Introduction
Spinal cord injury in children (SCI) is a serious disabling disease caused by various factors1. The disease not only causes motor, sensory and autonomic nerve dysfunction below the injury level2, and reduces the basic daily living and social participation abilities but also causes scoliosis, hip dislocation, pressure ulcers, and other complications3. The main clinical manifestations of SCI are sudden pain in the lower back, lower limb motor and sensory disorders, and urinary and fecal incontinence, while the attendant imaging reveals multi-stage abnormal spinal cord signals centered on T9 and T104. The main goal of spinal cord rehabilitation is to restore walking ability and improve walking quality after SCI. Extensive locomotor training can restore locomotion function after SCI in humans.
Activity-based locomotor training (ABLT) is a rehabilitation strategy that, based on scientific and clinical evidence, is designed to enhance the recovery of postural control, balance, standing, walking, overall health, and quality of life following neurologic injury or disease. The program consists of treadmill training with partial weight support, overground assessment, and integration into family and community activities (Fig. 1). As an activity-based therapy, locomotor training is a therapeutic intervention that results in neuromuscular activation below the level of the lesion to promote the recovery of motor functioning with the aim of retraining the nervous system to regain the ability to handle and tackle specific tasks5. Activation of the neuromuscular system occurs during repetitive and progressive practice of the desired task, with the so-called activity-dependent plasticity’ promoting the functional reorganization of the neuromuscular system. Locomotor training focuses on task-specific training of the injured components to return functioning to pre-injury levels of neuromuscular control as far as possible.
While studies have demonstrated that ABLT can effectively promote neuromuscular recovery and improve motor function in children with SCI, thus enhancing their social participation, there is a remarkable lack of standardization regarding the techniques and methods of assessment used to evaluate the effectiveness of rehabilitation6. Therefore, this study systematically reviews the clinical research status of the ABLT used for children with SCI and discusses the effects of the ABLT on rehabilitation in children with SCI. Overall, the study provides a reference and training guidelines for the clinical application of ABLT.
Materials and Methods
Protocol and registration
This systematic review was conducted according to the Cochrane Handbook and is reported following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses declaration (Fig. 2).
Information sources and search
The data sources were the Chinese National Knowledge Infrastructure, WanFang, VIP, PubMed, and Web of Science databases. To identify relevant studies, the following search terms were used: children or SCI or pediatric SCI and locomotor training, sports training, or ABLT.
Inclusion and exclusion criteria
The selection criteria were built based on the PICOs approach, which includes participants, interventions, comparators, outcomes, and study design.
The inclusion criteria were as follows: (i) studies compiled in Chinese or English; (ii) children aged 1-17 years with complete or incomplete SCI; (iii) intervention including body-weight-support treadmill training (BWSTT), robot-assisted gait training (RAGT), overground training (OGT), and community and family integration walking training; (iv) a control group was set up; (v) the outcomes mainly included the evaluation of body structure and function, activities and participation (e.g., American Impairment Scale [AIS], 6 min walking test [6MWT], 10 m walking distance [10WMD], Walking Index of SCI II [WISCI II] and the upper extremity and lower extremity motor score scales [UEMS, LEMS]); (iv) the study type was a randomized controlled study, cohort study, case report study, or cross-sectional study.
The exclusion criteria included the following: (i) duplicate studies; (ii) congenital SCI (spina bifida); and (iii) reviews or systematic reviews.
Data collection process
LITERATURE SCREENING AND DATA EXTRACTION
The relevant databases were searched manually, and the resultant literature was imported into EndnoteX9.0. The titles and abstracts of the studies were initially screened to identify those that did not meet the inclusion criteria. Following this, the content was read to ascertain whether it conformed to this review. The assessment was conducted independently by two researchers, with any differences resolved through discussion and negotiation and the final results determined by the consensus of the research group.
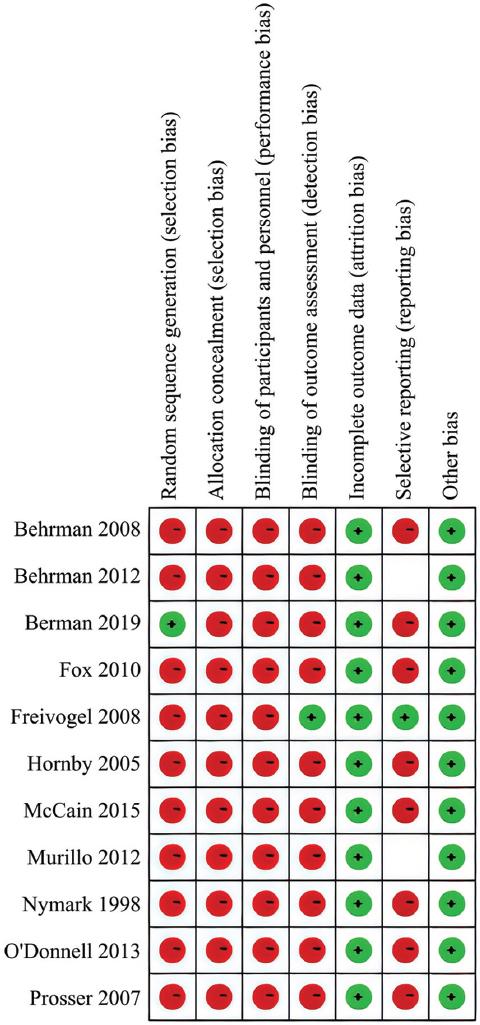
EVALUATION OF THE RISK OF BIAS
Two authors independently assessed the risk of bias. In the case of disagreement, the subject was discussed with another author. The risk of bias was assessed using the Cochrane risk-of-bias tool for literature. Here, a study is considered to be at a “low risk of bias” if all five domains are assessed to be at low risk of bias, while it is considered to be at an overall high risk of bias’ if determined to be at a high risk of bias in terms of at least one domain. The tool was applied to each outcome of interest.
Results
Literature search and article selection
We identified 606 potentially relevant studies through the database search, including 30 from the Chinese database and 576 from the English database. In total, 37 studies were identified after inclusion and exclusion criteria were applied. Finally, by reading the full text, 11 studies were obtained for this review, including 10 case reports and 1 prospective study7-17.
Risk of bias in the individual studies
As noted, the risk of bias was assessed independently by two researchers, with any differences resolved through discussion and negotiation and the final results determined by the consensus of the research group. The seven adopted items were as follows: (i) random sequence generation (10 studies had a high-risk bias and one a low-risk bias); (ii) distribution hiding (11 studies were high-risk bias); (iii) implementation bias (11 studies were high-risk bias; (iv) measurement bias (10 studies were high-risk bias and one was low-risk bias); (v) incomplete data (11 studies had low-risk bias); (vi) selective reporting bias (eight studies had high risk of bias, one had low risk of bias and two studies had unclear risk of bias); and (v) other bias (11 were low-risk bias). The quality assessment results are shown in figure 3.
Basic characteristics of children with SCI
The 11 selected studies included 38 subjects, ranging in age from 1 to 17, with more males than females. The most frequently involved localization was the chest of the spinal cord, followed by the cervical segment and the lumbar segment. The cause of injury in seven of the studies was traumatic SCI (motor vehicle accident, snowboarding accident, football match accident, gunshot accident), and two studies involved non-traumatic SCI (spinal cord disease). Two studies involved traumatic or non-traumatic SCI but were not specifically documented. The sensorimotor function of the patients was evaluated according to the International Standards for Neurological Classification of SCI Scale18. Here, there were seven A-level subjects, six B-level subjects, nine C-level subjects, and four D-level subjects.
Efficacy of ABLT in children with SCI
IMPROVEMENT IN MOTOR FUNCTION AND WALKING ABILITY
Eight studies evaluated the LEMS, and only one study reported a decrease in the LEMS score12. Six studies reported that ABLT improved the WISCI II score, five reported that ABLT improved the 6MWT scores, and seven reported that ABLT improved the 10MWT scores. The AIS grading of three children changed and that of five children did not. The motor function and walking ability scales are shown in table 1.
Table 1 Motor function and walking ability scale score
| Scale \ Study | LMES | WISCI II | 6MWT | 10MWD | AIS |
|---|---|---|---|---|---|
| Nymark et al.7 | Unclear | Unclear | Unclear | ↑0.70 | Unclear |
| McCain et al.8 | ↑6 | ↑12 | ↑61.57 | ↑0.17 | C→D |
| Freivogel et al.9 | Unclear | Unclear | Unclear | ↑0.70 | Unclear |
| Behrman et al.10 | ↑0 | ↑13 | Unclear | Unclear | C→C |
| Prosser11 | ↑23 | ↑12 | Unclear | Unclear | A→C |
| Fox et al.12 | ↓3 | ↑0 | Unclear | Unclear | C→C |
| O’Donnell and Harvey13 | ↑2 | ↑3 | ↑12.90 | ↑1.4 | C→C |
| Berman et al.14 | ↑0 | Unclear | ↑245.33 | ↑0.90 | C→C |
| ↑5 | Unclear | ↑35.00 | ↑0.26 | C→D | |
| ↑1 | Unclear | ↑6.40 | ↑0.42 | C→C | |
| Hornby et al.15 | ↑42 | ↑16 | ↑237.00 | ↑0.26 | Unclear |
| Murillo et al.16 | Unclear | Unclear | ↑200.00 | ↑0.15 | Unclear |
| Behrman et al.17 | ↑11.4 | Unclear | Unclear | Unclear | Unclear |
LEMS: lower extremity motor score; WISCI II: walking index of spinal cord injury II; 6MWT: 6 min walking test; 10MWD: 10 m walking distance; AIS: American impairment scale. ↑Represents the numerical value of each scale improvement after training.
IMPROVEMENT IN DAILY LIVING ABILITY
Four studies recorded the patients’ abilities for basic daily activities. Except for the study by Fox et al.12, the scores on the daily living ability scale were all improved, indicating that the children’s ability to participate in basic daily life was improved after receiving ABLT. Six studies recorded that the patient needed assistive devices to complete family or community walking, including activities using rolling walkers, wheelchairs, crutches, hip, knee, and ankle orthoses, and orthopedic insoles. Among them, the O’Donnell and Harvey13 study reported that these children achieved independent walking. The daily living ability scale scores are shown in table 2.
Table 2 Daily living ability scale score
| Study | Scale | Score | Auxiliary appliance |
|---|---|---|---|
| Nymark et al.7 | Unclear | Unclear | Unclear |
| McCain et al.8 | Unclear | Unclear | Crutches, AFOs, orthopedic insoles |
| Freivogel et al.9 | Unclear | Unclear | Unclear |
| Behrman et al.10 | Unclear | Unclear | Rolling walker |
| Prosser11 | Wee FIM II | Unclear | Rolling walker |
| Fox et al.12 | GMFM-66 | 0 | Rolling walker |
| O’Donnell and Harvey13 | Unclear | Unclear | Independent walking |
| Berman et al.14 | FIM | Unclear | The wheelchair |
| ADL | ↑6 | Unclear | |
| Unclear | Unclear | Manual wheelchairs, LKAFO | |
| Hornby et al.15 | Unclear | Unclear | Unclear |
| Murillo et al.16 | Unclear | Unclear | Unclear |
| Behrman et al.17 | Unclear | Unclear | Unclear |
Wee FIM II: The Functional Independence Measure-II for Children; GMFM-66: Gross Motor Function Measurement-66; FIM: functional independence measure; ADL: activities of daily living; AFOs: ankle foot orthoses; LKAFO: left knee-ankle-foot orthosis. ↑Represents the numerical value of each scale improvement after training.
Discussion
In this systematic review of 11 included studies, we found that ABLT can be an effective intervention in helping to develop or restore walking ability in children with SCI.
The incidence of pediatric SCI in the USA is approximately 2/10,000 children19. Spinal cord injuries in children have devastating consequences. SCI often leads to severe disability due to permanent neurological impairment. Walking recovery, or the development of walking, is a major goal for children with SCI and their families. ABLT is a rehabilitation strategy designed to enhance the recovery of postural control, balance, standing, walking, health, and quality of life after neurologic injury or disease based on scientific and clinical evidence20,21. At present, other than locomotor training, few broadly accepted clinical treatments for SCI exist.
ABLT has a good effect on the rehabilitation of SCI. The study by Harkema et al.22 indicated that rehabilitation that includes intensive activity-based therapy can result in functional improvements in individuals with chronic incomplete SCI. The study by Lucas et al.23 reported that the improvements in children with acquired SCI following ABLT were maintained, indicating that the program is neurotherapeutic. While not achieving complete recovery of trunk control, the immediate effects and sustained improvements provide support for a clinical shift to neurotherapeutic approaches and for continued research to achieve enhanced recovery. Following SCI, ABLT can induce the body to release neurotrophic factors to generate new structures or functions, including the germination of nerve fibers and synapses and the regeneration of injured distal nerve fibers, thus enhancing the plasticity of the spinal cord and promoting the reorganization of neuronal circuits24.
No one form of locomotor training has been determined to be superior. The combination of multiple rehabilitation programs is the best way to achieve the rehabilitation effect of children with SCI17. The ABLT reported in this study consisted of BWSTT, RAGT, OGT, and community and family integration walking training. The BWSTT method allows patients to be in an upright position using suspension devices, which can reduce the issue of upper limb weight for lower limb walking to varying degrees and can change the weight loss ratio and treadmill speed, such that walking training can be carried out with the assistance of therapists25. With the help of therapists, the LEMS, WISCI II, 6MWT, and 10MWD scores of the children in a number of the studies were improved8,13,15. Murillo et al.16 found that after 2 months of RAGT, children with thoracic complete SCI could use a walker for therapeutic walking with the help of therapists. Moreover, this method has a good effect on preventing pressure ulcers and improving intestinal function and lower limb blood circulation. The reconstruction of lower limb motor function is of great significance to the self-care and social integration of affected children7-11,13-17. Altizer et al.26 demonstrated that following RAGT, children can engage in simple family activities, participate in community entertainment activities, and eventually return to school and integrate into collective life.
The ABLT program not only significantly improved motor function and walking ability, as assessed by the 6MWT, 10MWD, and WISCI II scores, in children with SCI, but also had additional benefits. LT has the potential to decrease secondary complications that result from SCI in childhood. The majority of children in a review study completed by Schottler et al.27 demonstrated that children with SCI developed scoliosis if they had a complete injury. Hip dysplasia also occurred in 57% of children. Increased upright mobility, including ABLT, can potentially decrease these complications. Research with adults supports that standing for > 20 min, 3-4 times/week, following SCI, can improve personal well-being, circulation, spasticity, bowel and bladder function, and digestion. One study within this review assessed bowel and bladder function to have improved in children with SCI following ABLT16. Therefore, outcomes such as improved bowel and bladder management, bone density, cardiovascular endurance, and overall quality of life should also be assessed in addition to just ambulation outcomes such as the 6MWT, 10MWD, and WISCI II with future research.
This review has some limitations. The studies that were relevant to this review were mainly case reports, and the effects of different training methods on the motor function and walking ability of children could thus not be compared. Furthermore, the application of ABLT to children with SCI is in its nascent stages.
Conclusions
The ABLT method is a means of rehabilitation for children with SCI. Compared to other conventional exercise training programs, intelligent exercise training is characterized by high accuracy, high intensity, repeatability, and fun, which provides a strong guarantee for the recovery of children’s walking ability, an enhancement in lower limb muscle strength, an improvement in quality of life, and the prevention of complications. With the development of intelligent rehabilitation programs, ABLT will be more widely used to benefit more children with SCI.











 nueva página del texto (beta)
nueva página del texto (beta)