Introduction
Surgical resection is the only strategy to improve survival rates for hilar cholangiocarcinoma (HC), even though, the 5-year survival rate of HC is unsatisfactory, ranging from approximately 14% to 45%1,2. Despite the advances in surgical techniques and perioperative supportive care, the treatment of HC remains challenging. Due to its longitudinally extended infiltrative nature and proximity to vital vascular structures, surgical resection of HC is limited and has unfavorable oncological outcomes3,4. Extended major hepatectomy with concomitant vascular and biliary resection and reconstruction is associated with high perioperative morbidity and mortality rates, and thus, the evolution of surgical management for HC is ongoing. Predictors reported in some previous studies include resection margins, tumor differentiation, and lymph node metastasis5,6. These studies identified a wide range of prognostic factors due to the variation of the follow-up period, including palliative or numerous surgical approaches and R1 resection. Therefore, at present, the predictive factors affecting the survival of HC are ambiguous. The aim of this study is to investigate the predictors and recurrence patterns of HC in a large cohort of patients who underwent R0 resection and had long-term follow-ups.
Methods
Patients
The data of 126 consecutive patients with HC from January 2009 to December 2019 at two hospitals were retrospectively reviewed. Computed tomography (CT) and magnetic resonance imaging (MR) were used to assess tumor infiltration. PET-CT was used to detect suspected distant metastases. Endoscopic ultrasound was also suggested to evaluate biliary and vascular involvement. If patients had obstructive jaundice, endoscopic nose biliary drainage through endoscopic retrograde cholangiopancreatography or percutaneous transhepatic biliary drainage was routinely performed. This study was approved by the hospital's ethics committee, under the approval number 2008-117-(1), and was conducted according to the principles outlined in the Declaration of Helsinki. Each patient provided a written informed consent.
Surgical procedures
During this procedure, bile duct resection (BDR) was routinely performed with both the proximal and distal bile duct margins examined by frozen examination. Resection margins of the distal bile duct and proximal hepatic duct were sent for frozen-section examination during operation. R1 resection was obtained when the resection margin (distal bile duct or proximal hepatic duct or both) was not free from cancer cells under microscope observation. Re-resection of the bile duct or hepatectomy was performed if the bile duct margin was positive on frozen section analysis. All 126 patients underwent R0 resection approved by the frozen section analysis. Lymphadenectomy was also performed by skeletonizing the hepatoduodenal ligament as well as harvesting the lymph nodes along the common hepatic artery and retro-pancreatic region. Other lymph nodes are removed only if they are found to be enlarged or positive on pre-surgical imaging. Overall, however, whether and how a BDR or hepatectomy was performed depended largely on the decision of the surgeon. Complications were ranked in accordance with Clavien–Dindo classifications7. T and N staging was performed following the American Joint Committee on Cancer 8th edition. Chemotherapy (gemcitabine+cisplatin) was administered to patients with lymph node metastasis if they did not refuse, and those with R1 resection received 5-FU-based concurrent chemoradiotherapy.
Follow-up
Patients were followed up at a 3-month frequency during this decade, including a physical examination and a laboratory test. CT or MR was arranged every 3 months for the 1st year and then every 6 months for the 2nd year. CT of the thorax, bone scan, and MR of the brain were performed if clinical examination led to a suspicion of metastasis or PET-CT was performed if other metastases were suspected. The primary end-point of the study was recurrence. The secondary end-points were disease-free survival and overall survival. Recurrence was defined as suspicious or confirmed lesions on imaging or histological examination.
Statistical analysis
Continuous variables were expressed as median and range or mean ± standard deviation, whereas categorical variables were expressed as number and percentage. Chi-squared test was used for nominal data. Univariate analysis with χ2 test or Fisher's exact test was used for categorical variables. When the data did not follow normal distributions, the nonparametric Mann-Whitney U-test was applied. Kaplan-Meier survival was compared using log-rank test. Univariate and multivariate analyses were analyzed through Cox proportional hazard regression. Significance was considered at p < 0.05. SPSS 22 (SPSS, Chicago, IL) was used for statistics.
Results
Baseline and clinicopathological features of HC patients
Thirty-seven patients were included in the non-recurrence group while 89 patients were found to have a recurrence during follow-up. None of the patients in these two groups underwent additional portal vein or hepatic artery resection. No differences were detected between the two groups in terms of age, gender, laboratory tests, proportion of preoperative biliary drainage, proportion of transfusions, incidence of serious surgical complications, and length of hospital stay. Noticeably, the proportion of Bismuth I and II HC was significantly higher in the recurrence group than that in the non-recurrence group (43.8% vs. 24.3%, p < 0.01). In addition, the recurrence group had poorer tumor differentiation, a more advanced N stage, and a higher incidence of perineural invasion compared to the non-recurrence group. No differences were observed in other clinicopathological features between the two groups (Table 1).
Table 1 Baseline features of patients with hilar cholangiocarcinoma
| Variables | Non-recurrence (n = 37) | Recurrence (n = 89) | p value |
|---|---|---|---|
| Age (mean ± SD) | 62.1 ± 6.4 | 61.5 ± 7.8 | NS |
| Sex (male) (n, %) | 27 (73.0) | 67 (75.3) | NS |
| BMI (kg/m2) (mean ± SD) | 21.1 ± 3.1 | 23.2 ± 2.4 | NS |
| Hb (g/dL, mean ± SD) | 15.3 ± 2.3 | 14.7 ± 2.8 | NS |
| Albumin (g/dL, mean ± SD) | 3.8 ± 0.5 | 3.9 ± 0.5 | NS |
| Bilirubin (mg/dL, mean ± SD) | 1.9 (0.3-3.2) | 2.1 (0.4-4.4) | NS |
| CEA (median, range) | 3.2 (0.3-43.4) | 4.0 (0.6-39.2) | NS |
| CA199 (median, range) | 121.6 (2.2-2220.0) | 132.1 (4.5-2490.0) | NS |
| Biliary drainage (n, %) | 7 (18.9) | 15 (16.9) | NS |
| Transfusion (n, %) | 6 (16.2) | 14 (15.7) | NS |
| Complication (≥ IIIa) (n, %) | 2 (5.4) | 6 (6.7) | NS |
| Hospital stay (days, mean ± SD) | 24.2 ± 12.5 | 22.5 ± 10.6 | NS |
| Tumor size (cm, mean ± SD) | 3.5 ± 1.9 | 3.8 ± 1.1 | NS |
| Bismuth type (n, %) | |||
| I + II | 9 (24.3) | 39 (43.8) | |
| III + IV | 28 (75.7) | 50 (56.2) | < 0.01 |
| T stage (n, %) | |||
| 1 | 1 (2.7) | 3 (3.4) | |
| 2 | 26 (70.3) | 64 (71.9) | |
| 3 | 8 (21.6) | 18 (20.2) | |
| 4 | 2 (5.4) | 4 (4.5) | NS |
| N stage (n, %) | |||
| 0 | 31 (83.8) | 54 (60.7) | |
| 1 | 5 (13.5) | 29 (32.6) | |
| 2 | 1 (2.7) | 6 (6.7) | < 0.01 |
| Differentiation (n, %) | |||
| Well | 8 (21.6) | 10 (11.2) | |
| Moderate | 25 (67.6) | 51 (57.3) | < 0.01 |
| Poor | 4 (10.8) | 28 (31.5) | |
| Lymphovascular invasion (n, %) | 8 (21.6) | 18 (20.2) | NS |
| Perineural invasion (n, %) | 23 (62.2) | 67 (75.3) | < 0.05 |
| Adjuvant therapy (n, %) | 7 (18.9) | 20 (22.5) | NS |
NS: not significant; Hb: hemoglobin; CEA: carcinoembryonic antigen; CA199: cancer antigen 199.
Survival analysis in non-recurrence and recurrence groups
Overall survival was significantly worse in the recurrence group than in the non-recurrence group (p < 0.01) (Fig. 1). In both univariate and multivariate analyses, N stage and tumor differentiation were independently associated with disease-free and overall survival of patients (Tables 2 and 3). Disease-free and overall survivals decreased dramatically with the advancement of N stage (p < 0.01) (Fig. 2A and B). Patients with poorly differentiated tumors had the worst disease-free and overall survivals than those of moderate and well differentiation (p = 0.01 and p < 0.01) (Fig. 2C and D).
Table 2 Univariate and multivariate analysis of the risk factors associated with patients' disease-free survival
| Variables | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p value | HR | 95% CI | p value | |
| Biliary drainage | 0.32 | 0.11-2.09 | NS | |||
| Transfusion | 1.21 | 0.24-4.42 | NS | |||
| Complication (≥ IIIa) | 1.33 | 0.36-5.31 | NS | |||
| Tumor size (≥ 3cm) | 0.68 | 0.33-2.55 | NS | |||
| Bismuth type | 0.86 | 0.25-1.31 | NS | |||
| T stage | 2.33 | 0.76-3.44 | NS | |||
| N stage | 3.23 | 2.12-4.37 | < 0.01 | 3.27 | 1.87-4.50 | < 0.01 |
| Differentiation | 2.72 | 1.49-3.58 | < 0.01 | 1.87 | 1.21-2.80 | < 0.01 |
| Lymphovascular invasion | 0.49 | 0.10-2.56 | NS | |||
| Perineural invasion | 3.13 | 0.29-4.86 | NS | |||
| Adjuvant therapy | 0.36 | 0.12-5.22 | NS | |||
NS: not significant ; HR: hazard ratio; CI: confidence interval.
Table 3 Univariate and multivariate analysis of the risk factors associated with patients' overall survival
| Variables | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p value | HR | 95% CI | p value | |
| Biliary drainage | 0.29 | 0.03-3.12 | NS | |||
| Transfusion | 2.5 | 0.25-3.36 | NS | |||
| Complication (≥ IIIa) | 2.03 | 1.03-4.44 | < 0.05 | |||
| Tumor size (≥ 3cm) | 0.91 | 0.46-1.91 | NS | |||
| Bismuth type | 3.11 | 0.27-5.85 | NS | |||
| T stage | 2.20 | 0.60-3.97 | NS | |||
| N stage | 2.05 | 1.12-3.28 | < 0.01 | 3.11 | 1.60-4.24 | < 0.01 |
| Differentiation | 2.91 | 1.78-5.38 | < 0.01 | 2.22 | 1.10-4.76 | < 0.01 |
| Lymphovascular invasion | 2.02 | 0.72-3.85 | NS | |||
| Perineural invasion | 1.40 | 0.26-2.84 | NS | |||
| Adjuvant therapy | 2.22 | 0.22-3.34 | NS | |||
NS: not significant; HR: hazard ratio; CI: confidence interval.
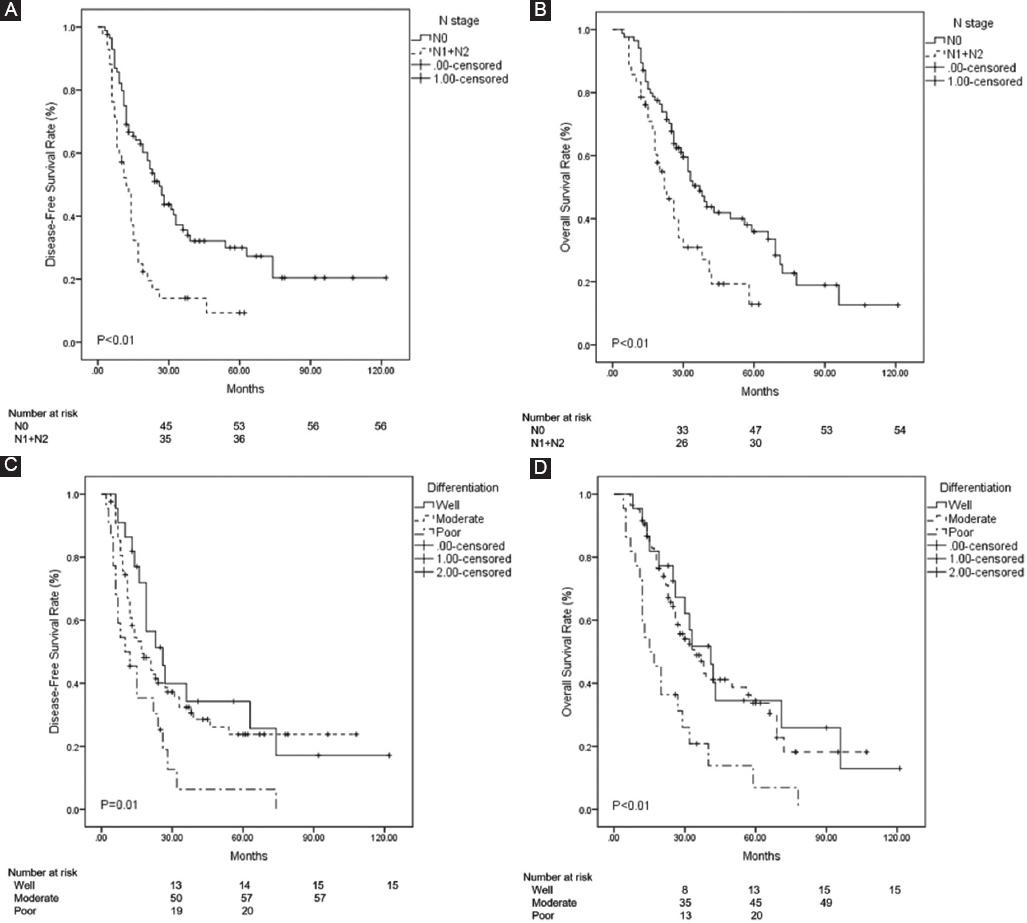
Figure 2 Comparison of survivals in non-recurrence and recurrence groups. A and B: the disease-free and overall survivals shortened dramatically with the advancement of N stage (p < 0.01). C and D: patients with poor tumor differentiation had the worst disease-free and overall survivals than those with moderate and well differentiation (p = 0.01 and p < 0.01).
Patterns of postoperative recurrence
In the recurrence group, local lymph node recurrence was identified to occur more frequently than local anastomosis recurrence, vascular recurrence, isolated locoregional recurrence, distant recurrence, and other recurrences. For distant recurrences, lung metastasis occurred more frequently, followed by liver, abdomen wall, brain, and bone metastasis (Table 4).
Table 4 Patterns of postoperative recurrence
| Recurrence (n = 89) (n, %) | |
|---|---|
| Locoregional metastasis (n, %) | |
| Local lymph node | 40 (44.9) |
| Local anastomosis site | 13 (14.6) |
| Hepatic and portal vessels | 4 (4.5) |
| Isolated locoregional recurrence (n, %) | 30 (33.7) |
| Distant metastasis (n, %) | |
| liver | 5 (5.6) |
| Abdomen wall | 5 (5.6) |
| brain | 3 (3.4) |
| lung | 7 (7.9) |
| bone | 1 (1.1) |
| Others (n, %) | 3 (3.4) |
Survival analysis stratified by surgical strategy in Bismuth I and II HC patients.
We found that the proportion of Bismuth I and II HC in recurrence group was larger than that of the non-recurrence group. Hence, we further determined the factors that contributed to this difference. It was found that the surgical strategy contributed to this difference. BDR combined with hepatectomy was more beneficial than BDR alone for the disease-free and overall survival in Bismuth I and II HC, although the p value was marginal (p = 0.072 and p = 0.045) (Fig. 3A and B). Moreover, in the non-recurrence group, a larger proportion of patients underwent BDR combined with hepatectomy than that in recurrence group (p < 0.01) (Table 5).

Figure 3 A and B: survival analysis stratified by surgical strategy in Bismuth I and II hilar cholangiocarcinoma patients. Bile duct resection combined with hepatectomy benefited the disease-free and overall survivals more than BDR alone in Bismuth I and II hilar cholangiocarcinoma (p = 0.072 and p = 0.045).
Discussion
HC is a relatively rare cancer with an extremely poor prognosis. Radical hepatectomy is the only curative treatment strategy for HC. Surgeons have made tremendous efforts to perform an aggressive surgical approach in spite of technique difficulties8,9. Despite the efforts to improve the prognosis of HC, the 5-year survival rate remains low10. In the past few years, several prognostic factors such as tumor differentiation, lymph node status, and resection margin have been identified. However, the predictive factors for HC are still ambiguous presently. We designed this study to investigate the predictors and recurrence patterns of HC using of a large cohort. We divided the study cohort into a non-recurrent and a recurrence group to compare the recurrence patterns and predictors of HC. As a result, we did find similar results to those previously reported5,6. First, the recurrence group had poorer tumor differentiation, a higher incidence of perineural invasion, and a more advanced N stage compared to the non-recurrence group. Second, in both univariate and multivariate models, N stage and tumor differentiation were independently associated with disease-free and overall survival, which decreased sharply as N stage advanced. Third, patients with poorly differentiated tumors had the worst disease-free and overall survival than those with moderate and well differentiation. Fourth, noticeably, we found that the proportion of Bismuth I and II HC in the recurrence group was higher than that in the non-recurrence group with a great significance, which has not been reported in previous investigations.
We further tried to identify possible answers that could explain this new finding. Previously, there was no survival advantage for HC patients undergoing aggressive surgical approaches due to high mortality11. However, with the advances in surgical techniques and preoperative management, this condition has changed a lot. Mortality rates have become acceptable and survival benefits have been achieved9,12,13. BDR combined with hepatectomy is now a standard procedure for Bismuth III and IV HC, but the benefit of hepatectomy in Bismuth I and II HC remains controversial. A few investigations have suggested that BDR alone was sufficient for Bismuth I and II HC. Otani et al. found that the R0 resection rate and overall survival were similar between local resection for Bismuth I and II HC and combined hepatectomy for Bismuth III and IV HC14. Chen et al. also demonstrated no diversity in long-term survival and recurrence between the two groups15. However, the sample size was relatively small, and thus, selection bias might exist in these studies. In the present study, we found that BDR combined with hepatectomy was beneficial to the disease-free and overall survival in patients with Bismuth I and II HC though the p value was marginal. Nakanishi et al. recommend left hepatectomy for Bismuth type I and II HC without extra ductal tumor invasion in the right side of the hepatic portal region16. However, Zhang et al. found that similar rates of R0 resection were achieved among patients who had BDR versus BDR+ hepatectomy for Bismuth I and II HC. The addition of hepatectomy with or without caudate lobectomy did not result in any survival or recurrence benefits than BDR alone, as long as R0 margin was achieved17. The main limitation of these retrospective studies is the small sample size. We suggest that the need for hepatectomy for Bismuth I and II is condition dependent. Once R0 margin can be achieved and evaluated by the surgeon, hepatectomy is an alternative option. However, future large multicenter studies are still needed to define the optimal surgical strategies for patients with Bismuth type I and II HC. Recent studies pointed out that a positive radial margin is the common cause of R1 resection and has a negative impact on survival18. Similarly, we found a larger proportion of patients who underwent BDR combined with hepatectomy in non-recurrence group than that in recurrence group in the present study of R0 resection patients. Therefore, we believe that more aggressive surgical strategies, such as combined hepatectomy, are critical to achieve R0 resection and improve the survival of Bismuth I and II HC. In addition, local lymph node recurrence was identified to occur more frequently than other recurrences, so we suggest an extensive regional lymph node dissection contributing to curative resection. In summary, it comes into view that the contents mentioned above may support the possibility that a larger proportion of Bismuth I and II HC occupies the recurrence group.
As for the issue of vascular resection, if resection and reconstruction are possible, combined vascular resection can be performed with an acceptable mortality rate and can offer long-term survival to some patients with advanced HC previously considered inoperable19,20. Combined procedures should be encouraged as an option to cure intractable disease as suggested by a meta-analysis21. Nowadays, surgical treatment of HC has steadily evolved, with decreasing mortality and increasing survival rates. Previous reports have emphasized lymph node metastasis, histopathologic status, resection margin, and adjuvant chemotherapy as important prognostic factors for HC22-25. Moreover, recent studies have recommended adjuvant chemotherapy conducted as a bridge modality to improve radical resection rates in locally advanced HC26,27. However, in the present study, we did not find the survival benefit of adjuvant chemotherapy in both univariate and multivariate analyses. Therefore, we advocate that the impact of surgical technique and approach remains important in such malignant tumors.
Conclusions
This study had some limitations because of its retrospective design. Although there were limitations, the new findings of the present study are remarkable and may have some impact on the current guidelines and contribute to the clinical practice in the following aspects. First, N stage and tumor differentiation are the two independent predictors of survival in patients with HC. Second, local lymph node recurrence is the predominant pattern of recurrence in HC. Therefore, we recommend extensive regional lymph node dissection to facilitate curative resection. Third, at present, however, we recommend BDR combined with hepatectomy for patients with Bismuth I and II HC.











 nueva página del texto (beta)
nueva página del texto (beta)



