Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Sanus
versão On-line ISSN 2448-6094
Sanus vol.7 Sonora Jan./Dez. 2022 Epub 21-Mar-2023
https://doi.org/10.36789/revsanus.vi1.292
Review
Systematic review of interventions for diabetic foot prevention in older diabetic adults
1Universidad Autónoma de Coahuila. Facultad de Enfermería. Saltillo, Coahuila, México.
2Profesor de Tiempo Completo. Facultad de Enfermería. Universidad Autónoma de Nuevo León, Monterrey, México.
Introduction:
The diabetic foot is one of the major complications of diabetes; alterations such as peripheral arterial disease and diabetic neuropathy, which initially manifest with foot injuries, which can progress to ulcers and even amputations and cause mobility and independence limitations in older adults. There are different types of interventions to prevent diabetic foot. Nevertheless, for a researcher, before developing an intervention to prevent diabetic foot in older adults, it is essential to review their quality criteria.
Objective:
Explore the characteristics of the most effective health interventions for diabetic foot prevention in diabetic older adults.
Methodology:
Systematic review, following the guidelines of “Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols” to prepare the report. The 8.5b risk of bias tool of Cochrane manual was used in order to assess study quality criteria. The sample was nine of 415 studies (1995-2017) from the Scopus, PubMed and Web of Science databases.
Results:
Foot care education with the support of materials was the most used and evaluated intervention strategy regarding the care behavior and neuropathy symptoms.
Conclusions:
The most effective interventions to prevent diabetic foot in diabetic older adults included foot care education and awareness, telephone follow-up, printed material, and foot care materials. According to quality criteria of the studies reviewed, it was not possible to determine which intervention is the best.
Keywords: Diabetes mellitus; Diabetic foot; Elderly; Systematic review (DeCS)
Introducción:
El pie diabético es una de las mayores complicaciones de la diabetes, alteraciones como enfermedad arterial periférica y neuropatía diabética, que en un inicio se manifiestan por lesiones en los pies pueden avanzar a úlceras hasta amputaciones y provocar limitaciones de movilidad e independencia de los adultos mayores. Existen diferentes tipos de intervenciones para prevenir pie diabético; sin embargo, para un investigador antes de desarrollar una intervención para prevenir pie diabético en adultos mayores es imprescindible revisar los criterios de calidad de éstas.
Objetivo:
Explorar las características de las intervenciones de salud más efectivas para la prevención de pie diabético en adultos mayores con diabetes.
Metodología:
Revisión sistemática, siguiendo las directrices de Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols para elaboración del reporte. Se utilizó la herramienta 8.5b riesgo de sesgo del manual Cochrane para valorar criterios de calidad de los estudios. La muestra fue nueve de 415 estudios (1995-2017) de bases de datos Scopus, PubMed y Web of Science.
Resultados:
Educación para el cuidado de los pies con apoyo de materiales fue la estrategia de intervención más utilizada y evaluada respecto al comportamiento del cuidado y síntomas de neuropatía.
Conclusiones:
Las intervenciones más efectivas para prevenir pie diabético en adultos mayores con diabetes incluyeron educación y conocimiento sobre cuidado de los pies; seguimiento telefónico, material impreso y materiales para el cuidado de los pies. De acuerdo con los criterios de calidad de los estudios revisados no fue posible determinar cuál es la mejor intervención.
Palabras clave: Diabetes mellitus; Pie diabético; Adulto mayor; Revisión sistemática (DeCS)
Introdução:
O pé diabético é uma das principais complicações do diabetes; alterações como doença arterial periférica e neuropatia diabética, que se manifestam inicialmente com lesões nos pés, que podem evoluir para úlceras e até amputações e causar limitações de mobilidade e independência em idosos. Existem diferentes tipos de intervenções para prevenir o pé diabético. No entanto, para um pesquisador, antes de desenvolver uma intervenção para prevenir o pé diabético em idosos, é fundamental revisar seus critérios de qualidade.
Objetivo:
Explorar as características das intervenções de saúde mais eficazes para a prevenção do pé diabético em idosos diabéticos.
Metodologia:
Revisão sistemática, seguindo as diretrizes de “Itens de relatório preferidos para revisão sistemática e protocolos de meta-análise” para preparar o relatório. A ferramenta de risco de viés 8.5b do manual Cochrane foi usada para avaliar os critérios de qualidade do estudo. A amostra foi de nove de 415 estudos (1995-2017) das bases de dados Scopus, PubMed e Web of Science.
Resultados:
A educação para o cuidado com os pés com apoio de materiais foi a estratégia de intervenção mais utilizada e avaliada quanto ao comportamento de cuidado e sintomas de neuropatia.
Conclusões:
As intervenções mais eficazes para prevenir o pé diabético em idosos diabéticos incluíram educação e conscientização sobre cuidados com os pés, acompanhamento por telefone, material impresso e materiais para cuidados com os pés. De acordo com os critérios de qualidade dos estudos revisados, não foi possível determinar qual intervenção é a melhor.
Palavras-chave: Diabetes insípido; Pé diabético; Adulto Idoso; Revisão Sistemática (DeCS)
Introduction
Diabetes mellitus 2 (DM) is one of the main causes of hospitalization in adults 1. With the increase in life expectancy, older adults (OA) with DM are a population group that is growing in developing countries; such is the case of those belonging to the Latin American (LA) region 2. Foot ulcers are among the major complications of DM, a complication that can lead OA to be more prone to mobility disability because of a non-traumatic lower limb amputation 3. DM is the cause of 70% of lower limb amputations, positioning it as one of the main causes of disability in the LA region 1, which implies depending on other people for activities of daily living thereby losing independence.
Periodic feet evaluation for neuropathy signs detection, circulation disorders and skin alterations in people with DM is a basic principle of comprehensive care for preventing diabetic foot (DF) 4, in addition to good management of early symptoms or manifestations, which presupposes education, hygiene and foot and disease care (e.g. diet, exercise, adherence to treatment, glycemic control) 5,6.
Therefore, a systematic review on health interventions can provide valuable information on activities applied or included and their results in OA with DM in order to guide an intervention program in this population. This is because systematic reviews found address population groups of 18 years of age and over and are not specific to OA 7,8.
Therefore, a knowledge gap was detected regarding the best health interventions in OA to prevent DF. This becomes relevant for primary care nursing staff, considering that OA are a vulnerable group, with functional decline and limited access to health services. Consequently, OA have a higher risk of complications from DM, including DF, which can affect the OA’s life quality, mobility, economy, and family and social care. Therefore, the purpose of this review was to explore the characteristics of the most effective health interventions for the prevention of diabetic foot in OA with DM.
Methodology
Systematic review, structuring a clinical question with the PICO format: Population (P), Interventions (I), Control (C [referring to the group]), Outcome (O). Being structured as: P: OA with DM, I: Most effective health interventions [randomized controlled studies], C: Intervention and comparison group, O: Prevention of DF. It was developed based on the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) criteria 9.
The quality of the studies was evaluated with the risk of bias criterion with the 8.5b risk of bias tool described by the Cochrane manual, Spanish version 10. The quality criteria assessed were selection, performance, detection, attrition and notification biases. These in turn are rated as high, medium or low quality.
Types of articles reviewed: Because only one randomized controlled trial (RCT) was located, the review was extended to evaluation programs and/or quasi-experiments. The interventions were classified into simple and complex. Simple interventions were those focused only on education compared to usual care (what the person is used to). Complex interventions included a comprehensive care approach (other care alternatives, in addition to what the person is used to) or those that combine education and comprehensive care, compared with standard care.
Selection criteria: Full-text articles, in English or Spanish, regarding intervention on foot care or prevention of DF in OA with DM or at least with a mean age of 60 or more years were included. The year of publication was not restricted. Articles whose interventions were aimed at healing DF or active ulcers, amputations, or drug experimentation, systematic reviews, meta-analyses, and book chapters were excluded.
The search for interventions was carried out from August 2019 to January 2020 in the Pub Med, Scopus, Web of Sciences Core Collection (KCL-Korean Journal Database, Russian Science Citation Index, Scielo Citation Index) databases.
The search terms used in English were elder, aging, ageing, older, later life, type 2 diabetes, glucose intolerance, diabetic foot, diabetic feet, foot diseases, foot problem, foot disease, foot ulcer, diabetic foot ulcer, diabetic foot infection, prevent, foot care, foot monitoring, clinical trial, clinical trial phase I, II, III and IV, controlled clinical trial, multicenter stud, randomized controlled trial, early termination of clinical trials, double-blind method, randomized, randomized, trial, trials, single, double, doubled, triple, tripled, treble, trebled, blind, mask, “4 arm”, “four arm”, evaluation studies, program evaluation, validation studies, pre, post, pretest, posttest, program, evaluat, effectiveness, intervention, noncontrolled studies, noncontrolled clinical trial, nonrandomized controlled trial, non-randomized controlled studies, quasi experiments, quasiexperiments, non-randomized, non-randomised.
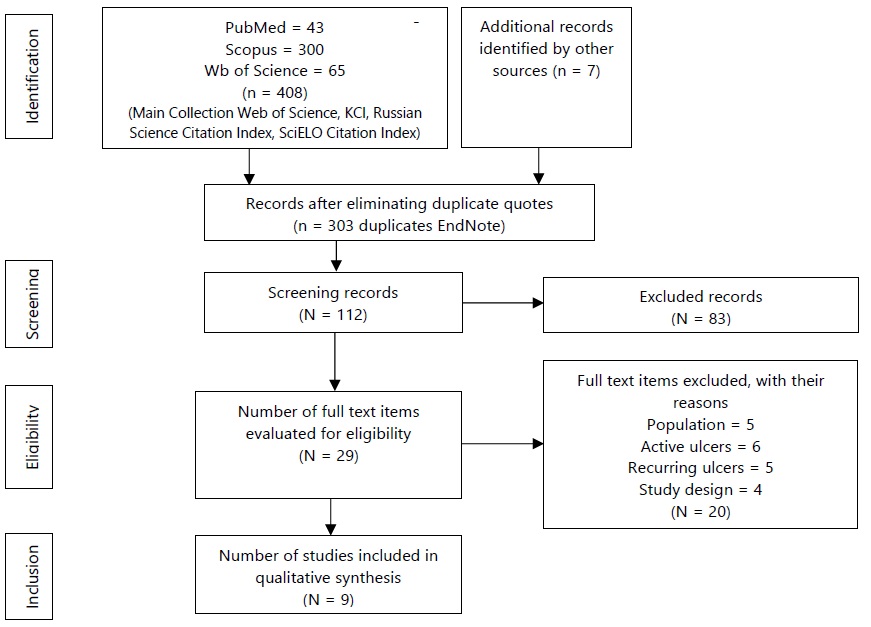
The Boolean operators AND and OR were used to perform all possible combinations, increase specificity and reduce search sensitivity. The End NoteTM bibliographic manager was used to merge retrieved titles, remove duplicates, and screen titles and abstracts. The selection was carried out in three stages: in the first, the title and abstract were reviewed, during the second, the reading and analysis of full text, and in the third, the evaluation of quality of the selected studies. Once the database search strategies were established, 408 articles were retrieved, in addition to seven that were previously available, which gave a total of 415. The principal investigator extracted the studies according to the eligibility criteria for in-depth review, using the files for critical reading (FLC 2.0) of clinical trials. When evaluating the articles by title and abstract, those that did not meet the inclusion criteria were removed. Subsequently, twenty-nine articles were reviewed in full text to obtain the final sample of nine articles. From the nine articles selected, the following was obtained: characteristics of the study (randomized controlled study [RCS], evaluation program or quasi-experiment), characteristics of the population (age and time of DM), intervention period (time, number of sessions), and type of intervention (delivery to the intervention group and delivery to the control group), (Figure 1). The results were divided into primary and secondary results. As primary outcome, the following was considered: existing or non-existing development of skills and/or foot care (washing, moisturizing, monitoring). The secondary outcome comprised the percentage that included the lack of formation of foot ulcers at the end of the intervention and during the follow-up.
Results
From the nine articles selected 66.7% of the studies were quasi-experiments without a control group 13-18, 22.2% RCTs 11,12, and 11.1% evaluation programs 19. 88.9% reported complex interventions 12-18 and 11.1% simple interventions 19. The age of the participants ranged between 63.9 and 76.0 years. Most were female. The duration of DM reported in 55.6% of the studies ranged from 4.8 to 13 years 12,13,15,16,18. Regarding primary results, 77.8% showed improvement in glycated hemoglobin (HbA1c) 11-13,15-18. In 77.8% of the studies, improvement in foot care (monitoring of sensitivity, hygiene and moisturizing) was seen, which is the main data for DF prevention 11,12,14-18. Regarding secondary results, only 11.1% 12 presented data that meant that there were no foot ulceration. The rest did not provide data in this area 11,13-19, (Table 1).
Table 1 Characteristics of selected studies, (2019-2020) (n=9).
Authors |
Methodology |
Results |
Evaluation times |
|||||||
Design |
Age |
Time DM |
Sample |
Instruments and measurements |
Primary |
Secondary |
||||
GI |
GC |
|||||||||
Ahn, et al. (2012)13 |
Quasi-experiment Non-randomized pre test-post test |
65 years |
12 to 13 years |
20 |
19 |
Fasting glycemia, HbA1c, Sensitivity, Total TSS for neuropathy symptoms, Balance, quality of life (SF-36v2) |
HbA1c:=3.11,p=0.004 (≠x GI 0.43±.57, GC -0.30±.87) Sensitivity: t=0.63,p=0.535 (≠x GI -0.05±.22, GC -0.10±.31) TSS: t=2.09,p=0.042 (≠x GI 0.21±1.44, GC -1.64±3.61) |
No data |
T1: Pre-intervention T2: 12 weeks post- Intervention |
|
|
Boyle, et al. (2013) 19 (USA) |
Multiple stages evaluation program (4 phases) aimed at health personnel. Evaluations carried out in patients with DM. |
>75 years (86% sample) |
No data |
19 |
No |
HbA1c, DEP on OA, OA reference of OA to specialists |
HbA1c: (p = .948), DEP: 43% (n = 35) to 60% (n = 40), p> 0.05, OA reference to specialists for feet anomalies: 50% to 80%, p> 0.05 |
No data |
T1: Basal T2: 3 months post intervention T3: 5 months post intervention |
|
Caruso, et al. (2007) 14 |
Quasi- Experiment without GC group control |
76 ± 8.6 years |
No data |
283 |
No |
Hba1c, foot skin exam, sensitivity with monofilament |
HbA1c: average of 7.9% vs. 7.3%, p = 0.004 Foot exam: 26% (44) vs. 57% (65), p˂0.001 |
No data |
T1: Pre-Intervention (12 months) T2: 9 months post- Intervention T3: 18 months post-intervention T4: 27 months post-intervention. |
|
Chen, et al. (2011) 15 |
Pretest-Postest Quasi-Experiment with a single group random selection |
68.89 ±9.53 years |
8.17 ±6.3 years |
323 |
HbA1c, IMC, CC, MNSI 0-10, ITB, Ability to self-care of feet |
HbA1c: t=1.31, p=0.191 CC: t= 4.22, p<0.01 MNSI: t=3.13, p<0.01 ITB right.: t=-3.14, p >0.001 ITB left: t=-1.75, p=>0.001 Feet care: 32.32 points (DE=6.76) vs 36.22 points (DE=6.95), t= -9.64, p˂0.001 |
No data |
T1: Pre-intervention T2: 10 to 12 months post- Intervention |
||
Cohen, et al. (2011) 11 |
ECA |
GI: 69.8 ± 1.07 years GC: 67.2 ± 9.4 years |
No data |
50 |
49 |
HbA1c, total cholesterol and triglycerides, SF-36, VR-36, DM self-care activities questionnaire ([TooBert] feet care), adherence to treatment |
HbA1c: GI X=-0.41, p<0.001, vs GC X=-0.20, p>0.001) Feet care: GI 1.46 days (IC= 0.75 to 2.18, p˂0.05) vs. GC 0.47 days (IC=-0.16 a 1.09, p>0.05) F=48.10, p<0.001 |
No data |
T1: Pre-intervention T2: 6 months post- Intervention |
|
Fu, et al. (2014) 16 |
Quasi-Experimental of a single group with repeated measurements 70.0 ± 7.46 Years |
8.8 ± 7.8 years |
29 |
No |
DKQ-24, DM self-care activities questionnaire ([Toobert] feet care) BMI, CC, blood glucose (fasting 8 hours) |
DKQ-24: F=37.78, p<0.005 Feet care: F=48.10, p<0.005 IMC: F=0.07, p>0.005 CC: F=1.28, p>0.005 Glucose: F=4.74, p<0.00 No data |
No data |
T1: Pre-intervention T2: 1.5 months post- Intervention T3: 2.5 months post- Intervention |
||
Pieber, et al. (1995) 17 |
Controlled test |
GI: 63.9 ± 8.2 years GC: 65.4 ± 6.1 years |
No data |
45 |
49 |
HbA1c, IMC, podiatry evaluation, DM knowledge and self -care. |
HbA1c: GI: 8.11 ± 1.55 vs. GC: 9.03 ± 1.79, averages difference -0.92 (IC=0.23 to 1.61, p<0.01). IMC: GI: 29.2 ±4.50 vs. GC: 30.3 ± 4.90), averages difference -1.08 (IC=0.28 to 1.86, p<0.01). Feet: Calluses GI 78% (35) to 49% (22), p <0.001 Interdigital fissures GI 55% (26) to 49% (22), p <0.001 |
No data |
T1: Pre-intervention T2: 6 months post- Intervention |
|
Sharoni, et al. (2017) 18 |
Cuasi-experimental pretest y postest |
68.52 ± 4.23 years |
12 ± 12.95 years |
31 |
No |
Feasibility and acceptability. DFSBS, FCCS, quality of life against neuropathy and foot ulcers. Podiatry assessment |
Feasibility (100% recruitment and retention). Moderately high acceptability, X=33.8, DE=4.08, DFSBS Z=-4.86, p<.001, FCCSZ=-4.76, p<0.001, Improvement in feet hygiene p <0.05, Anhydrosis decreased p <0.05 |
No data |
T1: Pre-intervention T2: 3 months post- Intervention |
|
Lavery, et al. (2007) 12 |
ECA simple blind |
GI1: 65.4 years GI2: 64.2 years GC: 65.0 years |
GI1: 13.7 ± 10.3 years GI2: 12.7 ± 9.7 years GC: 13.8 years (DE=11.5) |
G1: 59 G2: 56 |
58 |
Ulceration Risk (IWGDF): Neuropathy (SW 10 mg monofilament sensitivity and vibration), ITB (palpation and doppler), feet ulceration history, bone deformity. |
GI2: Decrease in ulceration risk: OR=4.48, 95%, IC 1.53–13.14) |
GC: 61% no ulceration GI1: 70% no ulceration GI2: 92% no ulceration |
T1: Pre-intervention T2: 15 months post- Intervention |
|
Source: Own-development.
nGI= 915, ngc=175, OA: Older Adult, IG: Intervention Group, CG: Control Group, DM: Diabetes Mellitus, HbA1c: Glycosylated Hemoglobin, BMI: Body Mass Index, WC: Waist Circumference, ABI: Ankle Arm Index, PPA= Podiatry Performance Assessments, MNSI= Peripheral Neurological Examination, TSS= Total for Neuropathy Symptoms, SF-36, VR-36= Veterans Life Quality, DKQ-24= DM Knowledge Questionnaire, DFSBS= Behaviors of foot care, FCCS= Foot Care Confidence Scale, IWGDF= International World Group of Diabetic Foot.
The duration of the interventions ranged from 1 to 15 months; the number of sessions ranged from 2 to 60; and the follow-up time ranged from 2.5 to 39 months (3.3 years average). Education prevailed in all the studies 11-19, additionally, 11.1% placed educational posters in offices where they attended the participants 14. 55.6% provided foot care kit 11-14,18, 11.1% combined education with Tai Chi 13. Another (11.1%) delivered the intervention through telephone sessions 15. There were those who incorporated the measurement of foot temperature with an infrared thermometer (11.1%) 12. Another study considered the participation of family members during the intervention (11.1%) 16. There were those (11.1%) who delivered the intervention through a multidisciplinary team and incorporation of the second hour session dedicated to pharmacotherapy 11. 88.9% of the studies, the facilitators were nurses 11-15,16-18, followed by DM educators in 44.4% 11,14,15,19, (Table 2).
Table 2 Synthesis of the intervention elements and selected studies quality of the evidence, 2019-2020). (n=9).
Authors |
Intervention Characteristics |
Activities |
Evidence quality |
|||||
Time (min) |
Frequency (weekly) |
Duration (months) |
Facilitator |
Intervention context |
GI |
GC |
||
|
Ahn, et al. (2012) |
60 |
2 |
3 |
Nurses |
Clinic sessions. Continuation with home exercises. |
60 minutes Tai-Chi in stages. Capillary glycemia evaluation. Motivation to continue with home exercises. T-shirts, music. |
60 minutes Tai-Chi |
Medium |
Boyle, et al. (2013) (USA) |
Stage 2: 120 Stage 3: 0 Stage 4: 0 |
Stage 2: 1 Stage 3: 0 Stage 4: 0 |
Stage 2: 0.25 Stage 3: 5 Stage 4: 3 and 5 |
Master training expert on DM |
Stage 2: Health center. Stage 3: Webinar Stage 4: 3 and 5 months, assessment of OA residents of institutions |
Stage 2: Face -to -face session to doctors, nurses, pharmacists and Cooks of OA residences. Stage 3: Reports evaluation and delivery Stage 4: OA residences assessment where trained personal work. |
There are not |
Medium |
Caruso, et al. (2007) |
Stage 1: Stage 2: Stage 3: |
Stage 1:4 |
Stage 1: 9 Stage 2: 9 Stage 3: 9 |
Nurse, medical assistant. DM Educator |
Stage 1 and 2: During consultations at health centers. Stage 3: Telephone calls to those who did not have podiatric evaluations. Continuation of activities E1 and E2. |
Stage 1: Bulletins in the waiting room on self-management of DM. Posters in offices reminding to remove shoes for podiatric evaluation Stage 2: Patients received informative folders on DM self-management. Podiatric assessment protocol in consultations. |
There are not |
Good |
Chen, et al. (2011) |
Phone calls 15 to 30 |
12 |
12 nurses (3 DM educators and 9 public health specialists) previously trained. |
Education in community health centers. Personalized phone calls (one year later). |
Sessions included diet control, medication, foot care, physical activity, movement |
There are not |
Medium |
|
Cohen, et al (2011) |
E1: 120 E2: 90 |
4 |
5 |
DM educators, nutritionists, nurses, pharmacists. |
Meeting room (4 to 6 people). Family members joined. |
E1: 1 hour educational components. 1 hour adherence to treatment E2: Needs of the group |
No activity |
|
Fu, et al. (2014) |
60 |
1 |
1.5 |
Community nurse |
Sessions in a room of 4 to 5 participants. Family members joined. |
Sessions on basic knowledge of DM, diet, physical activity, self-monitoring of glucose and foot care, adherence to pharmacological treatment. |
There was not |
|
Pieber, et al. (1995) |
90-120 minutes |
1 |
1 |
Health personnel |
Groups of 4 to 8 patients in the room. |
Information on DM, glucose self-monitoring practice, diet, exercise, foot care. |
Traditional care |
|
Sharoni, et al. (2017) |
Nurses |
Power point presentations, posters. Classroom session with 10 to 11 participants. |
Sessions: foot self-care, diabetic foot risk factors, prevention of complications, foot self-monitoring, daily foot hygiene, foot protection. They handed out a foot care kit, nursing checklists. |
There was not |
Good |
|||
Lavery, et al. (2007) |
No data |
G1: 1 time every 8 weeks G2: twice a day |
15 |
Nurses, doctors |
Group sessions and monitoring at home. G3: I/ He/ She consulted nurses about doubts and detection of anomalies during the intervention. |
G2: Standard therapy and structured foot assessment training. Received self-inspection log and mirror G3: Standard therapy and trained to use digital infrared thermometer. Received self-inspection logbook and infrared light thermometer |
G1: Podiatric assessment, practical educational sessions on self-care and foot complications. Participants received a pedometer. |
Good |
Source: own-development.
AM: Older Adult, IG: Intervention Group, CG: Control Group, G: Group, E: Stage, G1: Group 1, G2: Group 2, G3: Group 3.
Evidence quality: Regarding evidence quality, 44.4% of the studies showed high evidence quality 12,14,17-18. In these, the risk assessment was classified between low bias risk and unclear bias risk. The rest (55.6%) were classified as medium quality 11,13,15-16,19, because in some of the evaluated criteria they presented a high bias risk (Figure 2).
Discussion
In view to the objective of this systematic review, which was to explore the characteristics of the most effective health interventions for the prevention of DF in OA with DM, the following was found: most interventions focused on education about foot care and only one included improvement in the risk of DF (foot cracks, calluses and neuropathy symptoms). This reflects that education and knowledge of foot care (hygiene, moisturizing, monitoring, rest) is critical in prevention of DF, especially in people with neuropathy or loss of feeling in the feet 20.
Almost all interventions used educational sessions on foot care and/or delivery of care kits. More than half showed that participants increased foot care. Therefore, hygiene and moisturizing of the feet reduce injuries due to dry skin and daily feet monitoring warns about changes and injuries (color and temperature of the skin, cracks, among others) 21,22. However, the studies do not report a reduction in the injuries.
Education on foot care in patients with DM was reported to be effective both in the delivery of written informative material 12-14,18 and face-to-face sessions 11-13,15-19 or both combined 12,13,18. Both modalities involved feedback in person or by telephone, respectively. It seems that both informative material and face-to-face orientation and demonstration accompanied by feedback help participants to carry out more frequent foot care 23. Perhaps written material constitutes a guide that the participant can review or consult at any moment and as many times as required. Educational sessions offer the participant the opportunity to see procedures and raise concerns. This may be due to the fact that educational materials are an instrument to guide learning through education 23.
Additionally, just over half of the studies 11-14,18 provided foot care kits as a strategy that facilitated the process of improving foot care. This is certainly relevant for low-income or older patients who have difficulty obtaining accessories for their foot care, in addition to preventing excuses for not doing so. However, the studies that delivered kits, except for one of them 12 indicated that it served as a motivator for foot monitoring, the rest did not indicate advantages of such delivery.
Regarding the primary outcomes, almost all studies observed improvement in HbA1c results 11-13,15-18, critical results in foot irrigation and feeling, which in turn minimized the risk of DF. Hyperglycemia affects the function of the endothelium, which reduces the quality of the production of nitric oxide, which increases endothelial vasoconstriction that manifests in endothelial vascular disease. These lower limb injuries affect blood flow to the degree of hypoxia and damage the nerve fiber (diabetic neuropathy) manifested by altered sensitivity to vibrations, temperature and pain 25.
The number of sessions, intervention period and follow-up time varied among the studies. The longest intervention and follow-up corresponded to ECA (by its acronym in Spanish). Most of the studies were quasi-experimental, as they did not have randomization or a control group, so they were evaluated as studies with medium bias risk.
Only one study 16 considered the participation of family members in the intervention sessions; the incorporation of family members on health care and education interventions allows having positive progress of family members with chronic diseases tackling the disease, in addition to form support networks 24.
It was not possible to make a decision regarding the best intervention to prevent DF, due to the medium quality of the selected studies. However, elements for the development of a DF prevention intervention program were identified, which included: an intervention period of at least two months of education on foot care with the inclusion of a family caregiver, delivery of materials or kits to facilitate the foot care and assessment of health conditions such as control for HbA1c, presence of sensory neuropathy, peripheral arterial disease and foot status.
Conclusions
When exploring the characteristics of the most effective health interventions for the prevention of the DF in OA with DM, it can be concluded that interventions reviewed as most effective were those that included education and knowledge about the feet care, follow-up telephone calls, printed material and materials (kits) for feet care. HbA1c was the most used physiological indicator to determine glycemic control. The DF risk level was measured in one of the studies only. As well as the incorporation of the caregiver or relatives in the intervention. Evidence quality according to bias risk was medium so it was not possible to determine which intervention was the best to prevent diabetic foot.
Financing
Resources of program for professional development (PRODEP) 2019. “Fund aimed at promoting development of science and technology in the state of Coahuila” (FONCYT) with COAH-2020-C14-C087 registration number.
REFERENCES
1. Bello-Chavolla OY, Aguilar-Salinas CA. Diabetes in Latin America. En: Sam Dagogo, editor. Diabetes mellitus in developing countries and underserved communities. Suiza: Springer International Publising: 2017. p. 101-126. Disponible en: https://link.springer.com/book/10.1007/978-3-319-41559-8 [ Links ]
2. Metha R, Del-Moral ME, Aguilar-Salinas CA. Epidemiología de la diabetes en el anciano. Rev Invest Clin [Internet]. 2010 [citado 18 ene 2020];62(4):305-311. Dispnible en: Dispnible en: https://www.medigraphic.com/pdfs/revincli/nn-2010/nn104e.pdf [ Links ]
3. Ishak NH, Mohd-Yusoff SS, Rahman RA, Kadir AA. Diabetes self-care and its associated factors among elderly in primary care. J Taibah Univ Med Sci [Internet]. 2017 [citado 20 ene 2020];12(6): 504-511. Disponible en: https://doi.org/10.1016/j.jtumed.2017.03.008 [ Links ]
4. Organización Mundial de la Salud. Informe Mundial sobre la Diabetes. Biblioteca de la OMS [Internet]. Suiza; 2016 [citado 03 ene 2020]. Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/254649/9789243562255-spa.pdf?sequence=1 [ Links ]
5. Federación Internacional de Diabetes. IDF Diabetes Atlas. fmdiabetes.org [Internet]. Reino Unido; 2017. [citado 02 ene 2020]. Disponible en: Disponible en: http://fmdiabetes.org/wp-content/uploads/2018/03/IDF-2017.pdf [ Links ]
6. Federación Internacional de Diabetes y Grupo Internacional de Trabajo para Pie Diabético. Time to Act. Los Druk & Design BV Naarden [Internet]. Netherlands; 2005 [citado 02 ene 2020]. Disponible en: Disponible en: https://d-foot.org/images/pdf/put-feet-first.pdf [ Links ]
7. Hoogeveen R, Dorresteijn J, Kriegsman D, Valk G. Complex interventions for preventing diabetic foot ulceration. Cochrane Database Syst Rev [Internet]. 2015 [citado 12 ene 2020];24(8). Disponible en: https://doi.org/10.1002/14651858.CD007610.pub3 [ Links ]
8. Van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev [Internet]. 2016 [citado 20 ene 2020];32(1). Disponible en: https://doi.org/10.1002/dmrr.2701 [ Links ]
9. Urrutia G, Bonfill X. Declaración PRISMA: una propuesta para mejorar la publicación de revisiones sistemáticas y metaanálisis. Med Clin [Internet]. 2010 [citado 12 feb 2020];135(11):507-511. Disponible en: Disponible en: https://www.elsevier.es/es-revista-medicina-clinica-2-articulo-declaracion-prisma-una-propuesta-mejorar-S0025775310001454 [ Links ]
10. Centro Cochrane Iberoamericano (traductores). Manual cochare de revisiones sistemáticas de intervenciones. es.cochrane.org [Internet]. Barcelona; 2012 [citado 03 ene 2020]. Disponible en: Disponible en: https://es.cochrane.org/sites/es.cochrane.org/files/public/uploads/manual_cochrane_510_web.pdf [ Links ]
11. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ [Internet]. 2011 [citado 07 ene 2020];37(6):801-812. Disponible en: https://doi.org/10.1177/0145721711423980 [ Links ]
12. Lavery LA, Higgins KR, Lancot DR, Constantinides GP, Zamorano RG, Athanasiou KA, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care [Internet]. 2007 [citado 03 ene 2020];30(1):14-20. Disponible en: https://doi.org/10.2337/dc06-1600 [ Links ]
13. Ahn S, Song R. Effects of tai chi exercise on glucose control, neuropathy scores, balance and quality of life in patients wity type 2 diabetes and neuropathu. J Altern Complement Med [Internet]. 2012 [citado 18 ene 2020];18(2):1172-1178. Disponible en: https://doi.org/10.1089/acm.2011.0690 [ Links ]
14. Caruso LB, Clough-Gorr KM, Silliman RA. Improving quality of care for urban older people with diabetes mellitus and cardiovascular disease. J Am Geriatric Soc [Internet]. 2007 [citado 07 ene 2020];55(10):1656-1662. Disponible en: https://doi.org/10.1111/j.1532-5415.2007.01320.x [ Links ]
15. Chen MY, Huang WC, Peng YS, Guo JS, Chen CP, Jong MC et al. Effectiveness of a health promotion programme for farmers and fishermen with type-2 diabetes in Taiwan. Adv Nurs [Internet]. 2011 [citado 05 ene 2020];67(9):2060-2067. Disponible en: https://doi.org/10.1111/j.1365-2648.2011.05678.x [ Links ]
16. Fu M, Hu J, Cai X. Effectiveness of a community-based diabetes self-management intervention for Chinese adults with type 2 diabetes: a pilot study. Int J Nurs Pract [Internet]. 2015 [citado 16 ene 2020];21(2):132-140. Disponible en: https://doi.org/10.1111/ijn.12373 [ Links ]
17. Pieber TR, Holler A, Siebenhofer A, Brunner GA; Semlitsch B, Zapotoczky H, et al. Evaluation of a structured teaching and treatment programme for type 2 diabetes in general practice in a rural area of Austria. Diabet Med [Internet]. 1995 [citado 05 ene 2020];12(4):349-354. Disponible en: https://doi.org/10.1111/j.1464-5461.1995.tb00491.x [ Links ]
18. Sharoni SK, Abdul RH, Minhat HS, Shariff GS, Azman OM. A self-efficacy education programme on foot self-care behavior among older patients with diabetes in a public long-term care institution, Malasya a Quasi-experimental pilot study. BMJ Open [Internet]. 2007 [citado 12 ene 2020];7(6):e014393. Disponible en http://dx.doi.org/10.1136/bmjopen-2016-014393 [ Links ]
19. Boyle PJ, O’Neil KW, Berry CA, Stowell SA, Miller SC. Improving diabetes care and patient outcomes in skilled-care communities: successes and lessons from a quality improvement initiative. J Am Med Dir Assoc [Internet]. 2013 [citado 07 ene 2020];14(5):340-344. Disponible en: https://doi.org/10.1016/j.jamda.2012.11.010 [ Links ]
20. International Diabetic Federation. IDF Clinical Practice Recommendations on the Diabetic Foot. [Internet]. Bélgica; 2017. [actualizada 03 jul 2018; citado 10 ene 2020]. Disponible en: Disponible en: https://www.idf.org/about-diabetes/54-our-activities/222-idf-clinical-practice-recommendations-on-the-diabetic-foot.html [ Links ]
21. American Diabetes Association. Microvascular complications and foot care: standards of medical care in diabetes-2020. Diabetes Care [Internet]. 2020 [citado 12 ene 2020];43(Suppl 1):S135-S151. Disponible en: https://doi.org/10.2337/dc20-s011 [ Links ]
22. Schaper NC, Van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev [Internet]. 2020 [citado 18 ene 2020];36(S1):e3266. Disponible en: https://doi.org/10.1002/dmrr.3266 [ Links ]
23. Institutional Repository of information sharing, Pan American Health Organization (IRIS-PAHO). Guía para el diseño, utilización y evaluación de materiales educativos de salud. Organización Panamericana de Salud [Internet]. Washington, D.C.; 1984 [actualizada 02 dic 2013; citado 15 ene 2020]. Disponible en: Disponible en: https://iris.paho.org/handle/10665.2/3285 [ Links ]
24. Mendinueta MD, Valderrama CZ, Trout GG, Paredes BM. Enfoque de enfermería en la atención primaria de diabetes y corazón como herramienta fundamental para la prevención, cuidado y promoción. Duazary [Internet]. 2017 [citado 11 ene 2020];14(1):79-90. Disponible en http://dx.doi.org/10.21676/2389783X.1738 [ Links ]
25. Diaz CL, Luna PD. Productos finales de glicación avanzada en la enfermedad cardiovascular como complicación de la diabetes. Rev Med Inv [Internet]. 2016 [citado 20 ene 2020];4(15):52-57. Disponible en http://dw.doi.org/10.1016/j.mei.2016.02.002 [ Links ]
Received: May 13, 2021; Accepted: January 04, 2022











 texto em
texto em