Introduction
Endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) is a therapeutic tool that allows for biliary drainage when conventional endoscopic retrograde cholangiopancreatography (ERCP) is technically or clinically unsuccessful; around 5.6% of patients present stent obstruction at long-term follow-up1. Here, we describe a novel technique to treat EUS-HGS obstruction.
Case report
A 63-year-old man, diagnosed with a Klatskin tumor in 2019, was initially treated with ERCP, with the placement of two uncovered self-expandable metal stents (UC-SEMS) to the left and right hepatic ducts. After a positive response to oncologic treatment, a biliodigestive derivation (Roux-en-Y surgery) was carried out. In March 2021, the patient presented tumor progression with acute cholangitis; hence, an EUS-HGS was performed with a SEMS (Giobor Stent Taewoong Medical, Seoul, Korea). In April 2022, the patient presented acute cholangitis; the treatment of choice was UC-SEMS biliary stent (70 mm × 10 mm Wall Flex Biliary RX Stent; Boston Scientific Corp) placement in the HGS. In December 2022, the patient reported a new episode of acute cholangitis2.
A therapeutic endoscopic re-intervention was done. An indirect canulation through the HGS stent approach was decided, and with a diagnostic gastroscope (190 Olympus Medical Systems, Tokyo, Japan), the HGS SEMS was identified. Lumen obstruction from abundant cellular debris was observed.
With a sphincterotome (TRUEtome 44; Boston Scientific Corp), the HGS stent was cannulated, and a 0.035 mm guidewire (Jagwire Revolution High-Performance Guidewire, Boston Scientific Corp) was advanced up to the left hepatic duct. (Fig. 1) The cholangiography showed stent dysfunction and dilatation of intrahepatic ducts.
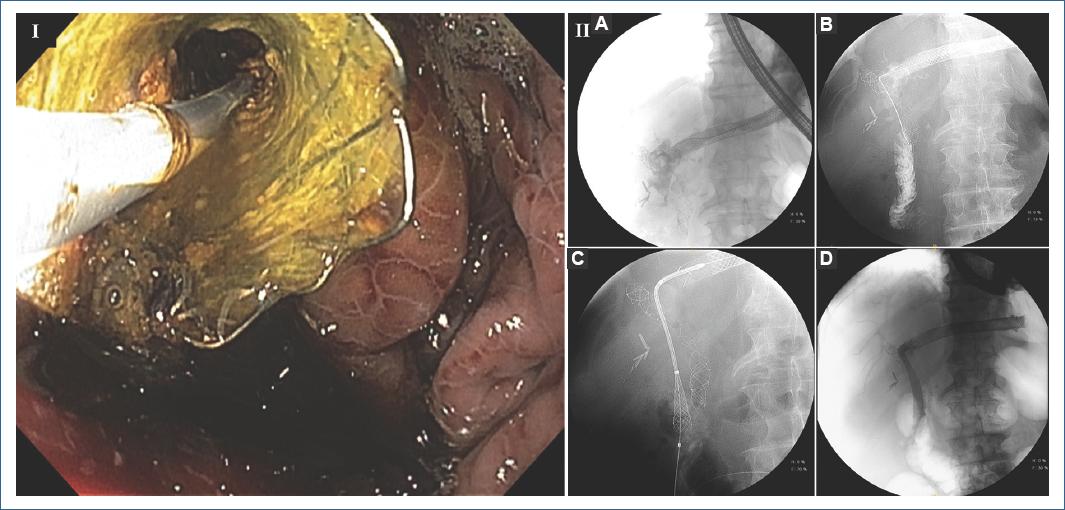
Figura 1 I. Selective cannulation of the hepaticogastrostomy with conventional sphincterotome. II. Cholangiogram. A: intrahepatic biliary dilatation with diffuse infiltration of cholangiocarcinoma. B: selective cannulation of the main left hepatic duct with the guidewire; contrast shows the hepaticojejunostomy. C: placement of the UC-SEMS from the hepaticogastrostomy to the hepaticojejunostomy. D: complete tract from the hepaticogastrostomy to the hepaticojejunostomy.
The guidewire was repositioned until it reached the hepaticojejunostomy (HJ). Then, an 8.5 × 10 Fr biliary dilatation catheter (Soehendra, Cook Medical, Winston Salem, NC, USA) was advanced until it reached the HJ. Later, an antegrade UC-SEMS biliary stent (80 mm × 10 mm WallFlex Biliary Stent, Boston Scientific Corp) was advanced from the HGS stent to the HJ. The patient improved clinically, with cholangitis resolution. No procedure-related adverse events were encountered.
Discussion
Patients with hepatobiliary malignancy have benefited from increased survival rates in recent years, due to new drug chemotherapies and indicated surgery in borderline resectable and locally advanced hepatobiliary cancer3.
With an increased survival rate, the probability of EUS-HGS obstruction and dysfunction increases over time because of an increased mucosal hyperplasia and biliary sludge that accumulates inside the stent4. Some studies have shown that stent length >3 cm has been associated with an increased patency time5, but very few studies have reported a concise technique to recover patency through the original stent.
A recent case report by Atalla et al.6 showed a similar technique to treat biliary malignant stenosis in a patient with modified anatomy, by introducing an anterograde stent through the puncturing of the left hepatic duct and placing a metal stent in the common bile duct.
The "through the mesh" technique, described by Minaga et al.7, is another example of unconventional intervention of an already obstructed stent. They reported that puncturing the mesh of a metal stent and then placing a guidewire in which they would later install another metal stent could be an alternative to treat this type of patients.
Argon plasma trimming is another recently described technique, in which patency is recovered through the coagulation of mucosal hyperplasia and sludge8.
Another described technique is the EUS-HGS dysfunction approach through direct visualization with a cholangioscope; this device allows a direct visualization of the stenosis zone and a more accurate maneuverability with the guidewire and sphincterotome9.
Conclusion
Although there is no gold standard for re-intervention of HGS stents, these techniques are promising to offer alternatives in the growing scenario of patients that with the new surgical and oncological treatments have been surpassed the survival rates and, in consequence, increased the probability of EUS-HGS dysfunction and the need of re-intervention.
The approach for patients with HGS dysfunction with an anterograde insertion of UC-SEMS is a technique that could be considered an additional treatment option.











 nueva página del texto (beta)
nueva página del texto (beta)


