Introduction
In 1958, Charles Rob defined thoracic outlet syndrome (TOS) as "a set of symptoms that may exist due to compression on the brachial plexus and on subclavian vessels in the region of the thoracic outlet." TOS affects approximately 8% of the general population1. Patients often report pain, which can lead to significant disability. Weakness is another common symptom. Vascular TOS presents with edema and cyanosis of the upper limbs with decreased pulses2. Although arterial complications arising from the compression of the thoracic outlet are present in < 5% of the operations carried out by TOS, these complications have great medical importance due to their serious prognostic implications. In 1905, Murphy performed the first successful resection of the cervical rib in a patient with TOS and subclavian artery aneurysm using the supraclavicular approach3. Arterial TOS is always associated with bone abnormalities, in the cervical rib, a fibromuscular band, or a fracture. TOS generally affects young patients, with an average age of 36 and predominance in males. This disease can be devastating by threatening the upper limbs. Delay in diagnosis is common, which is frustrating for the patient and can lead to permanent damage4.
Case study
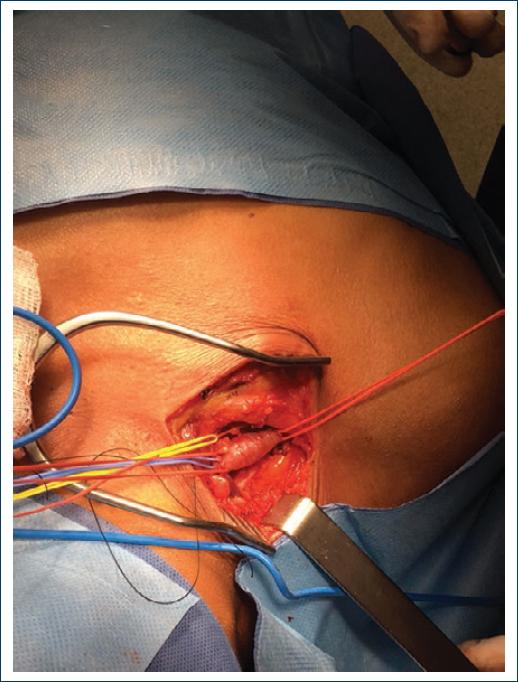
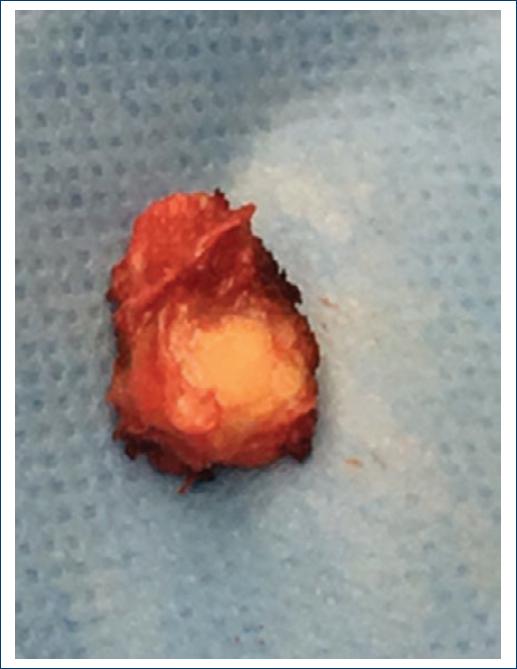
A 40-year-old female patient admitted to the High Specialty Regional Hospital (Hospital Regional de Alta Especialidad) of the Yucatan Peninsula, with a 2-week history of pain, paresthesia, muscle weakness, and coldness in the right upper limb. Physical examination revealed paleness and coldness of the hand, with decreased muscle strength and absence of pulses. Doppler arterial ultrasound was performed, in which brachial artery thrombosis was documented. Hence, the patient underwent emergency surgery, that is, brachial arterial exploration, where an arteriotomy was performed to obtain an organized thrombus. Embolectomy was performed with a Fogarty catheter, extracting organized thrombi, subsequently obtaining flows. When the operation was completed, weak pulses were obtained in the brachial, radial, and ulnar artery. On the 1st post-operative day, it was decided to perform arteriography of the supra-aortic trunks and thoracic limbs due to high suspicions of TOS, due to the patient's age and as risk factors for arterial thromboembolism were not detected. The arteriography shows dilatation in the subclavian artery posterior to the compression site and severe stenosis, as well as cervical rib (Figs. 1 and 2). Resection of the first cervical rib was performed by the right supraclavicular approach, with post-stenotic dilatation of the right subclavian artery in the transoperative period (Figs. 3 and 4). The patient was discharged on the 2nd post-operative day without complications.

Figure 2 Severe stenosis of the right subclavian artery with abduction of the arm at 45° (lower arrow) and cervical rib (upper arrow) is observed.
Discussion
Patients with arterial symptoms constitute only a small fraction of < 5% of the entire population of patients with neurovascular compression in the thoracic outlet region. TOS is frequently caused by congenital or acquired abnormalities. Regarding patients with arterial TOS, 88% have bone abnormalities and congenital bone abnormalities are the most frequent cause. The cervical rib is present in most patients in arterial TOS complications5. Long-term compression in the subclavian artery leads to various arterial lesions including stenosis with or without mural thrombus, post-stenotic dilatation, and post-stenotic aneurysms. These chronic changes carry risks of complications such as embolism of the arm or hand, leading to acute ischemia of the limb or digital gangrene5,6. A simple X-ray of the neck and thorax with a view of the cervical or thoracic spine often shows bone anomalies that can help in the TOS diagnosis. However, the negative predictive value of a simple X-ray is debatable, and in almost all cases, a definitive diagnostic image is required to establish or rule out a TOS diagnosis. Arteriography or venography has traditionally been considered the gold standard diagnostic test for vascular TOS, as it provides information on the exact location and nature of the vascular compression. However, due to being invasive and the lack of visualization of the surrounding structures, it is only reserved for guidance in interventional procedures. Computed tomography (CT) with contrast and magnetic resonance imaging (MRI) are widely available, reliable, and reproducible modalities used to establish the diagnosis of vascular TOS. CT scans provide information about the vasculature and relationship with adjacent bone structures; MRI is more effective in the representation of accessory muscles, muscle hypertrophy, and fibrous bands. The American College of Radiology recommends CT scans and MRI to establish the diagnosis of TOS5. Surgical treatment is required for patients with symptoms and evidence of arterial complications such as intimal damage, mural thrombus, embolization, post-stenotic dilatation, or aneurysm formation. The appropriate surgical strategy is guided by three main principles: decompression, arterial resection, and distal revascularization. There are two main surgical approaches for TOS decompression: transaxillary and supraclavicular. The main advantage of the transaxillary approach is that it provides a complete visualization of the first rib for its resection and presents a minimal risk of injury to the neurovascular structures. This approach is widely used for neurogenic TOS, as it is not suitable for vascular reconstruction. The supraclavicular approach is preferable for arterial TOS because it allows for the resection of a cervical rib and first rib, fibromuscular structures, and vascular reconstruction3.
Conclusion
Arterial TOS is a rare and relatively uncommon cause of upper limb ischemia. Its complications threaten the life and viability of the limb. Arterial TOS can present itself with symptoms of ischemia related to stress or emboli, typically in the context of an aneurysm with partial thrombosis. Bone abnormalities, such as a cervical rib, a prominent transverse process in the seventh cervical vertebra (C7), or a prominent bony callus after a clavicular lesion, are typically associated with this compressive syndrome. Embolization may require urgent treatment with thrombolysis or surgical embolectomy. The supraclavicular approach is usually preferred when arterial reconstruction is indicated for better access to the subclavian artery.











 nova página do texto(beta)
nova página do texto(beta)