Introduction
Diabetic mastopathy (DM) is a rare, benign fibroinflammatory breast disease. Pathology studies have shown lymphocytic ductitis and lobulitis with varying degrees of fibrosis, vasculitis, epithelioid fibroblasts, and lymphoid nodule formation. Furthermore, named lymphocytic mastopathy, fibrotic mastopathy or sclerosing lymphocytic lobulitis, and DM have been associated with uncontrolled type 1 diabetes (T1DM) in premenopausal women2, but cases with type 2 diabetes and male patient have been described too3. DM was initially described by Soler and Khardori1 and represents a collection of clinical, radiological and histological features found in breast lumps. In this review we describe two cases of DM that mimics breast cancer by clinical examination and radiological assessment.
Case report
Case 1
37-year-old woman, with a long history of T1DM, has been diagnosed with multiple diabetes-related complications such as chronic kidney disease, retinopathy, and hypertension. The chief complaint included a 2-week history of an enlarging left breast lump. Clinical examination showed a 5-cm left breast nodule and no enlarged nodes where detected during axillary examination. Mastography and mammary ultrasound showed BI-RADS 4c (Fig. 1). Ultrasound-guided biopsy was performed, and pathology study showed DM without evidence of invasive carcinoma (Fig. 2).

Figure 1 Breast ultrasound. A: irregular mass with angular margin and parallel orientation, show posterior shadowing. Color Doppler showing no vascular flow within the mass; B: percutaneous breast biopsy and the tip of the needle lie in the center of the lesion.
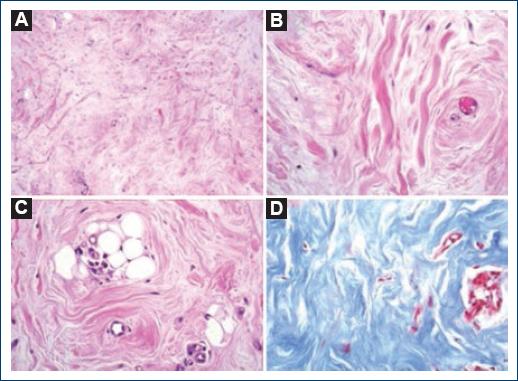
Figure 2 The characteristics lesions of diabetic mastopathy. A: hyalinized fibrous collagen bundles (H and E, ×100); B: approach of figure A, thick bundles of collagen (H and E, ×400); C: adipose tissue atrophy and lymphoplasmacytic inflammation foci are evident in some fields (green arrow) (H and E, ×400); D: the collagen bundles and fibrotic tissue are more evident with Masson’s straining (Masson ×400).
Case 2
We report a 42-year-old woman with a long history of T1D with diabetic neuropathy. She came to our center because of an enlarging left breast mass. Clinical examination showed a left breast mass with nipple retraction. Mastography and ultrasound revealed a left breast BI-RADS-4c lesion (Figs. 3 and 4). Ultrasound-guided biopsy was performed, and after pathology study, DM was diagnosed.
Literature review
Soler and Khardori1, in 1984, were the first to describe the association between diabetes mellitus and benign fibroinflammatory breast disease. Based on different reports, the association between diabetes mellitus and DM has been reaffirmed and associated with the presence of microvascular complications (nephropathy, retinopathy, or neuropathy)6. It usually appears as a palpable and hard breast lump, clinically indistinguishable from breast cancer.
Mammography is usually the first study for evaluation in women with breast palpable nodule. The most common mastographic findings in DM are: (1) a breast nodule with high density and poorly defined margins, (2) focal asymmetry in density, without associated calcifications, speculated borders or changes of adjacent skin, and (3) normal axillar nodules7-9.
Breast ultrasound is the standard of care imaging study for DM diagnosis. The most common findings include irregular hypoechoic breast lesion with indefinite, angulated or microlobulated margins, with acoustic shadow10. There is no ultrasound signal suggesting vascularity in Doppler mode. Normally, these findings do not rule out malignancy and a BI-RADS 4a is the most usual classification determined in these lesions. The ultrasound-guided core biopsy is better than the excisional biopsy. Surgical biopsy is not indicated for the diagnosis, only in cases of high uncertainty of malignancy; it is not recommended as initial therapy because a high percentage of recurrence is observed.
In 1987, Byrd and Hartmann described the histopathology features of DM as the combination of connective tissue overgrowth, and perivascular lymphocytic infiltrate as a characteristic of this lesion4.
The pathogenesis of DM remains unknown, several mechanisms have been suggested; Seidman et al. proposed that administration of insulin could produce chronic inflammation; Tomaszewski et al. described DM as an increased collagen production and decreased degradation related to the hyperglycemic state; and Ely et al. hypothesized that bilateral presentation and the multiple recurrences would indicate a systemic cause rather than a local event.
In a follow-up of 19 patients (including 17 women and 2 men) with DM, Ely et al.5 described the histopathologic findings of DM characterized by the presence of lymphocytic ductitis or lobulitis, and keloidal fibrosis and perivasculitis. They described the presence of ductitis as universal, but lobulitis was present only in female DM cases (as the men breast lacks lobules). Six of 19 cases recurred at follow-up (three ipsilateral, two contralateral, and one bilateral). In 2013, Akahori et al.3 described a case of DM in a man with 20 years of diagnosis of type 2 diabetes treated with hypoglycemic agents. He had diabetic retinopathy and neuropathy, but no nephropathy.
MD can present with synchronic or metachronic lesions (multifocal). Surveillance is the only treatment for these patients, but any new breast mass needs a complete evaluation to rule out malignancy, which may represent multiple biopsies overtime10. The breast cancer prevalence in these women is similar than general population, but the diagnosis of malignancy is more difficult.











 nueva página del texto (beta)
nueva página del texto (beta)




