Introduction
Different methods are available to evaluate the degree of bone healing that are as simple as the transmission of complex sound waves (ultrasound) or as complex as bone densitometry and computed tomography. However, the cost-benefit ratio does not justify the use of the latter on a regular basis. A good choice involves employing optical techniques and taking into account the optical properties of tissues because it is possible to differentiate them according to their densities.
When collimated light is applied on a surface of any material, a fraction of it is absorbed to generate heat or perform photochemical reactions. The remaining portion is dispersed and may pass through the surface if it has sufficient power. However, the incident light might be reflected from different internal structures to the surface. This reflection depends on the optical properties, particularly the optical absorption coefficient, which is characteristic of each material. Infrared light is reflected in solids and absorbed in liquids. When the wavelength of 940 nm is applied to human skin, the IR radiation reaches muscle or bone with minimal losses due to its low optical coefficient of absorption.1,2 In the case of the fracture line, bone fractures consolidate with time, and reflection of IR radiation increases. Based on the nature of radiation (which does not change its frequency, but its intensity), it is possible to evaluate bone healing because it changes gradually over time. Thus, the optical properties depend on the level of bone consolidation (density of the fracture line), which is the starting point for the development of a device that uses a laser diode that emits IR light. Thus, we can observe how the fracture line is modified over time. A fraction of IR light applied on a tissue is reflected from all layers in pairs,3 as shown in Figure 1.
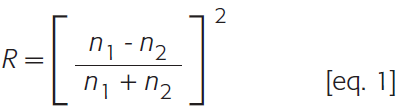
Reflection on the border of two layers of inhomogeneous tissue is known as diffuse reflection or Fresnel’s law4-6 and is calculated according to Equation 1.
Equation 1
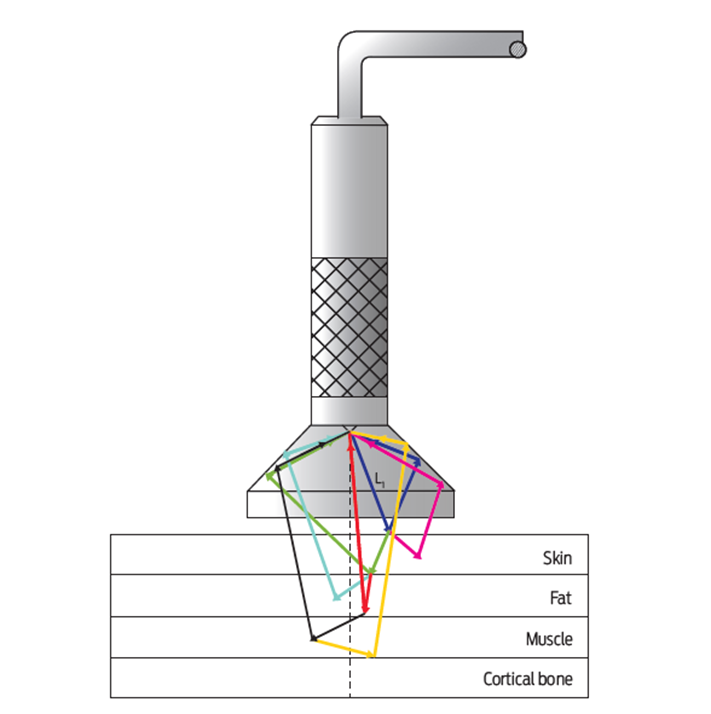
Figure 1 Laser light applied and reflected from the different tissue layers. This light is collected by the sensor and is subsequently processed.
RT total reflection was not strictly calculated, but the intensity detected with a photo sensor through an optical fibre corresponds to the optical response of all the tissue layers.7,8 To assess bone consolidation, two observations were made in this work: first in the contralateral zone, which is considered as a reference at 100 % consolidation independent of bone density, and then subcutaneously in the fracture line. The final reading is displayed on the computer as a percentage and is obtained using the program for the Arduino board. The main argument for developing this program assumes that an increase in bone density is directly proportional to the time elapsed.
Background
Since the discovery of X-rays in 1895, it is possible to offer a diagnosis and treat bone fractures with scientific rigor. Another development that contributed to the field of orthopaedic trauma was computed tomography, which was invented in 1972. By using this technology, a bone can be observed through cuts in three dimensions with a precision of millimetres. It is possible to know the shape of a fracture line and its location, but it does have a problem when determining bone quality. For this purpose, bone densitometers were designed to assess the bone density gradients in the same bone by using laser light scanning. For this procedure, it is necessary to know the optical parameters of the tissues to be studied and to have mathematical software that allow the behaviour of a tissue to be modelled,9 or an assembly of tissues to obtain the desired graphic or image response. Regarding the study of the optical properties of the tissue, the first studies reported date to the time when Beer’s Law was unveiled.10 By using this application, only one tissue could be analysed by the incidence and transmission of a beam of monochromatic light.
In 1981, Wan et al. developed a theoretical model to explain the reflection and transmission of multilayer diffuse structures, such as human skin.11 They conducted an experimental study in sheep’s abdomen and chest skin. In 2000, The London College University in England performed a study of human skin in which the optical absorption coefficients of human skin were known in black and Caucasian skin.12,13 Thus, it is possible to understand the set of values of the broad range of human skin shades (optical properties of the skin). Cook conducted a study in 1993 to calibrate an X-ray device and used aluminum to simulate transverse and oblique fractures, finding that it was possible to detect fractures on the order of 0.05 mm. In his article, he noted that the fracture callus can exhibit an up to 20 % increase compared with the healthy contralateral side two weeks after attachment plate removal. He also mentions that the progress of consolidation for patients treated with an external fixator may be expressed as a percentage of the mineral density compared with the same site on the contralateral limb. Finally, he mentions that although the mineralization process is not linear with respect to time, it provides an idea of bone mineral density during the consolidation process.14
In 2002, Srinivasan et al. mentioned the reasons why devices containing any ionizing source, such as X-rays, are not fully recommended. In addition, he discovered that laser light in the range of 600 to 1 300 nm at low intensities does not represent a risk for health, thus prompting the development of new imaging technologies.15 The following year, a group of Australian researchers found that visible light is absorbed in the soft tissue.16 The incident intensity is reduced to 10 %. In contrast, when applying infrared light, it is reduced to only 5 %. In 2008, Krawiecki et al. developed a model to explain the absorption and scattering of light in human tissues. Using a mathematical model, he showed that dispersion and optical density can be considered the summation of a linear combination of coefficients and constants, whereas transmission can be considered a product of absorption and dispersion constants, which are characteristic of each tissue to be analysed. The model is consistent for a structure of up to eight different layers.17 Thus, it is clear that bone healing can be evaluated based on the change of the optical absorption coefficient, which depends on bone mineral density. Considering the experiences mentioned above, we believe that it is possible to design a device that provides information on the evolution of the fracture line versus time in a non-invasive manner.
Material and methods
Five New Zealand White (NZW) rabbits weighing 3 to 4 kg were used for this study with approval from the Bioethics Committee of the National Institute of Rehabilitation (INR-LGII). Care, feeding and use were performed according to the official standard NOM-062-ZOO99.
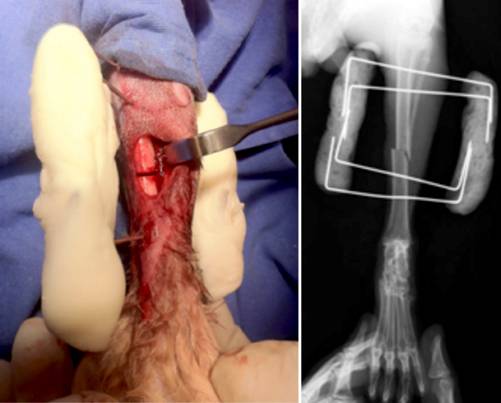
The procedure started by cannulating the marginal ear vein. Then, the left leg was shaved, and an anaesthetic was administered based on the rabbit’s the weight. Vital signs were continuously observed. Antisepsis was performed with isodine foam; sterile fields were placed, which allowed the left lower extremity to be exposed. Anatomical landmarks of the tibial anterior tuberosity and of the medial malleolus protrusion were identified. Then, an anteromedial approach of 1.5 cm in the middle third of the tibia was performed. The skin was dissected, and the tibial shaft was incised longitudinally. A 0.5 cm area of periosteum was stripped from the tibial shaft, and the cortical bone was exposed. Then, the osteotomy was performed using a handsaw. After the osteotomy, both fragments were fixed using an external fixator constructed with Kirschner nails and dental acrylic cement, as shown in Figure 2.
Results and discussion
Measurements were performed using IR light at the level of the fracture line from the first to the fourth week. The percentage of bone consolidation was in the range of 19-32 % for the first week, of 48-52 % after 23 days, and 64-73 % after 34 days.
Regarding computed tomography (CT), averages increased significantly from one measurement to another. The values increased from 419 in the first measurement to 700 in the second measurement and finally to 1080 in the third. Statistical analysis was performed using SPSS software version 17 (Friedman test for related samples p = 0.007). The CT results are presented in Table 1 at 7, 23 and 34 days after surgery.
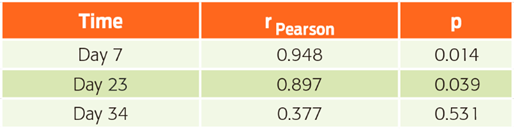
High Pearson correlation coefficients were observed between the first two measurements of the percentage of bone healing by IR light and postsurgical days. As time increased, the consolidation percentages increased. Of note (Table 2), the correlation coefficient decreased for the last measurement on day 34 after surgery in rabbit 5 at 73 %, which is in contrast to the minimum expected consolidation of 91.5 %. It is likely that rabbit 5 exhibited delayed consolidation for unknown reasons because it was apparently in good health. However, the CT results are not consistent with the IR light because rabbit 5 registered high CT values.
Table 2 Correlation coefficients of the percentage of consolidation measured by IR light with postsurgical advance days.
Finally, Figure 3 shows the overlapping correlations of CTs with consolidation percentage measured by IR light are shown, with the CT with postsurgical evolution days and consolidation percentage by IR light with postsurgical evolution days.
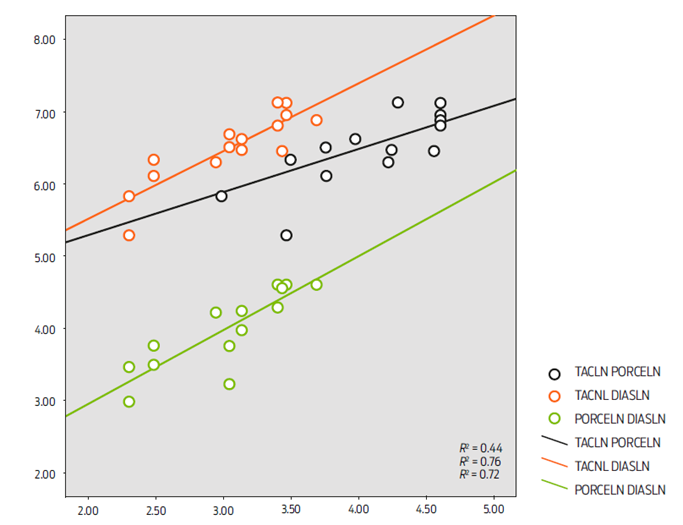
Figure 3 Superimposed scatterplots showing the relationships between variables. TAC LN PORCELIN = computed tomography (Hounsfield units) vs % of bone consolidation. TAC LN DIAS LN = days of experiment vs computed tomography (Hounsfield units). PORCELIN DIAS LN = days of experiment vs % of bone consolidation.
Conclusions
In this article, the functionality of a device that uses laser light IR (940 nm) to optically evaluate bone consolidation was estimated.18 The results obtained from only five rabbits are reported here given that the first rabbit died after the application of anaesthesia probably due to pre-existing health problems.
X-rays are useful to determine whether any fractures are present. However, X-rays do not indicate the progression of bone healing over time because the energy of X-rays can pass through the bone bridges that formed initially. Significant differences in terms of structural density can be observed until a maximum increase of osteoblasts occurs (typically on the fifteenth day after fracture reduction). In contrast, using optical methods, it is possible to observe significant changes starting on the third day. The reason for this sensitivity is that the optical absorption coefficient is altered depending on the level of cumulative mineralization and metabolism in the fracture, which depends on the time elapsed. Measurements made by means of IR light exhibit broad statistical correlation with the results obtained from the study of tomography. This fact underscores its use as a method of quantitative measurement of bone consolidation with significant potential in the clinic.
This study was conducted in an animal model (NZW rabbits 3-5 kg), which exhibits increased bone consolidation compared with humans. A proposal for the quantitative measurement in bone healing in humans is the next step to validate the use of IR light for fracture evaluation. It is important to make the necessary corrections to the device designed in this study.











 nueva página del texto (beta)
nueva página del texto (beta)