Background
Atopic dermatitis (AD) affects a large portion of the population, particularly children under 5 years.1,2,3,4 It usually precedes the development of other allergic diseases such as food allergy, asthma, rhinitis, and/or conjunctivitis, therefore, it is considered as an important risk factor for these diseases.5,6
AD has a great impact on the quality of life of patients. The frequency of physiological or psychiatric problems in patients with moderate to severe dermatitis is higher than those in patients with diabetes mellitus.7 The economic cost of skin hydration, physician visits, and drug treatment has increased in the last years.8,9,10 Therefore, the evaluation and management of AD should be comprehensive and must include all the stakeholders: patients, relatives, and health care systems.
Although there are excellent guidelines offering an appropriate approach to manage this disease,11,12 transparent evidence-based guidelines following the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) approach13 are needed.14 Since each patient must receive personalized treatment, the recommendations presented here may not be appropriate for all patients, nevertheless, they offer a kickoff for disease management based on current scientific evidence.
Methods
Update objectives: to evaluate some commonly used interventions in dermatitis and new practical interventions.
Target population: patients with AD regardless their age, but it is focused on under-6 children because they are the population with the highest AD incidence.15
Implementation place: these recommendations are to be implanted on outpatient clinical management.
Target users: general practitioners, family doctors, dermatologists, allergists, and pediatricians.
Clinical aspects covered: evaluation of topical and systemic dermatitis management interventions. Prevention and acute management. Outpatient management.
Clinical aspects not covered: management in hospitalization and/or emergencies.
Definitions
According to the recommendation of the WAO (World Allergy Organization),16 it is better to use the term “eczema” than “dermatitis”, while confirmatory immunological studies are done; also, WAO recommends limiting the use of the term “atopic eczema” when a mediation IgE is demonstrated in the pathophysiology of the disease, and “non-atopic eczema” when it is discarded. In many countries, the term “dermatitis” is used as an equivalent to “eczema”, so, in this guideline and in the bibliographic search we use both.17,18,19
Staff conformation
Since the first revision of the Dermatitis-SLAAI (Sociedad Latinoamericana de Asma, Alergia e Inmunología) Guidelines in 2015,20 new evidence has accumulated about some interventions in AD.
For this update, a stakeholder group with allergists, dermatologists, pediatricians, epidemiologists, and immunologists, developed the review protocol and made an open invitation to SLAAI members to participate.21 Subsequently, those members who correctly performed the protocol tasks and writing the guide were included in the staff.
Protocol to the guide update
This guideline update was focused on new information about some practical interventions in dermatitis. Characteristics of the epidemiology, classification, and pathogenesis of the disease are discussed in detail in the 2015 Consensus.20 ARIA (Allergic Rhinitis and its Impact on Asthma) report protocol was used as a model22 and the update protocol was based on PRISMA recommendations (see supplementary material).23
By using the Delphi process,24 the panel staff reached an agreement on the topics that required an update and on new topics that deserved to be included, and performed a systematic review of the literature to identify and summarize the evidence for each one of them (see supplementary material). Each topic is presented as a clinical question, and the answer to each question includes a conclusion with the strength of the recommendation according to the GRADE system.14 The AGREE Reporting Checklist was used to evaluate the completeness and transparency of the guideline recommendations.
For external validation and to assess the clarity of the concepts and their applicability, the manuscript was presented to allergists, dermatologists, general physicians from academic and external scientific institutions, and groups of patients. External recommendations were then discussed again by the staff and included in the manuscript.
Questions and outcomes of interest
The guideline panel deemed the following outcomes to be important to patients: cutaneous symptoms like pruritus and eczema, quality of life, work/school performance, and serious adverse effects. In general, these variables were considered critical for the decisions to be made, regarding the answer to each question. The questions chosen were:
How should we classify atopic dermatitis in clinical practice?
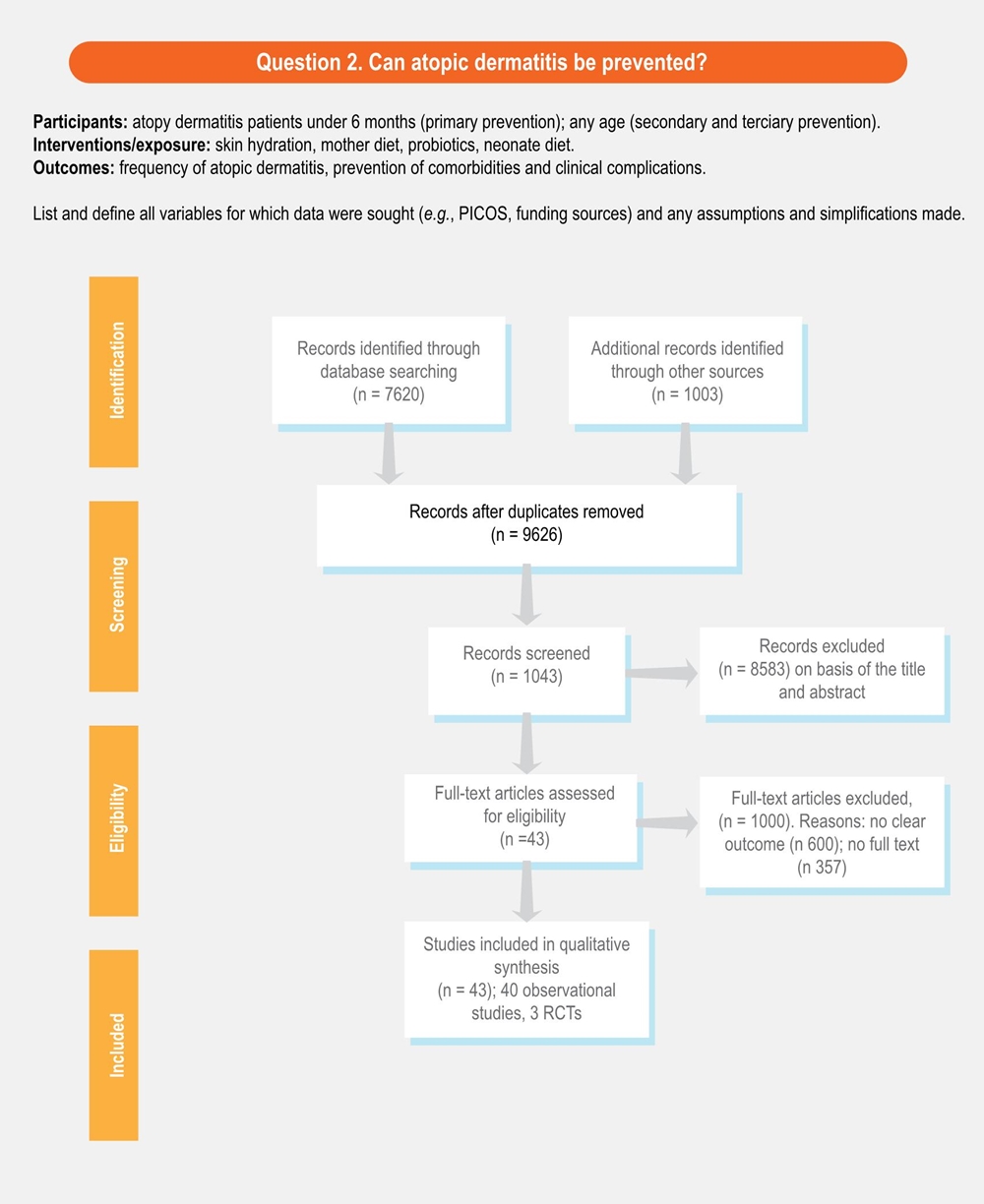
Can atopic dermatitis be prevented?
Can we predict the duration of atopic dermatitis?
Does the cutaneous microbiota influence the control of atopic dermatitis?
Is the use of probiotics in atopic dermatitis useful?
Can restriction diet help as a treatment of atopic dermatitis?
Are non-pharmacological interventions useful in the treatment of dermatitis?
Do antihistamines help in the treatment of atopic dermatitis?
When and which immunomodulator should be used in atopic dermatitis?
What new pharmacological treatments are available for atopic dermatitis?
Bibliographic search and evidence review
We systematically searched articles from December 2000 to December 2018 from the Medline and LILACs electronic databases. Titles and abstracts, and subsequently full-text articles were screened in duplicate to assess eligibility. Articles in English, Spanish and Portuguese were reviewed.
Studies were included if they provided empirical data related to the panel staff questions (clinical trials, cohort studies, case-control studies). We excluded narrative reviews and case reports. We shared the bibliography collected among the team members; in case any staff member considered it was necessary to include an additional reference, this was discussed.
Clinical recommendations
We prepared evidence summaries for each question according to the GRADE approach.14,25 The certainty of the evidence was categorized into four levels: strong, moderate, low, and very low. Specific criteria for evidence classification are presented in figure 1.

Figure 1 Classification of the evidence. The recommendation was classified based on the grade of evidence and the interpretation of the committee. We considered patient preferences and cost effectivity.
For each question, we summarized all information including a concise description of desirable and undesirable health effects.26,27 The answer to each question was reviewed by the panel staff, who provided feedback by means of electronic communications. The answers were modified accordingly when it was necessary. Recommendations and their strength were decided by consensus.
Results
Limitations from the systematic review
The protocol for this systematic review was not previously registered in any database, which limits the reproducibility of the results. However, since in the guide we considered the patients’ opinions and the reality of the clinical practice in different countries, these variables, that influenced the recommendation, could not be reproduced only with the bibliographic search. In supplementary material 1 and 2, an approach of the search carried out for each question is presented. However, a standardized evaluation to avoid the risk of bias was not used.
Limitations from articles
There is a considerable heterogeneity among the studies, patients’ characteristics, evaluation of clinical control, and the safety of each intervention. Additionally, many studies indicated the response to treatment without clarifying the doses of the drug, the treatment length, measurement of treatment efficacy, the speed of the effect, and/or follow-up period. We provide the rationale for the recommendations and the consideration of some factors that influenced the recommendations.
1. How should we classify atopic dermatitis in clinical practice?
Recommendation. Severity classification is available to all physicians and it is useful to define interventions (high, 1a). Atopy-based classification (yes/no) seems to be useful for the prognostic of duration in children (moderate 1a).
Explanation. AD can be classified in several ways.20 Some classification proposals according to endotypes have been done,28,29 but their utility in clinical practice is unclear. The presence or not of atopy seems to be associated with the patient’s clinical characteristics and the probability of remission or not, thus, the classification of allergic or non-allergic eczema according to the skin prick test result or IgE serum can be useful in the clinical practice.
The classification of the severity is established with different scoring scales, such as: Severity Scoring Atopic Dermatitis (SCORAD) and Eczema Area and Severity Index. These scores are defined according to three parameters: extension of the disease and type of injury; some scales also include pruritus and sleep disturbance as perceived by the patient. We recommend the use of these or any other validated clinical scale since they allow physicians to classify the severity of the patient, the degree of affectation and allow the decision making regarding the most appropriate medical intervention.
2. Can atopic dermatitis be prevented?
Recommendation. Primary prevention: early skin hydration (first six months of life) seems to decrease the risk of dermatitis (strong 1b). Secondary prevention: skin hydration and inflammation control improve the clinical control of dermatitis, and some evidence suggests that these interventions could modify the severity of eczema (moderate 2b).
Explanation. Primary prevention: the increase of IgA levels with breast milk30 and the use of milk hydrolyzed formulas in high-risk infants reduced the cumulative prevalence of eczema.31 Although these results are supported by some studies, other research studies do not reproduce these results, so their implementation cannot be widely recommended.
Two multicenter studies demonstrated that the daily use of emollients, with application on all the skin, significantly reduced the cumulative incidence of AD in children at 12 and 36 months, which corresponded to a relative risk reduction, between 30% and 50%.32,33 It is necessary to evaluate the cost-effectiveness of this intervention.34
Secondary prevention. The daily use of emollients in patients with mild-moderate disease prevents and delays exacerbations, as well as decreases the use of topical steroids and prolongs eczema-free time.35,36,37 Although there is controversial evidence,38 it seems that vitamin D supplementation during the winter season improves AD related to winter.39,40
3. Can we predict the duration of atopic dermatitis?
Recommendation. Maternal eczema, onset after two years old, severe onset, are associated with long duration of dermatitis periods (over 14 years old) (moderate 2a). Nevertheless, no single factor is enough to predict the duration of the disease (strong 2b). The creation of a prognostic model evaluating the magnitude of each individual factor could be useful.41
Explanation. Most childhood dermatitis remitted before puberty, nevertheless, from 1% to 25% of patients persist with symptoms even in adulthood.20,41 Findings from 14 systematic reviews published before 2016 observed that persistent atopic dermatitis is associated with more severe disease at the time of diagnosis, onset after the age of two years and being a female.42 A systematic review including 45 studies was considered and found that a later onset increased persistence.43 Some genetic factors have been associated with persistent dermatitis, but these factors are not easy to use in clinical practice.44
Some studies suggest that children with atopy from house dust mites or foods before their first year should be considered at risk of AD persistence;45,46 although it is not clear if atopy is a consequence of greater severity, it could be used as a duration predictor.
4. Does the cutaneous microbiota influence the control of atopic dermatitis?
Recommendation. The cutaneous microbiota influences the control of AD (strong 1b), however, heterogeneity in intervention strategies on bacterial overgrowth (topic or systemic antibiotics), makes comparative evaluations and the power of evidence difficult to extend and evaluate (moderate 2a).
Explanation. Microbial colonization of skin begins, more effectively, after birth and depends, in part, on the type of delivery; cesarean delivery children have a cutaneous microbiota profile that resembles maternal skin, while cutaneous microbiota of vaginal delivery children has a more diversified profile, similar to the maternal vaginal scenario.47 During puberty, new changes occur in skin microbiota.48 There are several mechanisms by which changes in microbial skin diversity (dysbiosis) affect the development of atopic dermatitis; the production, by these dysbiosis bacteria, of several enzymes, such as: proteases (which induce corneocyte desquamation); lipases (which break down lipids of skin barrier); ceramidases (which break down the ceramides present in the barrier structure).49,50 This bacterial overgrowth, with subsequent biofilm formation and mainly related to the pathogenic strains of Staphylococcus aureus (methicillin-resistant Staphylococcus aureus), would be directly related to changes in the cutaneous barrier.51,52,53
Cutaneous microbiota is associated with dermatitis severity, but it is less clear its effect in the pathogenesis; antibiotic interventions are also expected to be able to improve the dermatitis symptom scores. However, a systematic review,54 in 21 studies with different interventions (oral antibiotics, antibacterial soaps, topical steroids/antibiotics/antifungal, baths with antibacterial solutions) did not show differences statistically significant.
5. Is the use of probiotics in atopic dermatitis useful?
Recommendation. There is a potential effect of the use of probiotics in the prevention of atopic dermatitis (moderate 3a); however, methodological limitations, a wide variety of strains and the dosage schemes, lead to discordant and contradictory results and their routine use is not recommended.
Explanation. Probiotics could help dermatitis through restoration in the function of the intestinal barrier, degrading food antigens, regulating the Th1 and Th2 response, regulating the composition and activity of the intestinal microbiota and stimulating the production of IgA.55 The WAO in a systematic review indicates that is likely net benefit from using probiotics the primary prevention of eczema.56 The use of Lactobacillus rhamnosus, Lactobacillus salivarius, Bifidobacterium lactis and others, in several small studies has shown relief of symptoms, which results in an improvement of SCORAD,57,58 being more effective during the first two years of life.
Although probiotics are safe and are used as a reasonable option of dermatitis preventive treatment in under-6-month children or high-risk pregnant women, their impact on active treatment appears to be reduced.59,60
However, in order to apply this recommendation, solving several practical questions that currently do not have an answer is necessary, for instance: Does the type of microbiota affect the impact of probiotics? What dosage? For how long? What strains should be used?.61 The lack of control of these variables in the different clinical trials limits the ability to implement this intervention.
6. Can restriction diet help as a treatment of atopic dermatitis?
Recommendation. In patients with an objective demonstration of exacerbation of dermatitis by a food, dietary restriction is indicated (moderate 3a). Atopy to food allergens is not enough to initiate a dietary restriction (strong 1a).
Explanation. Frequently, patients associate food consumption with the onset or worsening of their disease.62,63,64 The sensitization to foods in children with AD is very prevalent, being the majority of cases asymptomatic (without clinical relevance).65,66 The subgroup of moderate to severe AD have a higher risk of sensitization to food allergens and this is translated into a high risk of true food allergy.65,67,68 The clinical history, along with an allergology evaluation, can help to identify suspect foods, but it is necessary to verify with restriction diets for 3 to 4 weeks or controlled oral challenges.
The avoidance of foods previously tolerated or never ingested due to a positive skin test without clinical confirmation of hypersensitivity reactions, is associated with an increased risk of severe reactions, after their reintroduction into the regular diet.69,70,71,72 Therefore, the avoidance of food should only occur in cases of AD with clinical impact confirmation.73 In cases in which negative results in oral challenges or food restrictions did not improve AD, foods must be reintroduced.74
7. Are non-pharmacological interventions useful in the treatment of dermatitis?
Recommendation. The hydration of the skin is a non-pharmacological intervention with adequate evidence for the treatment and prevention of eczema exacerbation in dermatitis (moderate 2a). Although the evidence is weak and the magnitude of this measure is not known, we recommend the use of hypochlorite, loose and preferably cotton-made clothing in patients with AD (low 3a-4). We discourage the use of products with perfume or clothing that may increase sweating (low 3b).
Explanation. The treatment of AD is a challenge because it is a chronic disease, which occurs with periods of outbreak and remission. The therapeutic approach of dermatitis includes two aspects: the management of active eczema and the prevention of new exacerbations.
The emollient preparation should be chosen according to the skin dryness degree, the areas of application, and the patient’s acceptance.75,76 Using tight or rough clothes, personal care products with alcohol or perfume, exposing oneself to heat or carrying out activities inducing heavy sweating, among others, should be avoided as far as possible.77,78 Some recommendations with low evidence but cost-effective are usually done: baths should be tempered and brief, no more than five minutes. Skin hygiene and cleaning should be smooth, scabs should be removed; avoid perfumes. Using hypochlorite during bath could reduce colonization of some bacteria.79,80,81 Using comfortable, loose and preferably cotton-made clothing seems to prevent skin exacerbation.
8. Do antihistamines help in the treatment of atopic dermatitis?
Recommendation. Some studies support the use of second-generation antihistamines to decrease pruritus in dermatitis (low 4). However, due to the lack of high-level evidence, we cannot make a recommendation in favor of or against the use of H1-antihistamines in the treatment of dermatitis-associated pruritus.
Explanation. Pruritus is usually the most distressing feature of AD.82 Histamine is one of the multiple mediators of itching in dermatitis. However, it is not clear if it has a key role.83 There are no large, randomized, double-blind, and placebo-controlled studies with precise endpoints on the efficacy of antihistamines in AD. Antihistamines (especially first generation) have been used in dermatitis to reduce scratching, however, these drugs, in most of the studies, are not more effective than placebo.84,85,86,87 Nevertheless, some studies, especially those with second-generation antihistamines, suggest a possible positive effect in pruritus and repair of the cutaneous tissue;88,89,90,91 these effects increased with a topical steroid.92
First generation sedating antihistamines have been used in dermatitis to promote sleep84,85 but sedating antihistamines reduce the rapid-eye-movement (REM)-sleep, affecting the quality of sleep and directly interfering with work efficiency in adults and learning skills in children.93
9. When and what immunomodulator should be used in atopic dermatitis?
Recommendation. The decision to start systemic therapy should be based on the severity of the symptoms, but also on the impact on the patient’s quality of life, as well as on the consideration of the risks and benefits of systemic therapies for each individual patient (strong 1b). Many randomized controlled trials (RCTs) with immunomodulator interventions for dermatitis have not used standardized efficacy outcome measures, which makes interpretation of results difficult. In addition, comparative studies between the existent systemic treatments in dermatitis are rare.
Explanation. Most patients with AD respond satisfactorily to conventional topical management. However, 10% to 50% of patients may not achieve adequate disease control with these regimens and require systemic immunomodulatory/immunosuppressive therapies. Before considering a systemic therapy, it should be determined whether the failure of conventional therapies is due to the severity of the disease, comorbidities, or lack of adherence to the treatment. The action mechanism of each one of these interventions is explained in detail in the previous dermatitis-SLAAI guideline.20 In table 1, we present some details of each one of some of these therapies. It is important to note that most of these therapies are not approved by the FDA or EMA for dermatitis.
Table 1 Immunomodulator interventions
|
Systemic drug intervention |
Doses |
Do not use in…* |
Efficacy- effectivity** |
GRADE recommendations |
Dupilumab |
|
Serious eosinophilic conditions |
50%-70% |
Strong 1a |
Phototherapy |
40-120 sessions |
Do not use in pregnancy and children under 6-year-old |
40%-70% |
Moderate 2b |
Cyclosporine A |
2.5-5 mg/kg/day |
Renal failure, pregnancy |
30%-90% after 4 months |
Moderate 2b |
Methotrexate |
5-25 mg once a week (the use of MTX must be complemented with folic acid) |
Pregnancy, breastfeeding, liver dysfunction |
30%- 80% |
Moderate 2b |
Azathioprine |
1-2.5 mg/kg/day |
Pregnancy, mielosupression |
30%- 70% |
Moderate 2b |
Mycophenolate (oral) |
1-3 g/day |
Pregnancy, breastfeeding, |
20%-80% |
Weak 3b |
Omalizumab |
150 mg/4 weeks to 450/2 weeks |
Patients without IgE demonstration |
30%- 50% |
Weak 4, expert opinion based in case reports |
The selection of the systemic drug for dermatitis, more than a selection step by step, should be based in individual safety profile, availability and access. The use of immunosuppressants can facilitate the onset of respiratory or skin infections.
*These medications may have other contraindications, the most frequently described are presented in the table.
**Different scales have been used to evaluated efficacy-effectivity, we present the effect size in percent as standard unit. The safety and efficacy of dupilumab in children have not been established.
Dupilumab. It was approved in early 2017 for moderate-to-severe adult dermatitis.94,95 Dupilumab is a fully human monoclonal antibody that blocks the alpha subunit of the receptor interleukin (IL) 4 and IL-13. The blockade by dupilumab of these key drivers of type 2 helper T-cell (Th2)-mediated inflammation help in the treatment of AD. Patients treated with dupilumab had marked and rapid improvement in all the evaluated measures of AD disease activity; Dupilumab also reduces the need for systemic steroids (NCT01259323, NCT01385657, NCT01639040, and NCT01548404.).95,96,97,98
Phototherapy or photochemotherapy. It is one of the alternatives with the highest number of articles and some RCT supporting its effectiveness. However, the need of attendance to the center of execution between 2 to 4 times per week limits its access and use.99,100,101,102 Different forms of light therapy are available, and have proved efficacy: narrowband (NB)-UVB, broadband (BB)-UVB, UVA, UVA1, cold-light UVA1, UVA and UVB (UVAB), full-spectrum light (including UVA, infrared and visible light), psoralen plus UVA, and other forms of phototherapy. One of the principal limitations for phototherapy is the requirement to attend several times per week for its application. However, some new home-applied modalities are being developed.103
Systemic corticosteroids (SCSs). They are not recommended as a control intervention for the treatment of dermatitis. Their use should be limited to very short terms (up to 1 week) during acute flares in need of immediate relief and as a transition to steroid-sparing therapies because of their adverse-effect potential.104,105,106
Cyclosporine A (CSA). It is an approved drug for severe dermatitis in some countries and numerous studies showed improvement of the skin symptoms by at least 50% after six to eight weeks of therapy.107,108,109,110,111 Once the drug is stopped the symptoms reappear quickly, eventually reaching pretreatment values approximately after 8 weeks from the end of treatment.109,110,111 CSA has been shown to be effective and relatively safe in adults who received up to 1 year of continuous treatment,112,113,114,115,116 but some of these studies had high dropout rates.116 The staff recommended choosing the regimen on an individual basis; it could be reasonable to start with a dose of 2.5 mg/kg/day,114,117 unless a rapid improvement is considered necessary, when a dose of up to 5 mg/kg/day may be used.116,118,119
Methotrexate (MTX). Patients receiving MTX should be monitored for hepatic and pulmonary toxicity, and myelosuppression.120 Different studies have shown good efficacy for MTX.121,122 MTX has some advantages and disadvantages compared to CSA but it seems to have a similar effectivity;122,123,124 The onset of control seems to be faster with ciclosporin, but relapse after stopping the medication seems to be less frequent with MTX
Azathioprine (AZA). Efficacy of AZA (2.5 mg/kg/day) was tested in some RCT, especially in adults,107,125 with efficacy (30 to 70%) in the severity of eczema and skin pruritus. In an RCT comparing MTX (10-22.5 mg/week) with AZA (1.5-2.5 mg/kg/day), at week 12, no statistically significant differences were found in the clinical impact (MTX SCORAD of 42% (standard deviation [SD], 18%) vs AZA 39% [SD, 25%]),126 but abnormalities in blood count (mostly lymphocytopenia) were statistically and significantly more frequent in the AZA group (p = 0.002).
Mycophenolate (MMF). Some case reports or uncontrolled clinical trial data from adults indicate that MMF could be effective in dermatitis.127,128,129,130,131 In an observer-blinded randomized controlled trial in 55 patients, a lower dose CSA (3 mg/kg/d) was found to be equally effective to oral MMF (EC-MPS, 1440 mg/d) as a maintenance therapy for severe dermatitis during a maintenance phase of 30 weeks and a 12-week follow-up period.112 The MMF group had a slower onset of action with 29% of the MMF patients requiring short courses of systemic glucocorticoids compared to none in the CSA group.132
Therapies like omalizumab, interferon gamma, and others, have been used in atopic dermatitis and may be useful for some patients but there are only case reports and case series supporting this recommendation. Some clinical trials are being conducted with omalizumab, but no results have been reported (Clinicaltrials.gov NCT01678092, NCT01179529).
10. What new pharmacological treatments are available for dermatitis?
Recommendation. Dupilumab is recommended in severe AD (strong 1a). Crisaborole is recommended in mild and moderate AD, but a safety-efficacy comparison to other topical interventions is needed (strong 1a).
From the dermatitis-SLAAI guideline in 2015 to these days, two molecules were released to the market and approved by the Food and Drugs Administration (FDA): crisaborole, a topical phosphodiesterase 4 (PDE4) inhibitor, became available in late 2016 in the United States and Europe for mild-to-moderate dermatitis. It can be used topically. Clinical trials have demonstrated its efficacy in treating patients with mild to moderate atopic dermatitis (children > 2 years) (AD-301: NCT02118766; AD-302: NCT02118792).133,134 The potency of crisaborole seems to be equivalent to the one of a moderate-potency steroid , but the frequency of adverse effects seems to be lower; as of now, there is no evidence of atrophy, telangiectasia, or hypopigmentation, resulting from its use.135 However, there are few equivalence or superiority studies comparing this molecule to topical steroids, therefore, at the moment, crisaborole is recommended at the same level as the use of steroids or calcineurin inhibitors.
Dupilumab has been shown to be effective in adult patients refractory to topical steroids and also in patients who did not respond to CSA.136 Among the adverse effects that have been described are the increase of eosinophils in the blood (without apparent clinical impact, but it requires more studies) and a high frequency of conjunctivitis.137 The high cost of dupilumab and the lack of studies in children are the main limitations for its use.
Conclusions
For this update, we covered a small number of topics. However, these were systematically reviewed. Many interventions have been proven in patients with dermatitis, but due to the lack of studies with an adequate design, most of these interventions have a weak or moderate recommendation. Further studies are needed in order to predict the duration and severity of the disease, as well as which interventions are the most appropriate for each patient.
Funding
This article was supported by the Group of Clinical and Experimental Allergy, from the Clinic IPS Universitaria of the University of Antioquia (Medellín, Colombia).











 nueva página del texto (beta)
nueva página del texto (beta)