Background
Atopic dermatitis (AD) is a chronic skin condition that is caused by genetic, inflammatory and environmental factors.1,2 It is a common disease and it is the leading cause of pediatric dermatology consultations, and it affects 5-20% of the pediatric population worldwide.3 In Colombia, according to the ISAAC study (International Study of Asthma and Allergies in Childhood), Barranquilla is amongst the Latin American cities with the highest prevalence of eczema in childhood; reaching up to 25-30% of prevalence in children between 6-14 years of age. The city of Bogotá stands out with a prevalence in childhood of 19% in the pediatric population and 13% in the general population.4,5
The natural history of the disease involves eczematous skin lesions that produce intense pruritus which affect sleep and general function, which impairs the patient’s ability for social interaction and focus during school hours.6,7 This causes a negative impact on their quality of life and it has been linked to psychiatric diseases like anxiety, depression, and attention deficit disorder.8 Pediatric AD has also been associated with progression to other allergic diseases like food allergies, asthma, and allergic rhinitis.9
The treatment of AD depends on the severity of the disease. The mainstay of the treatment involves an adequate hydration of the skin.10,11 Topical steroids are generally used as the first line medical therapy, as are topical calcineurin inhibitors and allergen-specific immunotherapy. Second and third line therapies include systemic immunosuppressors like cyclosporine, azathioprine, methotrexate, mycophenolate, and systemic steroids. Antihistamine agents have a role in suppressing pruritus, and phototherapy has been proven to be effective in the treatment of AD.12,13 Despite a wide range of therapeutic options, a percentage of patients with severe AD remain refractory to any of these treatments; a fact that has promoted the search for newer therapies like omalizumab or IFN-γ.
Omalizumab is an IgG-type monoclonal antibody with affinity for an epitope in the IgE’s epsilon heavy chain (Cε3). When bound to IgE, it avoids the linkage of the immunoglobulin to the high-affinity FcεRI receptor, which is located in mastocytes and basophils. Omalizumab causes a reduction in the serum IgE, as well as down regulation of high-affinity FcεRI receptors, which impairs mastocyte and basophil degranulation and, thus, it prevents early and late phases of allergic type-1 hypersensitivity reactions.14
Due to its profile of effectiveness and safety in the treatment of other IgE-mediated diseases like asthma and allergic rhinitis,15 omalizumab is a promising option for severe refractory cases of AD. Although evidence of its use in adult AD has proven its usefulness, evidence of omalizumab in pediatric AD is scarce. This study aims to describe the use of omalizumab as a concomitant therapy in pediatric populations with severe AD, and to serve as a starting point for further research of this monoclonal antibody as therapy for this disease.
Method
We retrospectively analyzed the records of patients with refractory AD from the pediatric outpatient allergy service of the “Fundación Santa Fe de Bogotá” who were treated with omalizumab from 2010 to 2015. The inclusion criteria were: patients who met the Hanifin and Rafka diagnostic criteria, as indicated in the Latin American Guideline for Atopic Dermatitis;16 the patients must had been 18 or younger at the beginning of the treatment; diagnosis of severe and recalcitrant AD, defined as persistent AD refractory to treatment with multiple drug combinations such as oral corticosteroids, azathioprine, methotrexate, cyclosporine, or phototherapy; and treatment with omalizumab for at least 6 months. Those patients who had been treated with omalizumab for less than 6 months were excluded. A chart review of all patients who met the inclusion criteria was done. The data was retrieved by using a data collection tool that included the following variables that were documented during regular office visits: age, sex, duration of the treatment with omalizumab, previous therapies before their treatment with omalizumab, concomitant therapies, side effects, and scales used to assess the level of compromise of their quality of life and the severity of the disease, among others. Analogue scales were used to assess the level of compromise of their quality of life before initiating treatment (from 0 to 10, 0 being “no symptoms” and 10 being “disabling disease”). The improvement time after initiating treatment with omalizumab was measured by patient self-reported improvement of symptoms during office visits. At maximum treatment time, an allergy specialist utilized SCORAD and CDLQI on most patients in order to assess the severity of the disease and the level of compromise of their quality of life, respectively. The descriptive statistics were made with STATA 12 software. A Spearman correlation test was carried out in order to calculate the correlation coefficient between baseline serum IgE levels and SCORAD and CDLQI scores at maximum treatment time.
SCORAD and Children´s Dermatology Life Quality Index (CDLQI)
The SCORAD tool has been validated to assess the severity of the disease in AD and its results are classified as mild (0-24 points), moderate (score from 25-49 points), or severe (50-103 points). The CDLQI is also a validated tool that is used to assess the quality of life in pediatric patients with AD, and scores range from 0 (no effect on the patient’s quality of life) to 30 (great effect on the patient’s quality of life).17 A validated Spanish version of the CDLQI was used.18
Results
19 pediatric patients with severe AD were included; ten females and nine males, with a mean age of 14.7 ± 3.3 years and a median age of 15 years. The baseline characteristics and treatment outcomes are summarized in table 1. Sixteen patients had a history of allergic rhinitis, 9 patients had a history of asthma, and 7 patients had a history of food allergies. Twelve patients had a family history of allergic diseases. An 82.4% of patients had baseline serum IgE levels over 2000 IU/mL (range: 251 IU/mL-46000 IU/mL). Eighteen patients had previous allergy tests that tested positive to one or multiple allergens, either by skin prick tests or by positive serum-specific IgE (ImmunoCAP). Fifty eight percent of these were only sensitive to aeroallergens, with dust mites and grass being the most common. Forty-two percent of patients were sensitive to both aeroallergens and food allergens; eggs were the most common of the latter.
Table 1 Patient baseline characteristics and severity of the disease and quality of life at the end of the therapy
Patient |
Age (years) |
Gender |
Personal history of atopy |
Previous therapies |
Allergen sensitivity |
Baseline IgE (UI/mL) |
Treatment duration (months) |
SCORAD* |
CDLQI* |
1 |
10 |
F |
Asthma, allergic rhinitis |
sIgE:Aeroallergens, 2; food allergens, 2 |
6667 |
36 |
8.1 |
9 |
|
2 |
8 |
F |
Asthma, allergic rhinitis |
SP: Aeroallergens, 5; Food allerg: 0 |
2796 |
13 |
— |
— |
|
3 |
9 |
M |
Asthma, allergic rhinitis, food allergies |
SP: Aeroallergens, 3; Food allerg: 0 |
N/A |
33 |
6.9 |
7 |
|
4 |
13 |
M |
Asthma, allergic rhinitis |
SP: Aeroallergens, 1; food allergens, 0 |
2500 |
34 |
25.8 |
4 |
|
5 |
13 |
F |
Allergic rhinitis |
SP: Aeroallergens, 1; food allergens, 0 |
24146 |
21 |
3 |
7 |
|
6 |
9 |
M |
Allergic rhinitis, food allergies |
sIgE: Aeroallergens, 5; food allergens, 4 |
11358 |
23 |
61.08 |
17 |
|
7 |
17 |
F |
Allergic rhinitis |
SP: Aeroallergens, 4; food allergens, 1 |
2500 |
8 |
— |
— |
|
8 |
13 |
F |
Allergic rhinitis, food allergies |
sIgE and SP: Aeroallergens, 2; food allergens, 3 |
9987 |
6 |
— |
— |
|
9 |
17 |
M |
Asthma, food allergies |
sIgE: Aeroallergens, 2; food allergens, 3 |
499 |
53 |
22.2 |
2 |
|
10 |
9 |
F |
None |
sIgE: Aeroallergens, 2; food allergens, 0 |
1344 |
8 |
45.8 |
22 |
|
11 |
11 |
F |
Allergic rhinitis |
sIgE: Aeroallergens, 3; food allergens, 0 |
11260 |
22 |
44.85 |
3 |
|
12 |
16 |
M |
Asthma, allergic rhinitis |
sIgE: Aeroallergens, 1; food allergens, 0 |
N/A |
6 |
— |
— |
|
13 |
17 |
M |
None |
sIgE: Aeroallergens, 3; food allergens, 0 |
15667 |
29 |
— |
— |
|
14 |
15 |
M |
Asthma, allergic rhinitis |
Mo, TCort, TAb, Clr, SCort, Ttac, TMP, Cyc, Az, ImT, Anti-H, Phot, Diet |
sIgE and SP: Aeroallergens, 2; food allergens, 3 |
2500 |
17 |
26.2 |
17 |
15 |
19 |
F |
Allergic rhinitis, food allergies |
Mo, TCort, TAb, Clr, Cphx, StSCort, Ttac, Az, ImT, Anti-H, Diet |
sIgE: Aeroallergens, 4; food allergens, 5 |
2500 |
7 |
23 |
7 |
16 |
18 |
F |
Allergic rhinitis, food allergies |
sIgE: Aeroallergens, 3; food allergens, 0 |
2473 |
8 |
34.4 |
14 |
|
17 |
10 |
M |
Asthma, allergic rhinitis |
SP: Aeroallergens, 0; food allergens, 0 |
251.8 |
14 |
78.3 |
26 |
|
18 |
16 |
M |
Asthma, allergic rhinitis |
SP: Aeroallergens, 4; food allergens, 0 |
2947 |
20 |
— |
— |
|
19 |
14 |
F |
Allergic rhinitis |
SP: Aeroallergens, 3; food allergens, 6 |
46000 |
15 |
8 |
3 |
*Taken at maximum treatment time.
Mo = moisturizing agent, TCort = topical steroids, Tab = topical antibiotics, Clr = clarithromycin, Cphx = cephalexin, TMP = trimethoprim-sulfa, SCort = systemic steroids, StSCort = short-term systemic steroids, Ttac = topic tacrolimus, Mtx = methotrexate, Az = azathioprine, ImT= immunotherapy, Cyc = cyclosporine, Anti-H = antihistamines, Ket = ketoconazole, Acyc = acyclovir, Humid = humid therapy, Diet = diet restriction therapy, Phot = phototherapy, SP = skin prick test, sIgE = specific IgE, SCORAD = Scoring Atopic Dermatitis, CDLQI = Children’s Dermatologic Life Quality Index.
As a tertiary referral center, all patients were referred by dermatologists due to refractory AD. The patients arrived with the diagnosis and with a long standing pharmacological history for the control of the disease. As such, all patients had received treatment with a moisturizing agent, a daily topical steroid and calcineurin inhibitor (topical tacrolimus). Seventeen patients had received a prolonged course of systemic steroids at some point, ranging from 0.5 months to 38 months of use. Twelve patients had received some kind of immunosuppressive medication like azathioprine, methotrexate, or cyclosporine before starting omalizumab. Four patients were treated with dietary restrictions, thirteen received treatment with an anti-histamine drug, and one received phototherapy. None of the patients achieved complete control of AD symptoms.
At the time of the first office visit, eight patients were not enrolled in school or had been absent for extended periods of time. Six patients reported depression due to their skin lesions and were referred to a psychiatry consultation service. In the first office visit, all patients and their families had been interviewed about the impact of the disease on their quality of life by using a subjective scale from 0 to 10 (see Method). All patients reported a compromise of life quality of 8 or more points, with 25% rating the impact on their lives as 10/10.
The omalizumab dosing varied according to the patient’s weight and it ranged from 150 mg to 600 mg subcutaneously every 2 to 4 weeks. The dose was calculated according to the dosing recommendation for omalizumab in the treatment of severe asthma, based upon total IgE levels and the patient’s weight. Fifty percent of the patients reported improvement within five months or less from the beginning of treatment with omalizumab, and all patients perceived an improvement in symptoms within 9 months or less. The mean duration of the treatment was 20.1 months (95 % CI = 14.1-26.1). The mean time to notice subjective improvement of symptoms (as stated by patients) was 3,6 months. A total of 8 patients had disease flares while on omalizumab. Two out of 4 patients who discontinued treatment with omalizumab suffered regressions in symptoms and skin lesions.
All patients received treatment with clarithromycin as an anti-inflammatory agent in their first office visit in order to control symptoms and taper the use of systemic steroids while awaiting response to omalizumab. The macrolide treatment was extended for long periods of time ranging from 1-12 months (mean: 3 months). The use of clarithromycin lowered the use of systemic corticosteroids, but it was insufficient for improving the severity of the disease.
Regarding the severity of the disease after the treatment, SCORAD and CDLQI scores were obtained at maximum treatment time in 14 patients. The mean SCORAD score was 28.1 (95 % CI = 15.1-41.2), ranging from 3 to 78.3. Half of these patients had mild disease, 35.7% had moderate disease, and the remaining 14.3% had severe disease. After treatment, the quality of life, as assessed by CDLQI, was found to be unaffected or slightly affected (CDLQI score < 7) in 35.7% of patients, moderate to largely affected (score 7-18) in 50% of patients, and severely affected (score > 18) in 14.3% of patients. The six remaining patients in whom SCORAD or CDLQI was not obtained, reported an improvement in the severity of the disease above 8/10 by using a numerical analogue scale from 0-10 (0 being “no improvement at all” and 10 being “the biggest improvement” since diagnosis). No correlation was found between the baseline serum IgE levels and the SCORAD index score (rho −0.4, p = 0.1008) or CDLQI score (rho −0.38, p = 0.19) at maximum treatment time.
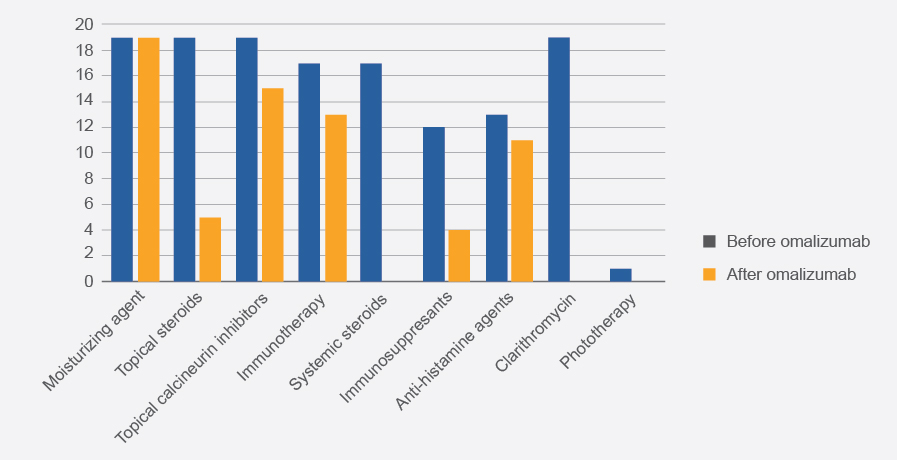
In the last scheduled visit, all patients were on moisturizing agents, 15 patients were using topical tacrolimus in specific skin regions; 5 patients were using daily topical steroids, 6 patients were using it occasionally, 4 did not require topical steroids, and 4 did not specify dosing. None of the patients was using systemic steroids. Four patients were taking systemic immunosuppressant agents other than steroids for symptom control; 3 of them were taking azathioprine and 1 was taking cyclosporine. In addition, 13 patients were using immunotherapy only for dust mites and 2 patients were using it for grasses and dust mites. The different frequencies between treatment regimes before and after omalizumab are shown in figure 1. No serious adverse events were reported with the use of omalizumab.
Discussion
This series of cases represents, to our knowledge, the largest series of cases of pediatric patients with severe AD treated with omalizumab as an adjuvant therapy. The cases reported in this paper represent an extreme end of the AD severity spectrum. None of the patients had achieved an adequate symptom control with first, second, or third line therapies for AD. Six patients (31.6%) had associated depression and one of them had a previous suicide attempt prior to treatment. Eight patients (42.1%) had dropped out of school due to the disability that AD had caused them. These numbers highlight the devastating consequences that severe, refractory AD can have on a child’s life, and they set the clinical profile where omalizumab may have the largest effect.
Regarding the outcomes of the disease after the omalizumab therapy, 85.7% of patients had an improvement in their quality of life and the severity of the disease within 9 months after initiating treatment with omalizumab as an adjuvant therapy. These results agree with a recent literature review on the use of omalizumab for adult AD in which 74.1% of patients (129 out of 174) showed improvement, varying between a small response to a complete response.19 On the other hand, 14.7% of our patients did not improve with treatment, which agrees with previous findings by Wang et al.17 Their study analyzed 13 studies for a total of 83 patients, 70% of which presented some degree of improvement, while 27.2% of the patients showed satisfying results and 30.1% showed irrelevant clinical changes or even deterioration.20
Even though evidence has been gathered mainly on adult populations with severe AD, findings suggest that omalizumab may also represent an effective therapy in pediatric patients with the disease.21,22 Lacombe et al.22 reported a series of cases of 7 children between 6-19 years of age with severe AD who were treated with omalizumab with similar baseline characteristics to those of our patients. After 12 months of treatment, an improvement in SCORAD index scores was documented (p < 0.005), for a mean score of 30. These results are similar to our findings, where the mean SCORAD score after treatment was 28.1, suggesting that omalizumab can offer multiple benefits by decreasing the severity of the disease in recalcitrant cases, as well as diminishing exposure to side effects from steroids and immunosuppressive drugs. In addition, Lyengar et al. carried out a randomized clinical trial that included 8 patients between 4-22 years of age with severe AD. They found a SCORAD improvement after therapy with omalizumab was initiated. However, no significant differences were found when compared to the control group. These findings must be viewed with caution since they can be influenced by a small sample size and the big age differences between the placebo group and the omalizumab group.23
In our experience, the use of clarithromycin as an adjuvant therapy in severe AD proved to reduce the need for systemic steroids and it was useful for controlling acute flares of the disease. Evidence suggests that macrolides can negatively regulate chronic inflammation by reducing reactive oxygen species, inhibiting neutrophil activation and blocking the production of nuclear transcription factors. Their prolonged use as an immune response modulator has been described in several chronic inflammatory diseases.24 More importantly, immune response modulation and anti-inflammatory properties of macrolides have been reported in animal studies simulating AD,25,26 which could explain the short-term improvement in our patients when using clarithromycin. Due to its prompt effect, it might be a good therapeutic option in cases where systemic steroid tapering is needed while awaiting response to omalizumab. None of the patients in our series suffered from infection by resistant bacteria after receiving long courses of clarithromycin. We suggest further randomized control trials in order to assess the effectiveness of long courses of macrolides as an adjuvant therapy for treating AD.
Our study evaluated the use of omalizumab as an adjuvant therapy along with multiple treatments including immunotherapy, systemic immune suppressors, clarithromycin, and topical therapy. However, the improvement of the disease cannot be attributed only to omalizumab since concomitant therapies could also contribute to clinical improvement in unknown proportions.
The response to omalizumab varied within our patients, which raises the question of predictive factors of response to this medication. In our study, there was no correlation between basal serum IgE levels and end of treatment severity or quality of life score; a result that may be biased by the size of our small sample. It is worthy of note that a good response was observed in the patient with the highest value of IgE (patient 19, IgE: 46 000 IU/mL). This contrasts with the findings of previous studies with a larger sample size where serum IgE levels below 700 IU/mL were associated with excellent clinical response.20 Hyper IgE syndrome must also be considered in patients with IgE levels above 10 000 IU/mL. This was excluding in all of our patients by the absence of clinical and phenotypic characteristics of the disease, such as severe and recurrent skin and airway infections in early life.27
Omalizumab improved the quality of life in all the reported cases. All patients reported a severe compromise (more than 8/10 on a numeric analogue scale) before the treatment, but only 14.6% of patients stated an extremely big compromise of the quality of life after the treatment with omalizumab according to the CDLQI. In addition, all 8 patients who had dropped out of school before the treatment were able to re-enter school after receiving omalizumab. This shows the positive effect on functionality that omalizumab may have in severe cases of pediatric AD. Our findings concur with a similar study made by Ramírez del Pozo et al. They studied patients between 12-52 years of age with severe AD who were treated with omalizumab as an adjuvant therapy. A significant decrease in the Dermatological Life Quality Index (DLQI, a questionnaire for adults similar to the CDLQI) was noticed.28
The limitations of our study include the small sample and the absence of a control group because of the nature of the study. Furthermore, the obtained results have methodological limitations since different scales were used to evaluate both the severity of the disease and the compromise of the quality of life before and after the treatment with omalizumab. The numerical analogue scale that was used to assess the severity and quality of life before initiating treatment gives way to subjectivity and it may be difficult to assess in pediatric populations, and it cannot be compared unequivocally to SCORAD and CDLQI scores after treatment. It does, however, allow to understand the subjective appraisal of the severity of the disease and the quality of life from the patient’s perspective. In perspective, a limitation of the use of omalizumab in Latin America is its limiting cost and availability, which limits the applicability of our study. However, our results highlight the positive impact of such treatment on a disease with a high burden among the population. Although we did not aim to evaluate the cost-effectiveness of omalizumab, our results favor the widespread use of this medication for treating severe pediatric AD.
Conclusions
To our knowledge, this study represents one of the largest series of pediatric cases of severe AD that were treated with omalizumab. Our findings are in line with reported literature on the use of omalizumab for AD, and they shed promising light on its use in pediatric populations with severe AD independent of serum IgE levels; an area that has yet to be carefully studied. Its possible benefits as an adjuvant therapy with conventional treatment in pediatric patients include the improvement of the quality of life, the decrease of the severity of the disease, and it acts as a steroid and immunosuppressive-sparing medication, in addition to its benign safety profile. Up to the moment, there is not enough evidence to determine the factors that predict the response to omalizumab in pediatric AD. Further research is needed to evaluate the use of omalizumab as monotherapy. Moreover, the use of adjuvant clarithromycin as an immune-modulating agent along with conventional treatment in severe AD appears to be safe for controlling disease flares











 nueva página del texto (beta)
nueva página del texto (beta)