Introduction
The uterus is an organ with a remarkable capacity for cyclic renovation throughout the reproductive life of females. The human endometrium is formed of a functional layer and a basal layer and goes through approximately 400 cycles of proliferation, differentiation and detachment during a woman’s reproductive life.1 During each menstrual cycle, approximately 4 to 7 mm of tissue is regenerated during the proliferative phase.2 Species that have an oestrous cycle include cycles of endometrial growth and cell apoptosis. Endometrial renovation in every mammal is regulated by oestrogen and progesterone secretion.1-3 The level of endometrial tissue regeneration is similar to that of tissues where the existence of stem cells has been demonstrated, such as the intestinal epithelium, epidermis and bone marrow (BM).4
The hypothesis that endometrial regeneration (particularly in humans) was mediated by stem cells was postulated many years ago.5 Over 70 years ago, the first indications of a stem/progenitor cell presence in the uteri of rhesus monkeys was published; complete regeneration of the uterus was observed after an almost total resection of the endometrium.6 Clinical cases have also reported endometrial renovation in women even after resection that can support gestation.7-9 Bone and cartilaginous tissues have been found in the endometrium,10-12 suggesting the presence of mesenchymal stem cells (MSCs). Despite the aforementioned findings, the first evidence for the presence of MSCs in the human endometrium based on functional testing was relatively recent.13
MSCs are a cell population that can be differentiated in vitro into various cell lineages, including osteogenic, chondrogenic, adipogenic, myogenic, tenogenic and stromal cells.14-16 These differentiations can be identified using staining, such as oil red O (for lipid vesicles), alizarin crimson (for osteogenesis), von Kossa (for calcified extracellular matrices) or alcian blue (for sulfated proteoglycans).17 The Mesenchymal and Stem Cell Tissue Committee of the International Society for Cellular Therapy proposed the following criteria to define human MSCs18: (1) MSCs adhere to the culture tray when maintained under standard conditions and form fibroblast colony-forming units (CFU-Fs); (2) MSCs express the CD105, CD73 and CD90 markers but do not express the CD45, CD34, CD14 or CD11b, CD79 alpha or CD19, and HLA-DR surface molecules; and (3) MSCs can be differentiated in vitro into osteoblasts, adipocytes and chondroblasts.
MSCs have been found in foetal blood, amniotic fluid, the placenta, and the umbilical cord. In adults, MSCs are resident cells in the BM and in many other organs and tissues, including adipose tissue, the dermis, intervertebral discs, teeth, peripheral blood,14,16 and the endometrium.1 As a prominent tool in regenerative medicine, cellular therapy is a strategy that consists of substituting damaged cells or tissues with the aim of restoring their altered functions following provocation by different causes, including disease, congenital malformations and trauma. Generally, MSCs possess the following four relevant biological properties that allow them to be considered an option for cellular therapy: (1) a high capacity for cellular differentiation into different cell types (plasticity); (2) low immunogenicity; (3) an ability to secrete various factors that are responsible for tissue renovation; and (4) an immune regulation capacity (or immunomodulation ability).19
An advantage of the endometrium compared with other MSC sources is the accessibility of MSCs and the amount of sample that can be collected. In domestic animals, these cells can be obtained through hysterectomy, with the advantage of removing the entire organ containing these cells instead of a small sample. In humans, MSCs can be obtained through an endometrial biopsy, which is a procedure that does not require anaesthesia and is less invasive and less painful than a marrow aspiration or liposuction.20 Therefore, the endometrium can be considered a good MSC source. The aim of this review is to present an updated outlook of the knowledge regarding endometrial MSCs and their possible applications in veterinary medicine.
Endometrial origin of MSCs
The female reproductive system originates from the intermediate mesoderm. Some cells are thought to undergo a transition from the mesenchymal to epithelial lineage as the tissue proliferates to form a coelomic epithelium, which will subsequently invaginate to form paramesonephric or Müller ducts.21 One hypothesis regarding the origin of endometrial MSCs is that a few epithelial cells and MSCs remain in the adult endometrium.22
A second possible origin for endometrial MSCs is the BM. BM-MSCs have been reported to circulate in small numbers and can be established in other organs,23 where they perform a transdifferentiation process to originate into cells of the new tissue or contribute to angiogenesis.24 To prove this hypothesis, some BM-MSC screening assays have been conducted using cells grafted into women through transplants. Significant chimaerism was detected in one of these assays in 0.2 to 52 % of the glands and in the endometrial stroma of women who received a BM transplant, suggesting that the BM-MSCs contributed to endometrial regeneration.25 However, another study in which women were transplanted with male donor bone marrow suggested that endometrial cells were more likely to be produced by the resident endometrial stem cells,26 which are responsible for uterus regeneration, although small amounts of endometrial cells were found in the recipients’ endometria.27
Endometrium stem cell phenotype
Cultured endometrial MSCs usually express typical BM-MSC markers, such as CD90, CD105, CD14628, CD9, CD13, CD14, CD29, CD31, CD44, CD73, CD117 and CD13318, but they do not express other markers, such as STRO 1, CD31 (typical of endothelial origin cells), or CD34, from haematopoietic stem cells (HSCs) and endothelial cells.29
General adult stem cell markers, such as bcl-2, c-kit (CD117) and CD34, have been identified in human endometrial tissue.30 Additionally, Oct-4 has been reported to be expressed in almost half of the analyzed human endometrial samples.31 Sporadic expression of the NANOG and SOX 2 pluripotency-associated genes has also been reported in the endometrial stromal cells of pigs.32
Using flow cytometry analysis, cells with a HSC (CD34 and CD45) phenotype and co-expression of the CD7 and CD56 markers (which appear to be lymphoid precursors) have been identified in human endometrial suspensions33; this finding may be due to the presence of small numbers of haematopoietic stem cells in the samples.
Cells originating from menstrual secretions express the CD9, CD29, CD41a, CD44, CD59, CD73, CD90 and CD105 markers.34 Endometrial MSCs have also been purified based on the co-expression of two perivascular markers (CD140b and CD146).35 Masuda et al.36 found that the W5C5 (SUSD2) perivascular protein was a marker that could be used for human endometrial MSCs. Finally, Ishikawa et al.37 demonstrated that NAC1, which was a transcriptional repressor that was implicated in the auto-renovation and maintenance of pluripotentiality in embryonic stem cells,38 was over-expressed during the proliferative phase of the normal endometrial menstrual cycle.
Endometrial MSCs in humans
The first evidence for the existence of stem cells in the human endometrium was presented by Dr. Caroline Gargett and her research group,13 who analyzed endometrial tissues obtained from women undergoing a hysterectomy. They purified and cultured the cells and found that a small number of isolated cells could form individual colonies.13 This result indicated that the cells exhibited clonogenicity and a high proliferation capacity, both of which are stem cell characteristics. These isolated cells showed MSC features, because they were able to differentiate into the adipogenic, chondrogenic, osteogenic and smooth muscle lineages.39
MSCs obtained from the human endometrium have been demonstrated in vitro to have a better capacity to differentiate into mesoderm lineages than cells obtained from adipose tissue. Moreover, endometrial MSCs are able to differentiate not only into the osteogenic, chondrogenic and adipogenic lineages but also show an apparent plasticity since they are capable of differentiating into cardiomyocytes, respiratory epithelial cells, neuronal cells, pancreatic cells and hepatic cells.34,40 Furthermore, the possible use of these cells in the treatment of myocardial infarction has been suggested due to their angiogenic capacity.41
The ability of human endometrial MSCs to regenerate tissue has been demonstrated in experimental models with xenografts. Transplant of purified suspensions of human endometrial MSCs under the renal capsule of NOG mice, which lack T and B lymphocytes and NK cells, has achieved the generation of endometrial,42,43 and myometrial tissue layers in the uterus.44
Stem cells use an ABC transporter (ATP binding cassette) in their cellular membrane to eliminate toxins. Therefore, proteins of the ABC superfamily may be used as markers to identify and characterize stem cells based on the elimination of the Hoechst 33342 vital DNA dye from the cytoplasm by these transporters. This elimination process may be visualized using flow cytometry, resulting in side population cells.45 Based on verapamil inhibition studies, two proteins of the ABC superfamily can be considered responsible for active transport in stem cells: ABCB1 (also known as MDR1) and ABCG2.46,47 The phenotype of these side population cells has been suggested to be a universal marker for adult stem cell activity.48
In vivo assays have demonstrated that endometrial side population cells may be genuine stem cells.40,42,49 These assays transplanted these cells under the renal capsules of immunodeficient ovariectomized mice administered oestradiol and progesterone for eight weeks who were subsequently subjected to nephrectomy. The results showed that all grafts reconstituted tissue similar to the endometrium under the renal capsules.49
Endometrial MSCs in mice
The mouse is a very well-established animal model for studies of endometrial functions. Female mice undergo approximately 80 oestrous cycles throughout their reproductive life. Each cycle lasts four days,26 during which time the endometrium undergoes cellular proliferation and apoptosis cycles. Several studies have been conducted in female mice following the removal of their ovaries (thus removing the main progesterone and oestrogen sources). The following results were obtained: (1) oestrogen-sensitive cells undergo apoptosis; (2) an atrophic endometrium has very few glands; (3) the epithelial lining is dramatically increased; and (4) a dense stroma is generated within a 10- to 14-day period after surgery.50 These studies demonstrated that important regeneration of the endometrium could be induced through the administration of exogenous oestrogen.50-52
The presence of epithelial and endothelial cell populations has also been reported in the endometria of cycling mice expressing mTert (Telomerase reverse transcriptase).53 Because adult stem cells have slow cycles and divide only during tissue replacement to replace lost cells, they can be identified in vivo using the ligase chain reaction (LCR) technique. These studies have been conducted in mouse uteri marked with bromodeoxyuridine (BrdU).52,54-57 BrdU is a molecular analogue of thiamine and is used by the cells in place of the original nitrogen base during cellular multiplication periods. As a result of this procedure, cellular populations with a slow division cycle are identified as stem/progenitor cells or label-retaining cells (LRC),55 whereas cells that divide rapidly (which do not correspond to stem cells) dilute the label. In these studies, immunohistochemistry was also used to locate epithelial, stromal and myometrial cells positive for BrdU, which revealed their locations and some components of the cellular niche.51,54,57 A total of 6 % of stromal cells can be identified as LRCs after a period of 84 days. In these studies, 40 % of the LRCs were located near the endometrium-myometrium union.51
LRCs are negative for CD45 expression.51,57 Additionally, epithelial LRCs lack alpha oestrogen receptor (ER-α) expression, whereas epithelial and stromal neighbour cells (identified as non-label-retaining) are indeed positive for ER-α expression. Hence, oestrogen has been suggested to stimulate endometrial proliferation indirectly through cellular niches for endometrial MSCs.4 However, only a portion of LRCs correspond to stem cells.56
Endometrial MSCs in cows
The presence of cells in the bovine endometrial stroma capable of differentiating in vitro into the osteogenic lineage that possess characteristics related to BM-MSCs has been reported.58 Cabezas et al.59 studied the uteri of healthy Holstein cows at the beginning of the oestrous cycle luteal phase (days 1-5 post-ovulation) and during the luteal phase (between days 13 and 18 post-ovulation) to search for stem cells. These authors were able to identify the expression of markers for embryonic stem cells (OCT4 and SOX2) and MSCs (STAT3, CD44 and c-KIT) in the cow endometria during both periods of the oestrous cycle luteal phase. Cell lines obtained in the late luteal phase were induced to differentiate into the osteogenic and chondrogenic lineages; these differentiations were determined using alizarin crimson and alcian blue staining, respectively.59
Endometrial MSCs in pigs
In pigs, some cells have been isolated from the uterus with the ability to differentiate in vitro into the adipogenic and osteogenic lineages. These cells express MSC markers, such as CD73, CD29, CD90, CD105,32 CD44, CD144, CD105 and CD140b, and are negative for the presence of HSC markers, such as CD34 and CD45.60
Using the Hoechst 33342 fluorescent dye and cytometry analysis, Bodek et al.32 was able to identify side population cells that might be responsible for the regeneration process in the porcine endometrium. Using an antibody against ABCB1 (MDR1), the authors determined that the side population cells resided between the stroma and the epithelial layer in the pig endometrium during the 19th day of the oestrous cycle. In this same work, the stromal cells isolated from the pig endometrium on days 2-4 and 19 of the oestrous cycle proliferated and produced colonies. Moreover, the cells differentiated into the osteogenic, adipogenic and chondrogenic lineages.32
Endometrial MSCs in ewes
The presence of a small population of CD271-positive and CD49-negative stromal cells has been reported in the ewe endometrium. This cell population has a perivascular location, can differentiate into the four mesodermic lineages (adipogenic, osteogenic, chondrogenic and muscular) and shows a high cloning efficiency.61
Immune modulating effects of endometrial MSCs
The uterus is an organ with privileged and unique immunological characteristics that allow it to host a semi-allogeneic organism (foetus) in an exceptionally tolerant environment.62 Many studies have shown that MSCs escape immune recognition and inhibit the immunological response.14,63 MSCs may play an important role in the maintenance of immune homeostasis by preventing the inappropriate activation of T lymphocytes and generating a tolerant environment or stopping the immunological response during reparation.64,65 This function is a very important feature because it facilitates the clinical allogeneic use of these cells in regenerative medicine.
MSCs may inhibit dendritic cell maturation and hence prevent T lymphocyte activation. Additionally, they diminish the proliferation and cytotoxic activity of NK cells.66,67 MSCs have been reported to have low or absent expression of the major histocompatibility complex (MHC) class II protein,14 which represents a great advantage when they are used for allogeneic cell therapy (Figure 1).
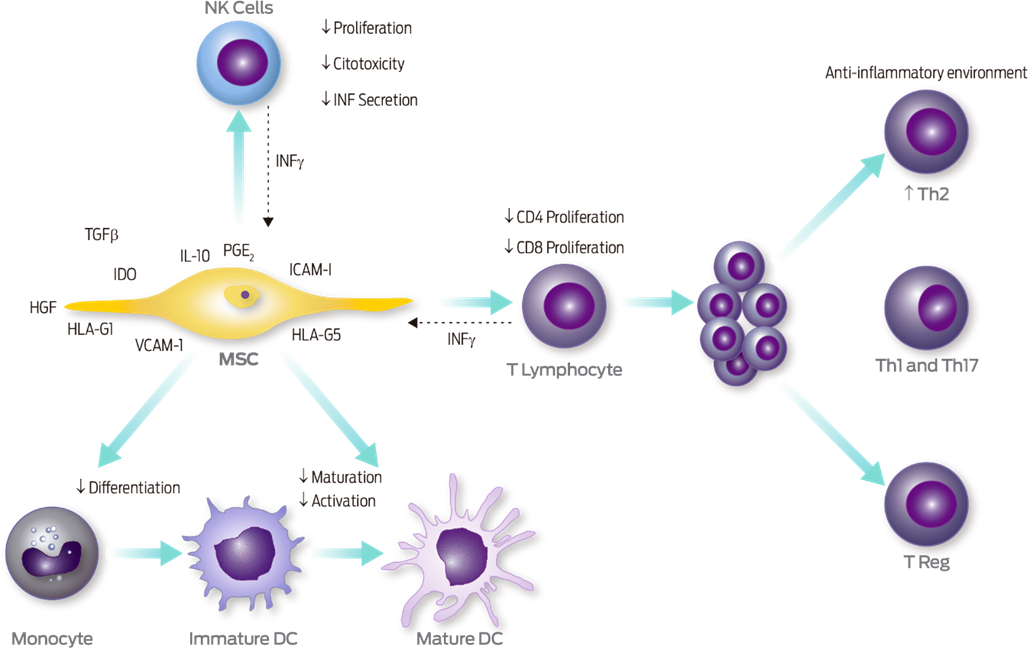
Figure 1 Immunoregulatory ability of MSCs. MSCs regulate the functions of NK cells, dendritic cells (DC) and T lymphocytes. The immunosuppressive effect may occur through the secretion of different factors or through cellular contact (black arrows). The former pathway involves TGFβ, HGF, IL-10, PGE2, and HLA-G5, whereas the latter pathway involves the products of IDO enzyme activity, PD-L1, HLA-G1, ICAM-I and VCAM-I. Pro-inflammatory cytokines (IFN-γ) secreted by NK cells and activated T lymphocytes favour the immunoregulatory activity of MSCs (dotted lines), because they increase or induce the secretion of molecules that regulate the functions of the distinct cellular components of the immune system. Modified from Montesinos et al., and Ma et al.19,66
Menstrual endometrial stem cells from healthy women have been shown to inhibit the appropriate differentiation from monocytes into mature dendritic cells in vitro. This effect was attributed to IL-6 and IL-10 production because the levels of these cytokines were increased in the culture medium.68 Due to their immune suppressing properties, MSCs may be a good option for autoimmune diseases, such as systemic lupus erythaematosus, diabetes type I and multiple sclerosis.69 However, the presence of MSCs with immune modulating characteristics must be taken into account in the tumour microenvironment because these cells may have important implications for tumour growth.70 The presence of MSCs in tumours has been suggested to benefit the growth of the tumour via an immune suppressing process that favours the ability of tumour cells to evade the immune system.70 These findings may limit the clinical use of these cells.
Potential clinical applications of endometrial MSCs
Regenerative medicine offers the potential for the replacement or repair of different types of cells within damaged tissues or the tissues themselves, typically through cell therapy or tissue engineering. Stem cells are critical for these approaches; indeed, the involvement of the BM in the differentiation of stem cells to non-haematopoietic cells has been well demonstrated. Furthermore, the contribution of BM-derived stem cells in the promotion of neoangiogenesis has been demonstrated not only in animal models but also in human clinical trials with an excellent safety profile.
Recent evidence indicates that the endometrium is a tissue with the potential for regeneration using these approaches. The presence of donor cells in the endometria of women receiving BM transplantations suggests a haematopoietic source with the ability to renew this tissue. Here, we describe the role of cell therapy with BM-derived stem cells for the treatment of endometrial dysfunction in Asherman’s syndrome and/or endometrial atrophy in humans and murine models. Additionally, the emerging field of tissue engineering has recently been applied to reproductive tissues beyond the endometrium with elegant studies involving humans and animal models.
Currently, most studies on the biology of MSCs have used BM-derived MSCs. Similarly, most of the literature has described the application of MSCs from this source for cell therapy protocols.66,71 Recent evidence indicates that the endometrium can be regenerated by BM-MSCs due to their capacity to promote neoangiogenesis and modify cellular fibrosis. Thus, in a rat model of severe uterine injury, BM-MSCs loaded onto degradable collagen membranes resulted in higher bFGF, IGF-1, TGFβ1 and VEGF levels in the wounded tissue adjacent to the collagen/BM-MSC constructs at four weeks post-transplantation compared to the corresponding tissues in rats who received the collagen construct alone or in the spontaneous regeneration group. Moreover, the collagen/BM-MSC system increased the proliferative abilities of the uterine endometrial and muscular cells, facilitated microvasculature regeneration, and restored the ability of the endometrium to receive an embryo and support its development to a viable stage.72 Moreover, CD133+ BM-derived stem cell (BMDSC) autologous cell therapy may be useful for the treatment of some pathologies, such as patients with refractory Asherman’s syndrome (AS),73-75 which corresponds to a replacement of the endometrial stroma by fibrous tissue and the complete disappearance of the endometrial structure (Donnez and Nisolle, 1994).74,75 Autologous cell therapy using CD133+ BMDSCs in conjunction with hormonal replacement therapy increased the volume and duration of menses as well as the thickness and angiogenic processes of the endometrium while decreasing the intrauterine adhesion scores within the first three months (Santamaría et al., 2016).73,75 Furthermore, BMDSC transplantation in a murine model of Asherman’s syndrome improved fertility in the mice, demonstrating a functional role for these cells in uterine repair.76
Many reproductive alterations are associated with abnormal endometrial proliferation; therefore, endometrial MSCs may perform an important role in the physiopathology of diseases, including human endometriosis, adenomyosis, and infertility problems related to hypoplasia or endometrial atrophy,53 and probably in some important diseases within veterinary medicine, such as cystic endometrial hyperplasia in dogs, equine endometriosis and endometrial cancer. However, these roles have not been demonstrated to date. Endometrial MSCs are responsible for endometrial renovation during each oestrous cycle. Therefore, a decrease in the numbers or functions of these cells may result in a thin endometrium that is unable to support embryonic implantation,77 as occurs in women going through menopause. However, administration of hormone therapy to these women causes the epithelial, stromal and blood vessel cells to proliferate and differentiate.78 Regeneration resulted in the formation of a thick endometrial layer that was able to support gestation even in women over 60 years of age who were able to have children by an in vitro fecundation technique.79 In humans, the possibility of using endometrial MSCs for the treatment of Asherman’s syndrome has been explored. This syndrome is characterized by uterine atrophy and the production of adherences to the endometrium due to trauma, which produces infertility as a consequence.53
In equines, endometriosis is a chronic degenerative disease produced by chronic inflammation that causes infertility in mares; this disease originates in endometrial fibrosis and uterus gland alterations.80-82 Currently, no effective treatments are available for this disease, although the administration of MSCs from adipose tissue has been shown to prevent its progression.83 Therefore, an endometrial MSC treatment for this disease from the same or an allogenic animal source may produce better results. In humans, endometriosis is a chronic disease that is characterized by the presence of endometrial glands and stroma outside of the uterine cavity.84 Endometrial MSCs have been hypothesized to play a significant role in the physiopathology of this disease.53 Currently, efforts are being undertaken to acknowledge the real participation of these cells and to design a strategy for the treatment and control of this disease. Cystic endometrial hyperplasia/pyometra is a poly-systemic disorder that may be chronic or acute, is present in adult female dogs, and is characterized by endometrial hyperplasia associated with high progesterone and oestrogen production that is generally complicated with an ascending infection.85 The pathogenesis of this disorder may be related to the oestrogen-endometrial stem cell interaction. This interaction has been observed in mice, where the presence of endometrial MSCs has been suggested.51 Furthermore, several studies have surgically removed the ovaries to produce endometrial atrophy within a 10- to 14-day period50; then, an important regeneration of these structures was induced by the administration of exogenous oestrogen.50-52 Although there are no reports to date regarding the existence of MSCs in female dogs, this hypothesis is interesting and warrants further study.
Apart from the common mesodermal lineages, endometrial MSCs may be induced to differentiate in vitro into skeletal and cardiac muscle,86,87 insulin-producing cells88 and the urinary epithelium89 in the endodermic lineages and finally into neuronal cells [similar to neurolemmocytes, Schwann cells],90,91 and dopaminergic neurons91 in the ectodermic lineages.28,92,93 Therefore, these cells might be used to treat affections such as cardiac disease, muscle degeneration, diabetes type 1 and neurodegenerative diseases in the future.
The possibility of using endometrial MSCs differentiated into uroepithelial cells along with an adequate scaffolding has been explored to fabricate a transplant substitute for the urinary epithelium for patients with bladder damage due to carcinoma, trauma or infection.89 Recently, the transplant of endometrial MSCs into the caudate nucleus of vervet monkey (Chlorocebus sabaeus) brains induced with Parkinson disease signs through administration of the 1-metil-4 fenil-1, 2, 3,6-tetrahidropiridina (MPTP) neurotoxin has been demonstrated to produce cells with neuronal morphology in vivo that also express tyrosine hydroxylase (TH). Thus, this procedure increases the TH-positive cell numbers to form dopamine metabolite concentrations within the in vivo transplant site. The aforementioned results suggest that endometrial MSCs may be used for the treatment of this disease in the future.94
MSCs may be useful for tumour treatment. In this regard, Han et al.95 reported that the administration of endometrial stem cells either intravenously or intratumourally in a glioma inhibited the growth and reduced the tumour size in more than 45 % of cases; these effects were associated with the inhibition of neo-vascularization.95
The endometrium is the site where physiological angiogenesis occurs in adults. This process uses regenerative cells that cyclically form tissues, which detach without leaving any scars.96 Angiogenesis is crucial in the context of cardiac regeneration (after one year) due to ischaemic damage.96 The uterus has been demonstrated to be a source or progenitor cells that induce angiogenesis when injected into a heart that has suffered infarction.97
Some immune privileged sites in organisms have low or absent MHC I protein expression on their cell surfaces.98 The uterus has a high percentage (> 20 %) of cells that are MHC I-negative96; however, whether these cells are stem cells has not been proven. The benefits of an intramyocardial injection of MHC I-negative allogeneic cells after a myocardial infarct are comparable to those of syngeneic BM cell transplants. MHC I-negative cells have been reported to preserve cardiac functions, decrease the infarct size and improve regeneration after a myocardial infarction.96
Human endometrial MSCs may restore functions in damaged ovaries. Mice subjected to ovary damaged through busulfan and cyclophosphamide administration (both drugs produce toxicity to germinal cells) followed by experimental treatment with an intravenous injection of endometrial MSCs exhibited improvements in weight and oestrous cycle presentation and restored fertility. Exhaustion of the germinal stem cell reserve induced by chemotherapy was also decreased.99 This evidence suggests a possible use of these cells as a cellular therapy for patients undergoing chemotherapy.
In addition to the reproductive scope, endometrial MSCs could be used in other fields of veterinary medicine for the treatment of a large number of diseases, such as (a) autoimmune diseases (i.e., rheumatoid arthritis, systemic erythaematosus lupus, and diabetes type 1), (b) cardiac affections (i.e., cardiac insufficiency), (c) lesions of the musculoskeletal apparatus (i.e., muscle degeneration, articular cartilage alterations, which are particularly important in equine osteoarthritis, and hip dysplasia in dogs), (d) urinary tract diseases (i.e., renal insufficiency), (e) neurodegenerative processes and spinal cord injuries, (f) tumour treatment by inhibiting the growth and reducing the tumour size, (g) development of pharmacological products for the study of drug toxicity or in vitro efficacy, and finally (h) the generation of animal models for the study of human diseases and diseases of veterinary interest. Additionally, endometrial MSCs may become an important tool for veterinary tissue engineering and regenerative veterinary medicine.100-102
Conclusions
The immune modulating capacity of MSCs facilitates their allogeneic clinical use in regenerative medicine and may have important implications for tumour growth. The endometrium is an alternative and accessible source of MSCs in humans, mice, cows, pigs and ewes. However, this capacity must be determined in these cells. In addition to the common mesodermic lineages, endometrial MSCs can differentiate into the endodermic and ectodermic lineages. Thus, in the future, these cells might be used to treat affections, such as cardiac disease, muscle degeneration, diabetes type 1 and neurodegenerative diseases.
The study of endometrial MSCs in domestic animals is a new and promising field because our improved understanding of the physiology and biology of these cells will help elucidate the physiopathology of reproductive diseases, such as cystic endometrial hyperplasia in dogs and equine endometriosis, and contribute to the proposal of new treatments. MSC studies can also help clarify and treat infertility problems due to hypoplasia or endometrial atrophy.
Although the endometrium seems to be a promising source of MSCs, several assays must be conducted before possible clinical applications can be considered. Furthermore, many basic investigations need to be performed to compare the biological aspects of these cells with other MSC sources, especially the bone marrow.











 nueva página del texto (beta)
nueva página del texto (beta)



