Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Sanus
versão On-line ISSN 2448-6094
Sanus vol.7 Sonora Jan./Dez. 2022 Epub 21-Mar-2023
https://doi.org/10.36789/revsanus.vi1.309
Review
Nursing intervention in neonatal metabolic screening: Integrative review
1Doctora en Ciencia de Materiales. Profesor de asignatura. Universidad de Sonora. Departamento de Enfermería. Enfermera en Hospital General “Dr. Fernando Ocaranza” ISSSTE. Hermosillo, Sonora, México.
Introduction:
Neonatal metabolic screening refers to a group of procedures and tests performed in order to separate among apparently healthy newborns, those with suspected inborn errors of metabolism. Therefore, it allows detecting the disease before it appears and initiating the treatment in time in order to prevent complications, disability and death. Currently, the neonatal metabolic screening is decisive for reliable results.
Objective:
Conduct an integrative literature review of nursing intervention in neonatal metabolic screening.
Methodology:
Integrative research in the databases Web of Science, Scielo, Scopus, Pubmed, Sciencedirect, Dialnet, OVID and EBSCO, using the descriptors neonatal screening, nursing care, inborn errors of metabolism, neonatology and analgesia; with the Boolean operators and, or and not. Of 116 documents obtained, 36 met eligibility criteria and represent the study material.
Results:
Blood sample collection for screening was performed between the third and fifth day of life, essentially by capillary puncture of the heel. Non-pharmacological analgesic measures are breastfeeding, kangaroo method and containment. The sample shall be protected from contamination, and its stability depends on the storage temperature until analysis is performed.
Conclusions:
The scientific literature reviewed empowers the nursing professional to provide comprehensive and safe care to the newborn who participates in the program.
Key words: Neonatal screening; Nursing care; Metabolism; Inborn errors; Neonatology. (DeCS)
Introducción:
El tamiz metabólico neonatal es el conjunto de procedimientos y pruebas que se realizan para separar entre recién nacidos aparentemente sanos, aquellos con sospecha de errores innatos del metabolismo. Por tanto, permite detectar la enfermedad antes que se manifieste e iniciar tratamiento oportuno para evitar complicaciones, discapacidad y muerte. Actualmente, es un programa neonatal prioritario para la salud infantil. En la etapa operativa, la estandarización de criterios es determinante para resultados confiables.
Objetivo:
Realizar revisión bibliográfica integrativa de la intervención de enfermería en tamiz metabólico neonatal.
Metodología:
Investigación integrativa en las bases de datos Web of Science, Scielo, Scopus, Pubmed, Sciencedirect, Dialnet, OVID y EBSCO, utilizando los descriptores tamizaje neonatal, atención de enfermería, errores innatos del metabolismo, neonatología y analgesia; con los operadores booleanos and, or y not. De 116 documentos obtenidos, 36 cumplen criterios de elegibilidad y representan el material de estudio.
Resultados:
La recolección de muestra de sangre para tamiz se realiza entre el tercer y quinto día de vida, esencialmente mediante punción capilar del talón. Las medidas analgésicas no farmacológicas son lactancia materna, método canguro y contención. La muestra debe protegerse de contaminación, y su estabilidad depende de la temperatura de conservación hasta su análisis.
Conclusiones:
La literatura científica revisada, faculta al profesional de enfermería para proporcionar atención integral y segura al recién nacido que participa en el programa.
Palabras clave: Tamizaje neonatal; Atención de enfermería; Errores innatos del metabolismo; Neonatología. (DeCS)
Introdução:
A triagem metabólica neonatal refere-se a um grupo de procedimentos e testes realizados a fim de separar entre recém-nascidos aparentemente saudáveis, aqueles com suspeita de erros congênitos de metabolismo. Portanto, permite detectar a doença antes que ela apareça e iniciar o tratamento a tempo, a fim de evitar complicações, incapacidade e morte. Atualmente, a triagem metabólica neonatal é decisiva para resultados confiáveis.
Objetivo:
Realizar uma revisão integrativa da literatura sobre intervenção de enfermagem na triagem metabólica neonatal.
Metodologia:
Pesquisa integrativa nas bases de dados Web of Science, Scielo, Scopus, Pubmed, Sciencedirect, Dialnet, OVID e EBSCO, utilizando os descritores triagem neonatal, cuidados de enfermagem, erros inatos de metabolismo, neonatologia e analgesia; com os operadores booleanos e, ou não, com os operadores booleanos. Dos 116 documentos obtidos, 36 preenchiam os critérios de elegibilidade e representavam o material de estudo.
Resultados:
A coleta de amostras de sangue para triagem foi realizada entre o terceiro e quinto dia de vida, essencialmente por punção capilar do calcanhar. As medidas analgésicas não-farmacológicas são a amamentação, método canguru e contenção. A amostra deve ser protegida de contaminação, e sua estabilidade depende da temperatura de armazenamento até que a análise seja realizada.
Conclusões:
A literatura científica revisada capacita o profissional de enfermagem a fornecer cuidados abrangentes e seguros ao recém-nascido que participa do programa.
Palavras-chave: Recém-nascido triagem; Cuidados de enfermagem; Erros inatos do metabolismo; Neonatologia (DeCS)
Introduction
Neonatal metabolic screening is the group of procedures and tests performed to separate among apparently healthy newborns (NB), those with suspected metabolic diseases, known as inborn errors of metabolism, which are characterized by an innate inability to carry out a metabolic process due to the absence or inactivity of an enzyme 1-5. Abnormal results of neonatal metabolic screening are not synonymous of disease; an integral evaluation of the neonate is required prior to the issuance of a confirmatory diagnosis. Screening is the first link in detecting the disease before it manifests and initiating timely treatment to avoid complications, disability and associated death 6-9.
In 1961, Dr. Robert Guthrie proposed the detection of phenylketonuria through drops of blood deposited on filter paper. Subsequently, his technique was used to identify other metabolic abnormalities, and neonatal screening was implemented in the United States in 1963 9-10.
In Mexico, the neonatal screening program for metabolic diseases was implemented in 1973 with the detection of phenylketonuria, galactosemia, maple syrup urine disease, homocystinuria, and tyrosinemia. The program was cancelled in 1977 and was reestablished until 1986 for congenital hypothyroidism and phenylketonuria. Subsequently, in 1988 the Ministry of Health made screening mandatory in institutions providing care to newborns 11. Currently, Article 61 of the General Health Law and NOM-007-SSA2-2016 and NOM-034-SSA2-2013 12) stipulates that neonatal metabolic screening is mandatory.
This neonatal screening is classified into basic and expanded according to the diseases that can be detected. In Mexico, by regulation, basic screening is performed on the newborn with a capillary blood sample from the heel, between the third and fifth day of life. The diseases to be detected are congenital hypothyroidism, congenital adrenal hyperplasia, phenylketonuria, galactosemia, biotinidase deficiency, glucose-6-phosphate dehydrogenase deficiency and cystic fibrosis 12-13. The expanded neonatal metabolic screening allows the detection of more than 76 metabolic diseases, according to laboratory technology 11,14.
As part of the operational process of this screening program, three basic stages have been proposed (a) pre-analytical, which includes sample collection, drying, storage and shipping, (b) analytical for processing, analysis and issuance of laboratory results, and (c) post-analytical stage, which includes from the delivery of results to the follow-up of suspected cases 12-15. All stages are essential to ensure the effectiveness of the program. However, among the main causes of altered results and samples rejected as inadequate for the laboratory are those related to the pre-analytical stage 16, which are interventions commonly performed by nurses working at the first level of health care.
Accordingly, the objective of this research is to carry out an integrative review of the nursing intervention in neonatal metabolic screening, with emphasis on its relevance, sample collection, drying, preservation and shipping procedures. The scope of this research is descriptive and explanatory; its importance is due to the fact that it synthesizes evidence that contributes to the successful intervention of the nursing professional in the operational stage of the neonatal metabolic screening program. In other words, in this area of care, the practice based on scientific evidence empowers nurses to improve interventions and enhances patient’s safety.
Methodology
The methodology is an integrative review of the literature, which provides evidence for the best nursing care practice in the proposed topic. The stages for its realization were: a) definition of the research question, b) search of scientific literature, c) evaluation of information, d) analysis and selection of research, e) interpretation of information, and f) synthesis and presentation of the review. The research question for this review was “What is the relevance of nursing intervention in neonatal metabolic screening?”. To answer this question, the literature search was carried out independently by the researcher in the databases Web of Science, Scielo, Scopus, Pubmed, Sciencedirect, Dialnet, OVID and EBSCO. The descriptors in Health Sciences (DeCS) were neonatal screening, nursing care, inborn errors of metabolism, analgesia, neonatology, and the Boolean operators AND, OR and NOT. The eligibility criteria were original researches that included in the title or abstract, interventions regarding neonatal metabolic screening, published in English, Spanish or Portuguese, during the period ranging from 1995 to 2021. In the case of documents published more than five years ago, those that provide basic evidence of the operability of the neonatal metabolic screening program were chosen. A total of 116 documents were found; 36 were chosen, consisting of articles, manuals and books, with a full text version available, which were classified into five categories: technical guidelines, reviews, case studies, descriptive, and neonatal analgesia. Abstracts of congresses, communications, dissertations, studies in children older than 28 days were excluded. Afterwards, an integrative analysis of the information was performed according to the PRISMA recommendation 17, with the algorithm proposed in Figure 1.

Source: Own-development
Figure 1 Identification, selection and inclusion process of research studies conducted in accordance with the PRISMA recommendation 17.
Results
On the basis of the findings, the following sections of relevant information have been identified for nursing intervention in the operational stage of the neonatal metabolic screening program.
Postnatal age and sample collection for neonatal metabolic screening: Identify metabolites present in congenital metabolic diseases; a blood sample is essentially taken between the third and fifth day of life of the newborn and collected on specific filter paper for metabolic screening 7,9,13,18-21. It has been reported that it should be performed within 24 to 48 h after birth, because before 24 h of life, elevated levels of phenylalanine markers have been found, findings that correlate with higher false positive rates for this condition. Additionally, the detection of some metabolic disorders may be impaired due to the biochemical transition of the neonate from a mother-dependent status to an autonomous status. Also, it has been suggested that sample collection after 48 h of life could delay diagnosis and initiation of timely treatment. The timing of sample collection may vary in preterm, low birth weight or other abnormalities at birth 18.
Sample collection methods
Venipuncture: Depending on the NB's health situation, as well as the extraction preferences used by the personnel of the laboratory, it is recommended to take a blood sample through venipuncture with short catheters, and its subsequent placement on filter paper for sieving. Collection in capillary tubes, as well as with needle and syringe increase the possibility of clot formation and hemolysis, in addition to damage to the filter paper when placing the sample and producing friction with needles 19. It has been reported that venipuncture is less painful and traumatic for the NB, and that the extraction time is less than that used in capillary heel prick, also that this method does not alter the results 4,19.
Umbilical cord sampling: This consists of extracting by needle puncture and syringe aspiration of a blood sample from a blood vessel of the umbilical cord that is cut in the NB immediately after birth, followed by placement on filter paper for neonatal screening. This sample only allows the identification of metabolites present in congenital hypothyroidism, so its practice rejects the possibility of detecting other metabolic diseases 13,20.
Heel capillary puncture: This is the method of choice for taking the sample, since it represents an alternative for extracting small volumes of blood quickly and easily, as it represents an area of great vascularization and relatively little nerve innervation. In addition, heel capillary puncture is a safe procedure when the anatomical characteristics of the NB foot are considered, as well as the asepsis specifications, material and equipment to be used. The puncture should be performed within the most lateral external or internal superficial area of the heel, and with a maximum depth of 2.4 mm to prevent damage to the calcaneal bone 7,13,19,22-23. The puncture site will be according to Blumenfeld's scheme, which is presented in Figure 2.

Source: Own-development
NOTE: The areas for heel capillary puncture are lateral edges, represented by (a) and (b). To define them, two vertical imaginary lines are drawn from references indicated with arrows, until reaching their projection to the heel 4,19.
Figure 2 Schematic representation of Blumenfeld's technique.
Among the warnings for capillary puncture of the heel are insufficient perfusion in the area, regardless of the cause; vascular compromise of the limbs, previous puncture, infection or local trauma and epidermal lesions in puncture areas 19,24.
Considerations to be taken into account in heel capillary puncture
Analgesia: Acute pain is defined as the unpleasant sensory and emotional experience associated to current or potential tissue damage 25. Capillary heel prick is an invasive procedure that produces acute pain in the NB, therefore, effective, low cost and free of undesirable side effects analgesic interventions, whether pharmacological or non-pharmacological are necessary. Non-pharmacological interventions consist of measures that induce well-being and comfort, such as restraint, breastfeeding at least five minutes prior to the procedure, attributing its analgesic effect to the product of restraint, skin-to-skin contact, sweet taste of breast milk, as well as hormonal induction (oxytocin). Another intervention is the kangaroo method, “skin to skin” 30 minutes prior to the puncture. The administration of drops of 25 and 30% glucose solution orally two minutes prior to the procedure is among the pharmacological interventions, whose effect is associated to the stimulation of the release of endogenous opioid neurotransmitters such as beta-endorphins 4,26-30. Moreover, an additive analgesic effect can be achieved when combined with another intervention.
Material and equipment: Sterile automatic lancet and filter paper specific for neonatal metabolic screening, data sheet, 70% alcohol or alcohol swabs, dry cotton swabs, adhesive band or gauze and sterile gloves. Currently, the data sheet has integrated filter paper for blood sample collection. If necessary, 25 or 30% glucose solution and dropper. In addition, material and equipment for hand washing, rigid container for biohazardous biological infectious waste (BBIW) and personal protective equipment (mask, goggles and/or mask) are required.
Samples care
Drying and sample position: The sample is protected from contamination and allowed to dry on filter paper for two to four hours at room temperature. Direct heat sources should not be used, or it should be dried by other methods. It is recommended to place it in a horizontal position on a support that facilitates uniform and safe drying 13,19.
Preservation and delivery: The dried blood sample on the filter paper and data sheet is placed in a paper or plastic envelope with a desiccant and stored until it is sent to the laboratory for analysis. The dried sample remains stable for 7 days at a temperature ranging from 20 to 25°C, while at 2 to 8°C stability is increased for 30 days 13,19. The conditions for stability shall be maintained during shipment. For temporary storage and dispatch of the sample, administrative controls are performed according to the institutional protocol.
Factors that affect the results of neonatal metabolic screening: They are related to (a) obtaining the sample, (b) preservation and transport, and (c) pharmacological interference of drugs such as valproic acid, risperidone, cephalosporins, benzodiazepines, loop diuretics and metoclopramide, among others 16.
Since obtaining and depositing the blood sample on the filter paper represents the beginning of the preanalytical stage of the operative phase, and it has to be performed according to the set forth protocol 13,19, Figure 4 schematically shows an adequate sample, as well as variants of inadequate samples.
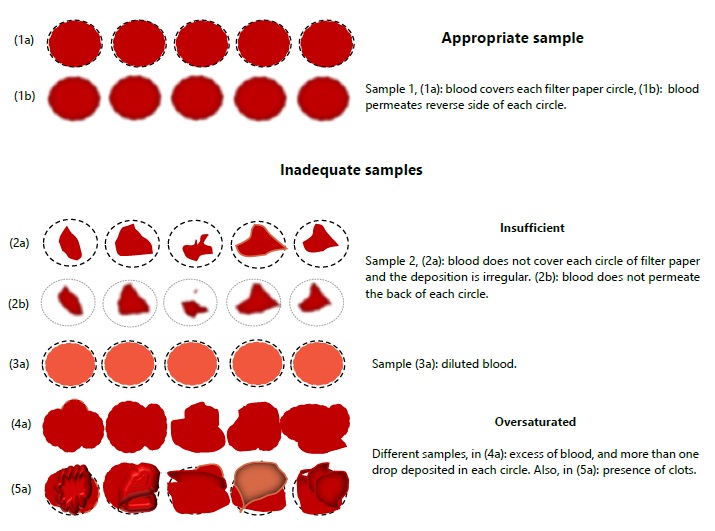
Source: Own-development.
Taken from Vela-Amieva, Ibarra-González, Fernández-Lainez, Belmónt-Martínez 19.
Figure 4 Schematic representation of capillary blood sample deposited on filter paper in an adequate form, and variants of inadequate samples. Where (a) and (b) represent the front and back side of the filter paper, respectively.
Discussion
This integrative review highlights that the neonatal metabolic screening program has emerged as a preventive medicine strategy for the benefit of children's health, both internationally and nationally. The early identification of newborns with suspected metabolic diseases and, based on this “suspicion”, a comprehensive assessment enables a confirmatory diagnosis and the initiation of timely treatment. Otherwise, a diagnosis could take years, and the disease could cause irreversible damage to the child's health, in addition to negative effects on family and social health, because the cost of the disease and associated disability is not limited to the economic aspect 9,13.
Worldwide, the most widely used method for obtaining blood samples continues to be capillary puncture of the newborn's heel, even though it has been proven to be more painful and traumatic than venipuncture 4,19. The permanence of this method may be related to the technical ease of puncture, an aspect that is independent of the quality of the sample obtained. Additionally, this procedure can be more socially acceptable.
There is variability in the results depending on the age in days of life of the newborn; it has been proven the convenience of performing this test between 24 and 48 hours of life of the NB in order to have a timely detection of abnormalities and prompt medical management 18. In addition, this time represents an opportunity to expand screening coverage by making it possible to perform the test before the newborn is discharged from the hospital.
In our country, this screening is performed on newborns between the third and fifth day of life, so that after hospital discharge it is necessary to go to the health unit to request it. Therefore, the relevance of this test should be disseminated from the prenatal consultation, and its understanding should be ensured before the mother is discharged from the hospital 9. To prevent delays or omissions in the participation of all NBs in the program, it is necessary to eliminate cultural, economic, geographic and health policy gaps; the existence of a legal framework for the obligatory nature of this public health strategy does not ensure its coverage 9-12.
Once the parents or guardians of the newborn are able to request the screening at the health institution, there is a risk of failure in the pre-analytical stage, which requires coordinated standardization of the process of collection, drying, storage and delivery conditions of the sample. In addition, humanized care is required during the NB care process. Therefore, it implies that the nursing professional performs evidence-based interventions to improve care, research, teaching and management practice, in collaboration with the multidisciplinary health team. In such a way that it contributes to the achievement of the main goal of the neonatal metabolic screening program, that is, infant health 30-36.
Conclusions
The review carried out allows highlighting that nursing intervention is a determining factor in the operation of the neonatal metabolic screening program. As they work at the first level of care, it is the nursing professional who participates in the promotion, dissemination, collection and care of the samples until they are taken to the analysis laboratory. Therefore, this review contributes to the development of competencies that allow interventions that respond to the care needs of the newborn who participates in this preventive medicine strategy. Thus, this available scientific evidence enables a safe praxis in this area of care. Nursing interventions in the pre-analytical stage should be risk-free, and ensure adequate blood samples for the practice of neonatal metabolic screening. One thought to consider is “an adequate sample can carry valuable information to save a child's life, as well as to prevent complications and disability.”
Referencias bibliográficas
1. Vicente E, Casas L, Ardanaz E. Origen de los programas de cribado neonatal y sus inicios en España. An Sist Sanit Navar [Internet]. 2017 [citado 15 feb 2021];40(1):131-140. Disponible en: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1137-66272017000100131 [ Links ]
2. Valera D, Montealegre AL, Bermúdez A, García R. Importancia de una propuesta para la implementación de un programa de tamizaje neonatal expandido en Colombia. Revista Med [Internet]. 2019 [citado 15 feb 2021];27(2):21-33. Disponible en: http://dx.doi.org/10.18359/rmed.4195 [ Links ]
3. Ibarra-González I, Fernández-Lainez C, Belmont-Martínez L, Guillén-López S, Monroy-Santoyo S, Vela-Amieva M. Caracterización de errores innatos del metabolismo intermediario en pacientes mexicanos. An Pediatr (Barc) [Internet]. 2014 [citado 17 feb 2021];80(5):310-316. Disponible en: http://dx.doi.org/10.1016/j.anpedi.2013.09.003 [ Links ]
4. Valero V. Venopunción versus punción en el talón para el cribado metabólico en recién nacidos. Metas de Enfermería [Internet]. 2014 [citado 20 feb 2021];17(10):24-27. Disponible en: Disponible en: https://www.enfermeria21.com/revistas/metas/articulo/80675/venopuncion-versus-puncion-en-el-talon-para-el-cribado-metabolico-en-recien-nacidos/ [ Links ]
5. Lise F, Machado A, Marten V, Schwartz E. Erros inatos do metabolismo do recém-nascido: Atualização de enfermagem. Revista Recien [Internet]. 2019 [citado 20 feb 2021];9(25):37-42. Disponible en: Disponible en: https://www.recien.com.br/index.php/Recien/article/view/278 [ Links ]
6. Delgado-Pecellín C, Álvarez AI, Bueno M, Jiménez MM, Quintana ME, Ruíz P, et al. Resultados del cribado neonatal de Andalucía Occidental tras una década de experiencia. Rev Esp Salud Pública [Internet]. 2020 [citado 25 feb 2021];94(16):e1-12. Disponible Disponible https://www.mscbs.gob.es/bibliopublic/publicaciones/recursos_propios/resp/revista_cdrom/vol94/o_breves/rs94c_202012174.pdf [ Links ]
7. González-Lamuño D, Couce ML. Cribado neonatal. Pediatr Integral [Internet]. 2019 [citado 25 feb 2021];XXIII(3):169.el-169.e10. Disponible en: Disponible en: https://www.pediatriaintegral.es/wp-content/uploads/2019/xxiii03/09/n3-169e1-10_Int-Esp_Glez.pdf [ Links ]
8. Cifuentes RA. Consideraciones bioéticas del tamizaje neonatal: pautas para su regulación integral. Rev Latinoam Bioet [Internet]. 2015 [citado 27 feb 2021];16(30-1):154-173. Disponible en: Disponible en: https://revistas.unimilitar.edu.co/index.php/rlbi/article/view/1445/1223 [ Links ]
9. Barba JR. Tamiz neonatal: Una estrategia en la medicina preventiva. Rev Mex Patol Clin [Internet]. 2004 [citado 27 feb 2021];51(3):130-44. Disponible: Disponible: https://www.medigraphic.com/pdfs/patol/pt-2004/pt043b.pdf [ Links ]
10. Repič B, Remec ŽI, Drole A, Žerjav M, Šmon A, Koračin V, et al. Expanded newborn screening program in Slovenia using tandem mass spectrometry and confirmatory next generation sequencing genetic testing. Zdr Varst [Internet]. 2020 [citado 07 mar 2021];59(4):256-63. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/33133282/ [ Links ]
11. Martínez AE, Cepeda AC. Tamiz neonatal en México. CienciAcierta [Internet]. 2018 [citado 07 mar 2021];(52):1-6. Disponible en: Disponible en: http://www.cienciacierta.uadec.mx/2018/03/25/tamiz-neonatal-en-mexico/ [ Links ]
12. García-Flores EP, Herrera-Maldonado N, Hinojosa-Trejo MA, Vergara-Vázquez M, Halley-Castillo ME. Avances y logros del programa de tamiz metabólico neonatal (2012-2018). Acta pediátr Méx [Internet]. 2018 [citado 12 mar 2021];39(6):57S-65S. Disponible en: http://dx.doi.org/10.18233/apm39no6pp57s-65s1722 [ Links ]
13. Centro Nacional de Equidad de Género y Salud Reproductiva. Tamiz neonatal detección, diagnóstico, tratamiento y seguimiento de los errores innatos del metabolismo. Lineamiento técnico. Secretaría de Salud [Internet]. México; 2010 [citado 12 mar 2021]. Disponible en: Disponible en: https://www.gob.mx/cms/uploads/attachment/file/13774/TN_E_Innatos_Metabolismo.pdf [ Links ]
14. Castiñeras DE, Couce M-L, Marin JL, González-Lamuño D, Rocha H. Situación actual del cribado neonatal de enfermedades metabólicas en España y en el mundo. Anales de Pediatría [Internet]. 2019 [citado 20 mar 2021];91(2):128.e1-128.e14. Disponible en: http://dx.doi.org/10.1016/j.anpedi.2019.05.007 [ Links ]
15. Loeber JG, Platis D, Zetterström RH, Almashanu S, Boemer F, Bonham JR, et al. Neonatal screening in Europe revisited: An ISNS perspective on the current state and developments since 2010. Int J Neonatal Screen [Internet]. 2021 [citado 20 mar 2021];7(1):1-21. Disponible en: http://dx.doi.org/10.3390/ijns7010015 [ Links ]
16. Cedillo B, Estrada R, Jonguitud V, Parra I. Factores que afectan algunas de las pruebas del tamiz neonatal. Medicina Universitaria [Internet]. 2007 [citado 27 mar 2021];9(34):36. Disponible en: Disponible en: https://www.medigraphic.com/pdfs/meduni/mu-2007/mu071b.pdf [ Links ]
17. Urrútia G, Bonfill X. Declaración PRISMA: una propuesta para mejorar la publicación de revisiones sistemáticas y metaanálisis. Med Clin (Barc) [Internet]. 2010 [citado 22 febrero 2022]; 135(11):507-511. Disponible en: Disponible en: https://es.cochrane.org/sites/es.cochrane.org/files/public/uploads/PRISMA_Spanish.pdf [ Links ]
18. Peng G, Tang Y, Cowan TM, Zhao H, Scharfe C. Timing of newborn blood collection alters metabolic disease screening performance. Front Pediatr [Internet]. 2020 [citado 27 mar 2021];8:623184. Disponible en: http://dx.doi.org/10.3389/fped.2020.623184 [ Links ]
19. Vela-Amieva M, Ibarra-González I, Fernández-Lainez C, Belmónt-Martínez L. Fundamentos teórico-prácticos para la toma correcta de la muestra de sangre del talón para el tamiz neonatal. Acta pediátr Méx [Internet]. 2014 [citado 07 abr 2021];33(6):273-278. Disponible: Disponible: https://www.medigraphic.com/pdfs/actpedmex/apm-2012/apm126b.pdf [ Links ]
20. Calle DG, Muñoz TV, Delgado CR, Vera RS. Tamizaje neonatal de hipotiroidismo congénito. RECIAMUC [Internet]. 2020 [citado 07 abr 2021];4(3):268-274. Disponible en: http://dx.doi.org/10.26820/reciamuc/4.(3).julio.2020.268-274 [ Links ]
21. West R, Hong Y, Derraik JG, Webster D, Heather NL, Hofman PL. Newborn screening TSH values less than 15 mIU/L are not associated with long-term hypothyroidism or cognitive impairment. J Clin Endocrinol Metab [Internet]. 2020 [citado 13 abr 2021];105(9):e3329-e3338. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32598474/ [ Links ]
22. Tugce T, Tugba E, Ozdemir H, Yahsi A, Fitoz S, Ciftci E, et al. Osteomielitis del calcáneo secundaria a la prueba de Guthrie. A propósito de un caso. Arch Argent Pediatr [Internet]. 2016 [citado 13 abr 2021];114(04):e260-e263. Disponible: http://dx.doi.org/10.5546/aap.2016.e260 [ Links ]
23. Jain A, Rutter N. Ultrasound study of heel to calcaneum depth in neonates. Arch Dis Child Fetal Neonatal Ed [Internet]. 1999 [citado 21 abr 2021];80(3):F243-F245. Disponible en: http://dx.doi.org/10.1136/fn.80.3.f243 [ Links ]
24. Chattás G, Egan F. Extracciones de sangre: Punción capilar de talón. Enfermería Neonatal [Internet]. 2007 [citado 21 abr 2021];1(3):24-27. Disponible en: Disponible en: https://www.fundasamin.org.ar/archivos/EXTRACCIONES%20DE%20SANGRE.pdf [ Links ]
25. Herdman TH, Kamitsuru S, Takáo C, editores. Diagnósticos enfermeros. Definiciones y clasificación 2021-2023. 12a ed. España: Elsevier; 2021. [ Links ]
26. Murillo de las Heras MM, Enríquez I, Martos IM. Lactancia materna y otros métodos no farmacológicos de alivio del dolor en el recién nacido. Paraninfo Digital [Internet]. 2018 [citado 03 may 2021];XII(28):1-3. Disponible en: Disponible en: http://www.index-f.com/para/n28/pdf/e097.pdf [ Links ]
27. Guzmán-Arteaga AN, Fajardo-Ochoa F, Ramírez-Rodríguez CA, Alvarez-Hernández G. Efecto analgésico de la solución glucosada al 25% vs crema EMLA. Evaluación por la escala de PIPP. Bol Clin Hosp Infant Edo Son [Internet]. 2013 [citado 03 may 2021];30(2):56-62. Disponible en: Disponible en: https://www.medigraphic.com/pdfs/bolclinhosinfson/bis-2013/bis132b.pdf [ Links ]
28. Committee on Fetus and Newborn and Section on Anesthesiology and Pain Medicine. Prevention and management of procedural pain in the neonate: an update. Pediatrics [Internet]. 2016 [citado 15 jun 2021];137(2):1-15. Disponible en: Disponible en: https://pediatrics.aappublications.org/content/pediatrics/137/2/e20154271.full.pdf [ Links ]
29. González CT, Fernández IM. Revisión bibliográfica en el manejo del dolor neonatal. ENE Revista de Enfermería [Internet]. 2012 [citado 13 may 2021];6(3):10. Disponible en: Disponible en: http://www.index-f.com/ene/6pdf/6304.pdf [ Links ]
30. Romero H, García CA, Galindo JP. Manejo del dolor en neonatos hospitalizados, revisión ampliada de la literatura. Repert. med. cir [Internet]. 2015 [citado 19 may 2021];24(3):182-93. Disponible en: Disponible en: https://www.fucsalud.edu.co/sites/default/files/2017-01/manejo%20del%20dolor%20en%20neonatos%20hospitalizados.pdf [ Links ]
31. Sánchez P, Cocho de Juan JA, Bóveda MD, Castiñeiras DE, Colón C, Iglesias AJ, et al. Evaluación y perspectiva de 20 años de cribado neonatal en Galicia. Resultados del programa. Rev Esp Salud Pública [Internet]. 2020 [citado 19 may 2021];94(16):e1-15. Disponible en: Disponible en: https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/vol94/c_especiales/rs94c_202012161.pdf [ Links ]
32. Molina B, Roberto W, Batistela G, Zanin G, Morales A, De Carvalho MC. Acceso precoz al tamizaje neonatal biológico: articulación entre accionas de programas de atención al niño. Rev Latino-Am Enfermagem [Internet]. 2020 [citado 25 may 2021];28:1-7. Disponible en: http://dx.doi.org/10.1590/1518-8345.2938.3266 [ Links ]
33. Nicolás P, Pàmpols T, García FJ, Arribas CM, Pérez A, García JM, et al. Medio siglo de cribado neonatal en España: evolución de los aspectos éticos, legales y sociales (AELS). Parte II, marco legal. Rev Esp Salud Pública [Internet]. 2021 [citado 25 may 2021];95(26):e1-14. Disponible en: Disponible en: https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/vol95/c_especiales/rs95c_202101018.pdf [ Links ]
34. Labrador M, Pàmpols T, Dulín E, Pérez A, García JM, Díaz A, et al. Medio siglo de cribado neonatal en España: evolución de los aspectos éticos, legales y sociales (AELS). parte III, aspectos sociales. Rev Esp Salud Pública [Internet]. 2021 [citado 29 may 2021];95(26): e1-17. Disponible en: Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=7957670 [ Links ]
35. González-Lamuño D, Bóveda MD, Bueno M, Gort L, Unceta M, Morales M. El cribado metabólico del recién nacido como modelo asistencial de la medicina de precisión. Perspectiva desde la asociación Española para el estudio de los errores congénitos del metabolismo (AECOM). Rev Esp Salud Pública [Internet]. 2021 [citado 02 jun 2021]; 95(26): e1-17. Disponible en: Disponible en: https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/vol95/originales/rs95c_202101021.pdf [ Links ]
36. Pàmpols T, Pérez A, García JM, Díaz A, Martín C, García FJ, et al. Medio siglo de cribado neonatal en España: evolución de los aspectos éticos, legales y sociales (AELS). Parte I, aspectos éticos. Rev Esp Salud Pública [Internet]. 2021 [citado 02 jun 2021];95(26):e1-22. Disponible en: Disponible en: https://www.mscbs.gob.es/bibliopublic/publicaciones/recursos_propios/resp/revista_cdrom/vol95/c_especiales/rs95c_202101008.pdf [ Links ]
37. Sharma P, Kumar P, Gupta S, Dhot PS, Sharma R, Mahapatra TK. Inborn error of metabolism [IEM] screening in neonates. Pravara Med Rev [Internet]. 2018 [citado 06 jun 2021];10(3):24-28. Disponible en: Disponible en: https://www.pravara.com/pmr/pmr-10-4-6.pdf [ Links ]
Received: July 15, 2021; Accepted: June 24, 2022











 texto em
texto em 




