Introduction
For patients with surgical alterations in the normal biliary anatomy (Whipple procedure), an endoscopic retrograde cholangiopancreatography (ERCP) is technically challenging1. The afferent limb syndrome (ALS) has been described in patients with biliodigestive derivative surgery, in which the afferent limb is unable to empty its contents due to a mechanical problem2. In patients with ALS, the access to the afferent limb depends on different types of reconstruction, the cannulation of the papilla is difficult due to the reversed orientation, and the performance of the therapeutic interventions often requires uncommon endoscopic accessories3 and the endoscopists skills to be successful. There is no gold standard for the endoscopic management of ALS, and alternative access points should be considered, like the rendezvous procedure (French for "encounter"), among others. We describe a successful case of ALS managed with a rendezvous and endoscopically stent placement.
A 73-year-old male was diagnosed with pancreatic adenocarcinoma and underwent a modified Whipple procedure (pylorus-preserving) 3 years earlier. Two months before the presentation, the patient developed intermittent jaundice, low-grade fever, and pain in the upper right quadrant of the abdomen. With respect to biochemical data, total bilirubin was 11.7 mg/dL (normal range 0.4-1.5 mg/dL), alkaline phosphatase was 800 IU/L (normal range 32-91 IU/L), and gamma-glutamyl transpeptidase was 550 IU/L (normal range 7-50 IU/L). An abdominal ultrasound reported dilatation of the biliary tree (common bile duct 8.5 mm in diameter). Ascending cholangitis secondary to an ALS was suspected and the patient underwent an emergency ERCP. Access to the biliary tree was impossible due to post-surgical alterations in anatomy.
Technique
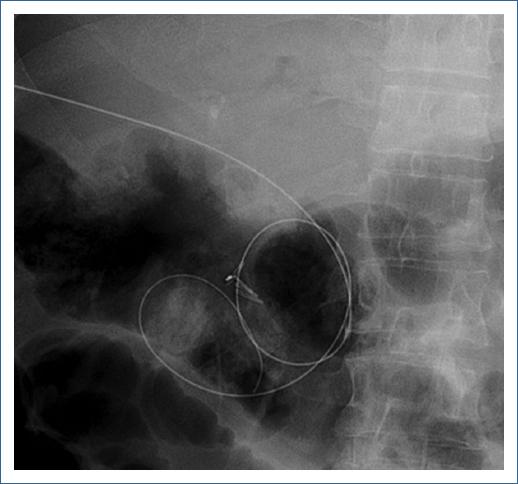
First, a colonoscope (190 Olympus Medical Systems, Tokyo Japan) was passed up to the choledochojejunostomy, which was found kinked and angulated. Therefore, the colonoscope was withdrawn and an enteroscope (EVIS EXERA II [SIF-Q180], Olympus Medical Systems, Tokyo Japan) was passed until the kinked choledochojejunostomy. Second, a hydrophilic Guidewire (0.035 mm Jagwire Revolution High Performance Guidewire, Boston Scientific Corp) was introduced percutaneously into the biliary tree under transabdominal ultrasound assistance to access the afferent limb (Fig. 1), and the guidewire was recovered with the enteroscope (Fig. 2). Third, the enteroscope holding the guidewire was withdrawn and interchanged into a stent-loaded colonoscope. Finally, the colonoscope holding the guidewire was introduced and an enteral uncovered self-expandable metal WallFlex Duodenal Stent, Boston Scientific Corp (22 mm × 60 mm) was successfully deployed at the site of the obstruction (Fig. 3). The schematic representation of the technique is described in figure 4. The patients evolution was satisfactory and was discharged 48 h after the procedure.

Figura 2 A: endoscopic view of the hydrophilic guidewire (asterix) emerging through the kinked choledochojejunostomy. B: hydrophilic guidewire retrieved with the endoscope.
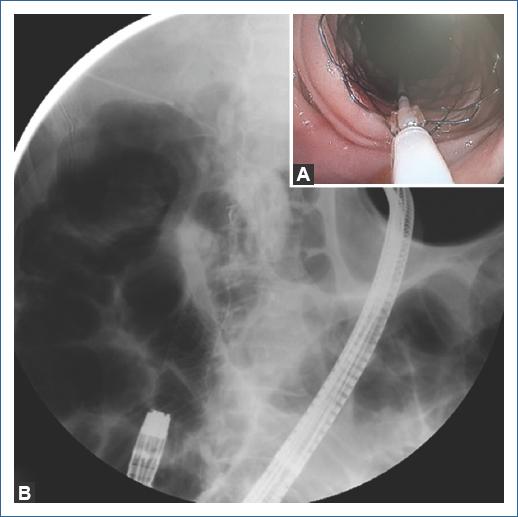
Figura 3 A: endoscopic deployment of enteral metallic stent with a colonoscope. B: enteral stent in correct position.
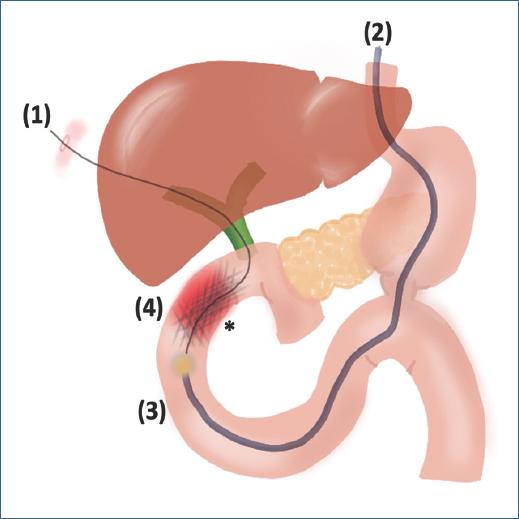
Figura 4 Schematic representation of the rendezvous technique and endoscopically stent placement. (1) A hydrophilic guidewire is inserted percutaneously through the kinked choledocojejunostomy (asterik) to bypass the afferent limb (red shadow). (2) The enteroscope is advanced to retrieve the guidewire (3) and a metal stent is deployed with a colonoscope (4) with resolution of the afferent limb syndrome.
Discussion
ALS is a rare complication after the Whipple procedure, resulting in a high risk of necrosis, perforation, or ascending cholangitis2. In a retrospective case series, Pannala et al.4 reported in patients with 2 years or more of follow-up after pancreaticoduodenectomy for pancreatic cancer, that 13% (24 patients out of 186) developed ALS. Median time to diagnosis was 1.2 years and obstruction was primarily caused by recurrent pancreatic cancer; interestingly, 54% (13 of 24 patients) were found with strictures of the afferent limb and 29% (seven of 24 patients) with angulation of a fixed afferent limb, as in our patient. Chahal et al.5 reported that the success rate of ERCP was 51% (45 of 88 procedures) and it was more likely to be successful for biliary indications (37 of 44 procedures, 84%) than for pancreatic indications (three of 37 procedures, 8%).
Depending on the site of the obstruction, the endoscopic management should be the first treatment option. Many endoscopic techniques have been described to facilitate access to the afferent limb and biliary tree1,3,6,7; however, each technique must be individualized according to the cause of the ALS2,8,9.
In this case, a rendezvous procedure was performed successfully with enteral stent placement. Therefore, there is no gold standard procedure and the endoscopists and radiologists skills are the cornerstone to minimize the morbidity in these patients.











 nova página do texto(beta)
nova página do texto(beta)