatre Hospital 332nd facility were prospectively recorded. Patterns of injury, mechanism of vascular injury, site and type of vessel injury, and the presence of no vascular damage were documented. The focus of the work was on extremity management experience (134 patients - 70%) with complex soft-tissue injuries. Regarding forty upper extremity injuries (4 axillary, 25 brachial, and 11 radial or ulnar), greater saphenous vein interposition was the best option. Most vascular injuries were due to explosive devices. Overall mortality and complication rates were low, 95% early limb recovery. These injuries present a unique challenge related to complexity. Venous reconstruction, combined with a strict wound management strategy, results in successful limb salvage with remarkably low infection, amputation, and mortality rates10. Some dislocations with vascular injury with certain arm, shoulder, and hand disability score have positive and significant correlation with severely injured limb score and prolonged ischemia time (> 6 h); therefore, we assume that ischemia time is more relevant than the other elements of the severely injured limb score. The use of a limb injury severity score of 7 or more points as an indication for primary amputation is not justified, as our patients with a limb injury severity score ≥ 7 achieved satisfactory functional outcomes at long-term follow-up. Hence, we recommend vascular reconstruction with any limb injury severity score as long as residual function appears reasonable. Early intervention and decreased ischemia time may increase the chances of limb salvage11. Experts in combat-wound vascular trauma report good outcomes in the upper extremity vascular trauma despite the fact that many of them work in field hospitals that present less than ideal conditions. The salvage attempt is critical because of the implications related to quality of life. Dedication, time, and care seem to be key factors, in spite of high injury scores, as long as function is viable.
Conclusions
Lesions of the humeral artery may remain unnoticed regarding the circulation of the arm and shoulder as well as the deep brachial artery, which may make diagnosis difficult, as it may seem to be a healthy limb.
Hard signs of vascular trauma require immediate examination in case of soft signs or soft extension studies of vascular lesions. However, in case of a high suspicion without any signs in its initial assessment, a second re-evaluation is recommended, especially in extensive tissue injuries such as bone fracture or onset of vascular component data such as pain on mobility (claudication) or paraesthesia.











 nueva página del texto (beta)
nueva página del texto (beta)