Background
Atopic dermatitis (AD) or allergic eczema affects a large percentage of the population around the world, specifically children under 5 years old (5% to 25%).1,2,3 Some European and American tests suggest that this disease usually begins before the age of two, but can occur at any time of life, although in most patients it disappears before puberty, it may extend into adulthood.4,5 There are no significant differences between genders in the first years of life, but it seems to be more common in women (3 of 5 patients) than in men (2 of 5) after the 6 years.6,7 This disease has been recognized as an important factor for the development of other allergic diseases such as food allergy, rhinitis and asthma.8,9,10 Dermatitis has a wide clinical spectrum. The acute features involve intensely pruritic erythematous papules with excoriation and serious exudate and the chronic condition is characterized by lichenification, papules and excoriations.11,12,13 The burden of those clinical symptoms has significant physical and social impact. Parents of children with AD have reported associated feelings of guilt, exhaustion, frustration, resentment and helplessness over their child’s condition.14 Kemp et al., reported that family stress associated with caring of children with moderate to severe AD was significantly greater than the ones with diabetes mellitus.15
The financial burden along with the physical and social impact of AD is also considerable. With cost of physician visits, treatment and work loss over 500 million dollars per year in only The United States and The United Kingdom.14,16
There is a growing concern over a noted increase in the prevalence of AD in many epidemiologic tests, nevertheless there is a high variation in the frequencies, that it may depend on many reasons such as populations characteristics and the diagnostic criteria selected in each test.17 Some international approaches using the same diagnostic tool have shown significant regional differences. ISAAC is the most widespread international test which evaluates dermatitis epidemiology, which tested the prevalence of atopic childhood diseases in more than 1,000,000 children of age between 6 to 7 and 13 to 14 years old in almost 200 sites in more than fifty countries around the world. ISSAC determined the presence of dermatitis using a questionnaire completed by the participants based with the Williams diagnostic criteria of dermatitis.18 In ISAAC’s phases ONE and THREE several sites from tropical countries were included. According to that test, the prevalence of dermatitis in tropical countries, especially in those from Latin America, was higher in comparison with other regions with a mode of 15%. That percentage among those populations using the same survey suggests that some genetic and environmental factors have an important effect on the development of dermatitis. However, considering that the surveys were completed by participants, it is possible that there was a misidentification of the disease and a tilt made from the patient are possible.
In the present article we compared the prevalence of dermatitis reported by ISAAC in tropical countries and some tests using other methodological approach. In addition, we evaluate the impact of infectious skin problems on the differential diagnosis of atopic dermatitis.
Challenges in the diagnosis of atopic dermatitis
According to the recommendation of the World Allergy Organization (WAO), the general term for a local skin inflammation should be dermatitis. and propose the term eczema to replace the term previously used as syndrome eczema/dermatitis.19 They also recommend limiting the use of the term atopic ezcema, when a mediation immunoglobulin E (IgE) is demonstrated in the pathology of the disease, and non-atopic ezcema when it is discarded. While confirmatory immunological tests are done, the recommend only using the term ezcema. however in many countries the term dermatitis is used as equivalent to ezcema, therefore in this article both are used as interchangeable terms.
The diagnosis of atopic dermatitis is based on a set of clinical symptoms and features, but there is not a worldwide accepted diagnostic test.20,21 The presence of pruritus is an essential symptom in patients with dermatitis who usually also have eczematous or lichenified injuries with periods of exacerbation and control. The distribution of eczema can change with time. According to some European tests children under the age of two years face and the extensor region were involved and are more common in toddlers than in the elderly, where folds features become more relevant. However, that distribution is not exclusive to each age group. The Hanifin and Rafka diagnostic criteria proposed over 30 years ago.22 summarized the four main characteristics to be considered when auscultating a patient with suspected AD. All diagnostics criteria that appeared subsequently -including Williams criteria- are based on them.23
Pruritus
Distribution and typical morphology
Chronic or recurrent symptoms
Personal or family history of asthma, rhinitis and/or dermatitis.
For diagnosis, is essential the presence of pruritus and at least two of the other criteria. Other symptoms such as xerosis, follicular hyperkeratosis, total IgE, conjunctivitis, tendency to skin infections, facial erythema, Dennie Morgan double fold, and sensitization to food, contact dermatitis and seborrheic dermatitis could support the diagnosis and are considered “minor criteria”.
As we can notice, these symptoms are not pathognomonic of dermatitis and could be present in other skin diseases. In tropical countries especially in under development areas, other causes of pruritus and lichenified injuries are common (scabies, papular urticarial, seborrheic dermatitis, miliaria, infection induced rashes, etc.):
Miliaria (also called “sweat rash” or “heat rash”) is a skin disease common for its small and itchy rashes.24 It is a common illness in hot and humid conditions, sucha s in the tropics and during the summer season in subtropical regions. Although it affects people of all ages, it is especially common in children and infants due to their underdeveloped sweat glands.
Papular urticarial is caused by a hypersensivity reaction to some insect’s protein like flea, tick and mosquito.
Scabies is common skin diseases especially in children under the age of 10 years (9%) caused by infection with the mite Sarcoptes scabiei.25,26 The characteristic symptoms of scabies infection include intense itching and superficial damage.
Some prospective studies have shown that in some tropical areas like South Indian, Brazil and Turkey more than 30% of children under the age of 7 years old could be infected with miliaria and the main differential diagnosis is dermatitis.27,28,29 In this studies, more than 15 000 children under the age of 14 years old were evaluated and 4 000 of them had a skin disorder. The results of three tests agree that in most of the 50% of dermatoses the etiology was infectious skin diseases like scabiosis, nevertheless between 50 to 80% of those cases were initially diagnosed as dermatitis by the physician. Dermatitis was the second dermatoses most frequent found in those three tests but with only a 9% of prevalence (6.5% to 12%). Because of the similarity between injuries caused by these diseases and dermatitis, sometimes they may represent a diagnostic challenge for the physician and require additional tests to make the correct diagnosis. It is also common that some of these diseases are present simultaneously hindering the proper diagnosis and initiation of appropriate treatment. In Nigeria, a study in which were included 1066 children under the age of 12 years old observed that about 20% of those children with dermatoses have two or more skin disease.30 Dermatitis was virtually absent (less than the 1%) but in the 60% of those patients they have another skin disorder being infection diseases like pityriasis or scabies.
ISSAC results about dermatitis.
As we mentioned before, ISAAC is a worldwide epidemiological test.31 The vision of ISAAC is to evaluate the prevalence of asthma and other allergic conditions among children living in different regions of the world. And to make comparisons within and between those countries. The study population was made up by school students in two age groups: 6 to 7 years old (parental completion of questionnaires), and 13 to 14 years old (self-completion of questionnaires). In both age groups, a questionnaire was used to assess symptoms of asthma, rhino-conjunctivitis, and allergic eczema.31,32 Although the questionnaire had questions about three most common allergic diseases an age range selection was performed focusing on asthma: the older age group has been chosen to reflect the period when mortality from asthma is more common. The younger age group has been chosen to give a reflection of early childhood years, when asthma is more prevalent, and hospital admission rates are higher. If we consider that dermatitis usually starts in the first two years of life and some cohort studies show a remission rate at 5 years of 80%, the selected age range generates a recall tilt.32
A sample size of 3,000 participants per age group was recommended in order to provide sufficiently accurate estimates of symptom severity, although smaller sample sizes (minimum of 1 000) were permitted for prevalence comparisons among participants sites.31
The core questionnaire was translated from English into the languages spoken by the populations that were tested. And those translations were validated prior to phase 2 and 3. The following questions from ISAAC survey were focused about dermatitis:
Have you (has your child) ever had an itchy rash which was coming and going for at least six months?
Have you (has your child) had this itchy rash at any time in the past 12 months?
Has this itchy rash at any time affected any of the following places: the folds of the elbows, behind the knees, in front of the ankles, under the buttocks, or around the neck, ears or eyes?
Only for 6 to 7 year-olds: At what age did this itchy rash first occur? (under 2 years of age, 2 to 4 years of age, 5 years old or more).
Has this itchy rash cleared completely at any time during the past 12 months?
In the past 12 months, how often, approximately, have you (has your child) been kept awake at night due to this itchy rash? (never in the past 12 months; less than 1 night per week; one or more nights per week).
Have you (has your child) ever had eczema?
In addition to those questions, two combinations of symptoms were evaluated4
Current symptoms (affirmative responses to questions 2 and 3).
Current symptoms of severe eczema (answered who have current symptoms of eczema as above and who have 1 or more nights per week sleep disturbance form rash).
The two age groups were analyzed separately. Symptom prevalence was calculated by dividing the number of positive responses to each individual question by the number of completed questionnaires. As we can see, 5 of the 7 questions are focused on pruritus, and the positive response by the survey would suggest that the child has or had dermatitis. However, except for the question about the distribution of lesions, none of these questions can differentiate if the itching was secondary to other common skin conditions, especially those described earlier in this review.
Until 1999, when the results of ISAAC phase 1 were published, little was known about the prevalence of atopic eczema outside Northern Europe.18 In ISAAC phase 1, data available for 256, 410 children between the ages of 6 and 7 years old in 90 sites and 458 623 teenagers between the ages of 13 and 14 years old in 153 sites worldwide showed a tremendous variability in the prevalence of symptoms of eczema. From less than 2% in Iran to over 16% in Sweden in children aged 6 to 7 years old. And from less than 1% in Albania to over 17% in Nigeria for those aged 13 to 14 years old.18
According to ISAAC phase 1 and phase 3 results, more than 1,000,000 children were included and it was observed that the prevalence of ezcema ever in tropical countries among children aged 6 to 7 years old, varied from 5% in Jodhpur, India to 44% in Quito, Ecuador. The presence of current eczema varied from 0.9% in Jodhpur to 22.5% in Quito. In children between 13 to 14 years old, the prevalence ranged from 0.2% in Tibet, China to 24.6% in Barranquilla, Colombia. All sites in tropical areas from Latin America and Asia showed a significantly higher risk of current symptoms. La Habana, Cuba and San Pedro Sula, Honduras were the sites with the highest risk of current symptoms of severe eczema in tropical region.
In the ISAAC relationships between different factors related to the prevalence of current symptoms of eczema and the severity in each country were evaluated, but only economical income was associated with dermatitis. For 6 to 7 year-olds, there was a significant negative correlation between national income per capita and mean country prevalence (excluding Cuba) of current symptoms of dermatitis (r = −0.564, 95% CI = −0.856 to −0.0003, p = 0.01), but not for severe dermatitis (r = −0.539, 95% CI = −0.846 to −0.036, p = 0.057). However, for 13 to 14 year-olds, both relationships were significant (r = −0.678, 95% CI = −0.886 to −0.275, p < 0.001 and r = −0.548, 95% CI = −0.870 to −0.209, p < 0.01, respectively). There were no significant relationships between dermatitis and many factors evaluated, among them: infant mortality rate; percentage of population with potable water; percentage of population with sewage disposal services; annual proportion of registered deaths under five years of age due to intestinal infectious disease.
To summarize, the ISAAC provides information about the prevalence of atopic dermatitis in the general population in various countries as to compare the results and identify possible risk factors. However, the age of the patients who underwent the questionnaire and kind of questions answered by self-reporting may lead to some recall tilt especially in tropical regions, where many other itchy skin diseases are highly prevalent.
Comparison of ISAAC and other epidemiological tests
For the same reason as you can see the cutaneous lesions, eczema is more readily confirmed by objective tests than either asthma or rhinitis. In theory, that could facilitate the identification of the skin disease by the patient. Nonetheless, in regions with a high prevalence of other similar skin diseases, the diagnosis could be a real clinical challenge even for specialized doctors (figure 1).
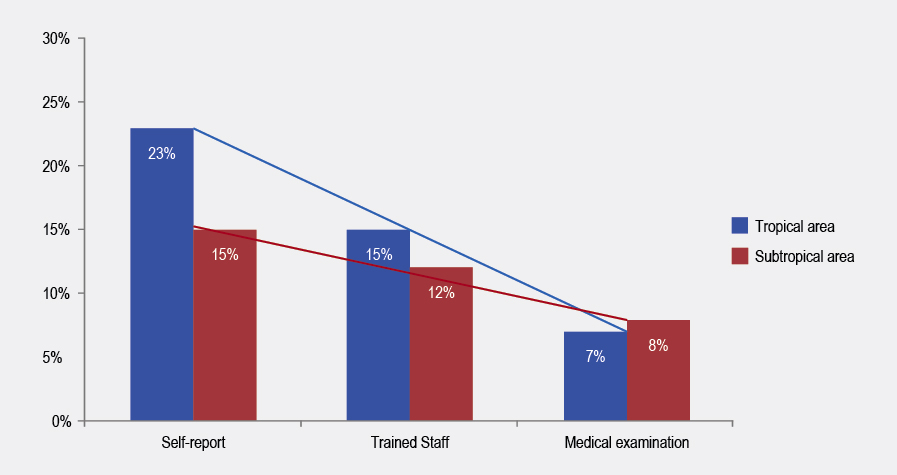
Figure 1 Prevalence of dermatitis in tropical and subtropical area. Evaluation of prevalence was conducted in three by three methodological ways: self-report, trained staff and medical examination
Some comparisons of parental report and physician examination of eczema in Britain, have suggested that eczema has a high prevalence in The United Kingdom,33,34 but the frequency observed was significantly different among studies (parental report: 27% vs physician report 14%). Even so, in some populations like Iran, the prevalence of ever eczema before 6 years of age evaluated by ISAAC questionnaires’ and medical examination is similar.35,36 The different results between auto-reported and medical report suggest that many factors in each region could affect the validity of knowledge of the disease, the sociocultural characteristics of the population, dermatitis definition used, the prevalence of other skin conditions and other factors.37
In tropical areas, one of the most highlight results of ISAAC phase 3 was the increasing prevalence of dermatitis compared with phase 1 and the high prevalence of dermatitis in Latin America countries. The higher frequency of current dermatitis among children 6 to 7 year-olds was observed in Barranquilla, Colombia with 24%. Those results are in stark contrast with data from similar study for Dennis et al., due in the same city (Barranquilla), at the same year, with the same ISSAC questionnaire and similar size population which parent-reported prevalence of less than 7% of current eczema.38 In that test, the prevalence of medical diagnostic of eczema was less than 2%. The frequency of severe eczema was similar between tests. Taking in consideration that the population, and the time of evaluation was the same, one possible explanation for the disparity between parent-reported results is that in the Dennis et al. test, parents received instructions for fill the questionnaire directly for a physician and in the ISAAC this explanation was given for no-physician personnel trained to conduct questionnaire. Dennis test also shows a difference between parent-reported prevalence and medical diagnosis, which is result to the physician’s ability to make differential diagnoses to various itchy skin conditions. In a second test Dennis et al., observed 10 years later, using the same methodology, that the prevalence of parent-reported eczema according ISSAC questionnaire, in Barranquilla was 11% and according medical diagnosis less than 7%.39 The increased prevalence agrees to the latest ISAAC reports, then again, the total prevalence differed between tests.
In another test from Cartagena, Colombia, which is located very near to Barranquilla, data from the Risk Factors for Asthma and Atopy in the Tropics (FRAAT) birth cohort with 326 children, shown that none of the children at age of three had developed atopic dermatitis. Given the ISAAC carried out the survey among families with children over 6years and FRAAT results were in population with less than 3 years, those results suggested that in some cities in Latin America, the onset of dermatitis is later in life (> 3 years) similar that found in some tropical countries located in the South-East Europe.6 Nonetheless in the follow-up test FRAAT at 5 years, it has shown no change in the prevalence of dermatitis (0%) (data provided by authors). Another possible explanation (again) could be the methodology of data recollection. In Barranquilla, ISAAC questionnaire was recollected by medical students who distributed the questionnaire and explained to parents. In the FRAAT cohort, eight patients present a skin disorder initially diagnosed as dermatitis, but an allergist revaluated the eight patients and in all cases the diagnosis of dermatitis was discharged: five were sick with popular urticaria, two with scabiosis and the last one with ictiosis vulgaris. It is possible that the high prevalence observed in Barranquilla could be due to other skin itchy disorders which the patient or their parents do not have the ability to differentiate. Nevertheless, as it is mentioned above, comparing rates of dermatitis is difficult because of the differences in tests designs, populations and case definitions.
Previous test suggest that the prevalence estimated by ISAAC project may overestimate the atopic eczema burden for countries. However, in some occasions parent-report could underestimate prevalence. According to ISAAC records in Buenos Aires, Argentina, the prevalence of ever eczema dermatitis was around 10%. Dei Cas et al.40 a test was composed of children in early infancy, this could partially explain the disparity with ISAAC results: Prospective tests suggest that there is a natural history of improvement of dermatitis by the onset of adolescence.41,42 However, if that was the case, it would question the reliability of the ISAAC questionnaire by a high rate of recall tilt.
The ISAAC set out to use a group of standardized questions relating to symptoms of atopic eczema with the goal of minimizing the cultural and social variations associated with the use of disease labels such as eczema.43,44 Although these questions have been effective in previous community validation tests most of them conducted in North Europe,45,46,47 more direct validation tests of those questions is required and it cannot be assumed that the same discriminatory functions applies in tropical regions such as Latin America, Asia and Africa where other itchy dermatoses, such as scabies and onchocerciasis, are common in childhood.
Gruchalla et al., in a test in Cuba, shown marked differences according ISAAC questionnaire and physicians diagnostic of dermatitis.48 A total of 398 children form five randomly selected elementary schools were included in the study. Their age range was between 5 and 13 years old (median eight years); parent or guardian of each child was interviewed by using an extended version of the ISAAC questionnaire. Additionally, each child was clinically examined by a physician. A Thorough inspection of the skin for signs of atopic dermatitis was done. For AD, the answers to the seven core questions yielded symptom percentages between 8% and 26%. Using the ISAAC definition for AD18 (affirmative answer to core questions 2 and 3), 9% of the children were diagnosed as suffering from AD, and 3.5% were suffering from severe atopic dermatitis. When physician evaluation was done, only 5 (< 2%) children showed clinical signs of atopic dermatitis. In that test, the authors observed a significant difference in dermatitis prevalence if they evaluated ISAAC questionnaires; considering the score that Yamada et al.49 (core questions on atopic eczema are graded a score for 0 to 2; positive for atopic eczema if global score is at least 3), 119% had AD. Despite the limitation of this data by the sample size, Cuba test shows a significant variation in dermatitis prevalence according the system used in questionnaires to defined dermatitis and in both systems dermatitis prevalence was overestimate according clinical examination.
Some other points to keep in mind when evaluating the results of the ISAAC test are:31,50
The definition of atopic eczema used in ISAAC overemphasizes flexural eczema and underestimates other patterns of presentation of dermatitis that may be more common in some populations like lichenification in Afro-American patients.
The generalizability of the ISAAC data is also limited by the fact that most of the data refer to children residing in urban settings, rendering it less able to examine factors that might only be revealed by examining rural/urban differences.
The nature of this school-based questionnaire test also means that children who do not attend school are excluded in the overall prevalence estimates.
Like all prevalence tests, it is unclear to which extent the global variation in atopic eczema prevalence reflects factors affecting disease chronicity (e.g. access to an effectiveness of treatment) as opposed to disease incidence.
Even though ISAAC is the largest and most comprehensive survey of atopic eczema symptoms conducted to date, there are still large gaps on the globe from which very little data is presented.
The low participation from some tropical regions as Central Africa and Asia is especially disappointing.
Several of the studies presented in this review highlight the need for medical examination to determine the real epidemiology of dermatitis, physician-diagnosed dermatitis usually contains a combination of history and clinical examination, sometimes supplemented with physiological and laboratory tests. However, the precise diagnostic measures and criteria used differ considerably from one test to another. While physicians agree that certain criteria are necessary to diagnose dermatitis, they disagree on the combinations of factors that are needed to do so. To our knowledge, only a few studies tried to arrive at a more accurate assessment of dermatitis prevalence by combining the ISAAC questionnaire with physician examination.
Conclusion
Atopic eczema is a common health problem for children and adolescents throughout the world. Symptoms of atopic eczema exhibit wide variations in prevalence both within and between countries inhabited by similar ethnic groups, suggesting that environmental factor may be critical in determining disease expression. Although several population tests of atopic eczema have been conducted, very little is known about the comparative prevalence of atopic eczema, especially outside Europe. The ISAAC permit comparisons to estimate the global burden of atopic eczema, to generate new hypotheses on disease causes that may only become apparent when prevalence data on a global scale are examined. And to test existing hypotheses regarding disease etiology on a wider scale. Nevertheless, ISAAC has some limitations and the results must be taken with precaution especially in tropical regions where other skin itchy disorders are frequent (table 1). Tests that include objective skin examinations are required to confirm the prevalence in said regions.
Table 1 Points to take in mind when atopic dermatitis prevalence according ISAAC results was evaluate
Although the ISAAC questionnaire had questions about the three most common allergic diseases, age range selection was performed focusing on asthma and this age range different form the most common age for dermatitis, increasing the risk of recall bias. |
ISSAC questions about atopic dermatitis are focus in itchy but other clinical characteristics like type of cutaneous lesions are under estimate. |
ISSAC questions have not enough specificity to differentiate atopic dermatitis from other skin diseases common in tropical areas. |
High variability in atopic dermatitis prevalence in the ISAAC this explanation was given for no-physician personal trained to conduct the questionnaire. |
Most of the ISAAC reports about atopic dermatitis prevalence were focus in the results of questionnaire without confirmatory test of atopy. |











 nueva página del texto (beta)
nueva página del texto (beta)



