Introduction
Conventionally, the options for obtaining liver samples have included percutaneous biopsy (PCB) and the vascular approach. PCB is the most common and has a diagnostic yield between 67% and 94%, with potential complications described in 0.09-3.1% of the cases1. The transjugular approach, which is used as an alternative is not without complications (0.5-6.5%)2. There is evidence that endoscopic ultrasound (EUS) is a useful method for liver pathology25. However, there are some reports with conflicting results mainly in patients with abnormalities in liver function tests (LFTs) without solid liver lesions6.
Clinical case
A 64-year-old woman who went to medical assessment because during general evaluation abnormalities in the LFTs was documented with elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) (ALT 220 IU/L and AST 280 IU/L) with elevated alkaline phosphatase in 350 IU/L. Rest of the LFT were normal. Patient was asymptomatic. In abdominal ultrasound only hepatic steatosis was reported without any other abnormalities. A computed tomography scan of the abdomen reported as normal. Viral hepatitis tests were reported as negatives as well as antibodies antinuclear. LFTs were repeated on two occasions and were founded with similar results. For this reason and due to the desire of the patient, we decided to perform a liver biopsy guided by EUS (EUS fine-needle biopsy [FNB]).
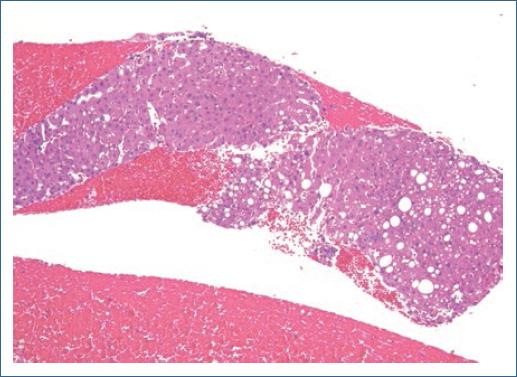
The above procedure was carried out with the new needle EchoTip ProCore 3-20-c (Cook Medical, Limerick, Ireland) which is specifically designed to take liver biopsies. EUS FNB was performed by the conventional manner with capillarity technique (Video 1) and with one single pass. Histopathological result was of “non-alcoholic steatohepatitis” with the presence of evaluable liver tissue sample including 10 portal tracts (Fig. 1).
Discussion
Actually, there are some controversies about if tissue samples of the liver obtained by EUS guidance are a good method for diagnostic approach mainly because the tissue sample obtained with EUS FNA is mainly useful for “cytologic evaluation” and does not allow to see the “architecture” of the parenchyma. EUS FNB is considered as a good option for obtaining better tissue samples compared to EUS FNA7. The previous reports of EUS-guided tissue samples that have included patients with non-specific alterations in LFTs and biopsy were taken randomly from parenchyma and have been showed discrepancy in the results25.
In the present case, the EUS FNB was made with a needle with a new design specifically for achieve a “tissue sample that allows to see architecture in the histologic evaluation.” This specific point could be the difference in many patients with liver diseases traditionally of “difficult diagnosis.” Of course, this is only one case report and we need studies with good simple size that allows a real evaluation. For now, we can say that the new device could represent, in the future, a good option for EUS FNB in patients with abnormal LFTs without a solid liver lesion.











 nova página do texto(beta)
nova página do texto(beta)