Introduction
Mammary gland tumor is the third most common neoplasia in cats. It is mostly found in elderly felines ranging from 10 to 14 years old. Its incidence could be heightened by estrogen therapy, pseudocyesis, obesity, and a high-fat diet at a young age.1-5 This tumor can be affecting one or several glands in the mammary chain, ulcerated or not and can produce a discharge that could be mistaken as lactation. The diameter of the tumor is an important prognostic factor: cats with small tumors have a higher survival rate after their excision. Accurate metastasis detection can also aid to predict the best way to treat patients.6 The most frequent type of mammary tumor in cats is adenocarcinoma. It has a fast growth rate and can spread out to regional lymph nodes and other locations such as pleura, liver, and lungs.7-10 Primary pulmonary neoplasia patients may present different clinical features such as chronic cough, weight loss, exercise intolerance, tachypnea and/or dyspnea, that could be misinterpreted for heart diseases or other.11-13
Early metastases diagnosis can play a crucial role in improving patients' prognosis. Even though there are tissues and organs more likely to harbor metastases, it remains a challenge to locate them with ultrasonography or conventional radiology techniques. In contrast, the Nuclear Medicine approach allows a whole-body scan to locate and detect different types of tumor lesions. Thus, nuclear medicine is a promising tool for veterinary oncology.14-16 Here we evaluated a cat with mammary cancer carrying out scintigraphy with 99mTechnetium-thymine (99mTc-THY), a radio-nucleotide developed by our research group, and that has been successfully used for the detection of breast tumors in women.17-19
For an efficient labelling method of tumors, radiopharmaceuticals should highlight the investigated tissue/pathology. Since neoplasms have an intense mitotic activity, they readily incorporate the radioactive material, enabling tumor diagnosis and staging.20-22 We have shown that thymine, a nitrogen base of the DNA structure, is highly integrated by the neoplastic cells in tumors such as bronchogenic carcinoma, lymphoma, and breast carcinoma in women.17,18 In 2001, Gutfilen et al. found that 99mTc-THY is superior to 99mTc-MIBI on sensitivity (95.83% vs. 95.65%), specificity (94.73% vs. 71.42%), accuracy (97.61% vs. 86.48%) and positive predictive value (95.83% vs. 84.61%) on mammalian cancer detection.18
This study aimed to determine the contribution of 99mTc-THY scintigraphy in the evaluation and detection of mammary adenocarcinoma metastases in a cat.
Material and methods
Patient and clinical aspects
A shorthaired Brazilian nine-year-old domestic queen, weighing approximately 4 kg, presented with masses spread throughout all four mammary gland-pairs. Other clinical signs as anorexia, apathy, difficult breathing, and progressive weight loss were present. Urinalysis, blood exams and conventional radiographic examination results were normal. Two months later, the patient underwent 99mTc-THY scintigraphy for further metastatic investigation. Few days after performing the scintigraphy, the patient died. We proceeded the investigation with necropsy after the owner's written consent. Unfortunately, the ultrasound examination was not performed at the time the patient came to our hospital.
Sedation and scintigraphy
An anesthetic protocol, including ketamin 10% (15 mg/kg) combined with xylazine 2% (2 mg/kg), was administered intramuscularly prior to the scintigraphy. In order to perform the scintigraphy procedure, 0.9 mCi (0.2 mL) of 99mTc-THY were injected into the cephalic vein. One hour after the radionuclide injection, the patient was placed in dorsal decubitus for image acquisition. Ventral and dorsal planar images of whole-body were acquired in a General Electric Millennium gamma-camera (General Electric Healthcare, Chicago, IL, USA), with a low energy collimator.
Results and discussion
Two months before the scintigraphy procedure, thoracic radiography was performed (ventrodorsal and latero-lateral planes), and no metastatic processes were found. Dorso-ventral and ventrodorsal 99mTc-THY scintigraphy showed increased focal uptake in the liver and lungs, and unexpectedly a very high uptake of radionucleotide was observed in the right kidney. Further, wide-spread nodular alterations were found across the lungs, liver and intercostal muscles at necropsy (Figure 1).

Figure 1 99mTc-THY scintigraphy ventrodorsal images showed increased uptake areas corresponding to the liver, lungs, and unexpectedly, to the right kidney.
Histopathological studies revealed a simple type of invasive tubular mammary adenocarcinoma spreading into the dermis with extensive tumor necrosis, and peripheral lymphocytic infiltrate (Figure 2A). Tubular adenocarcinoma metastases of probable mammary origin with tumor necrosis and moderated mitotic activity were found in the lungs, liver, right kidney, and intercostal muscles (Figures 2 B-D).
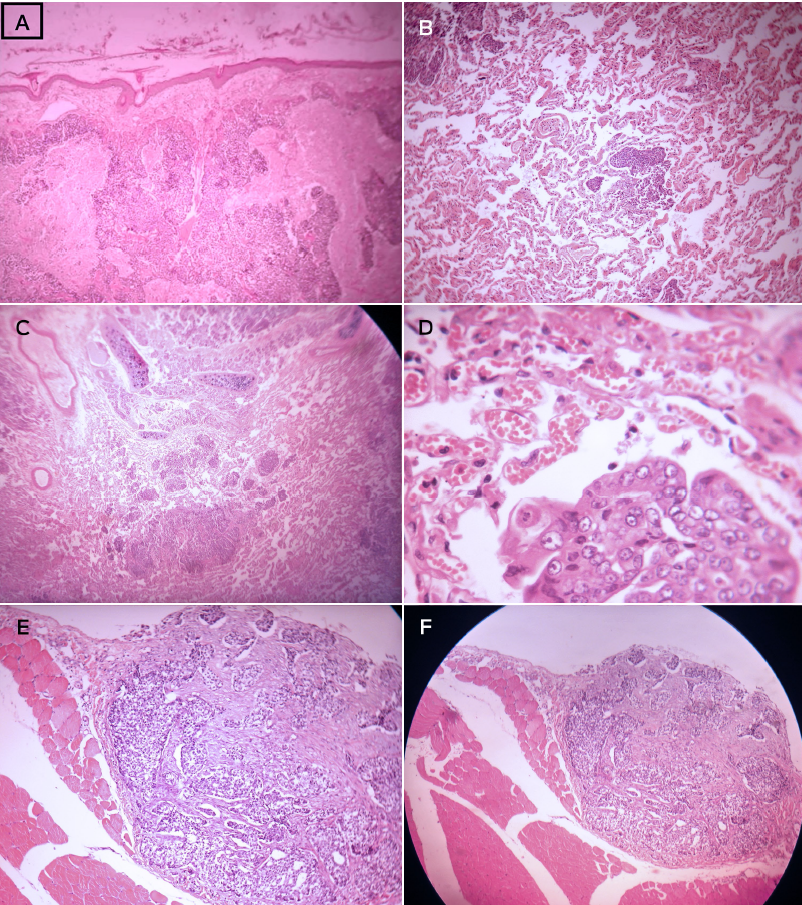
Figure 2 Histological images of feline mammary adenocarcinoma stained with hematoxylineosin (HE). 2A) Dermis invasion with focal points of tumoral necrosis (201 x 151 mm). 2B) Pulmonary metastases of a feline mammary adenocarcinoma (100x, zoom 2,0-201 x 151 mm). 2C-D) Right kidney adenocarcinoma metastases (20x and 40x, respectively). 2E-F) magnification of 10x and 4x, respectively..
Over 80% of cats' mammary gland masses are malignant,23 and the most common are adenocarcinomas.8 Squamous cell carcinomas, melanomas, hemangiosarcomas, and mammary carcinomas commonly metastasize to lungs, with a smaller likelihood of spreading to other tissues.1-4,6,8,24-26 Although tumors can occur at any age, they are more common in elder animals.
According to Sorenmo et al.,5 primary pulmonary tumors are rare in cats, which suggests that when found they may have mammary gland origin. Recent studies reveal that over 80% of mammary gland tumors in cats are malignant with a rapid progression and metastasizes at early stages.27 Earlier results show that mammary metastases occur in 50-90% of cases, with lymph nodes (83%), lungs (83%), pleura (22%), and liver (25%) being the most affected organs.8 Although we could not update the aforementioned data, De Campos et al. analyzed 37 queens and found that 35.13% of metastasis from mammary gland tumors were in regional lymph nodes. Additionally, metastases occur in all the epidermoid carcinomas, in 90% of anaplastic carcinomas, and 50% of the adenocarcinomas.28 Moreover, the ratio for thoracic metastases in malignant tumors is 15.9%.29 The limitation of conventional radiologic methods is the late identification of metastases, which results in less effective treatment and leads to a dim prognosis. Accordingly, chest radiographs are only able to detect pulmonary nodules larger than 4-5 mm, and their sensitivity to detect pulmonary metastases is estimated at 65 to 97% if held at least in two projections (right lateral and ventrodorsal/dorsoventral). However, this technique increases its reliability when performed in three projections (left and right side and ventrodorsal/dorsoventral).7,20,31
The cat in this study was referred to our hospital with only two X-ray projections performed two months before. Consequently, the scintigraphy results could not be compared with the X-ray findings.
Scintigraphy is widely used in horses, dogs and cats. Usually, osteosarcomas and lymphomas are staged in dogs with Technetium-labeled scintigraphy. Nonetheless, 99mTc scintigraphy labeling is more sensitive than radiography and computed tomography for skeletal imaging, and metastatic neoplasia.32,33 Moreover, scintigraphy is applied to assess thyroid dysfunctions,34 renal perfusion,35 portosystemic shunts,23 and gastric emptying time experiments36 in cats. In our study, thymine was labeled with 99mTc, proving to be effective for the detection of primary tumors and metastases.32,37
In light of our results, we suggest the expansion of scintigraphy use for metastatic lesion evaluation in the thoracic and abdominal cavities due to its sensitivity to early neoplasia stage detection when compared against other available imaging methods. One additional advantage of the scintigraphy is that it exempts particular incidences to acquire images when compared to X-ray examination that demands at least three projections (right-lateral, left-lateral, ventrodorsal or dorsoventral) for an adequate sensitivity.38 Moreover, the whole body can be studied with a single 99mTc-thymine dose. In this study, we detected metastases in the right kidney that was utterly unexpected. We believe that scintigraphy has been underused in veterinary care, especially in feline cancer imaging and treatment, as its primary use is for thyroid disease diagnosis.33
Traditional imaging methods are not able to detect secondary neoplasms due to their lack of sensitivity. However, scintigraphy is not a substitute for histopathologic examination on the determination of cancer stage, even if it can be an essential tool for choosing appropriate therapy and establishing prognosis.
Conclusion
In our study, the necropsy and histopathological findings were well correlated to 99mTc-THY results, both in the thoracic and abdominal cavities, especially since an otherwise undetected metastasis in the right kidney was found. Therefore, scintigraphy can be an adequate, reliable, non-invasive method to identify metastasis in feline patients with mammary adenocarcinoma. A limitation of this study is that no concomitant ultrasound or radiographic examinations were performed for comparison between techniques. Nonetheless, necropsy and histopathology validated the scintigraphy observations.











 nueva página del texto (beta)
nueva página del texto (beta)



