Introduction
One of the most common intestinal obstructions in newborn babies is congenital duodenal obstruction (CDO)1. Calder published the first work on the subject in 1733. Its frequency has been recorded between 1/6000 and 1/10000 in different series2. According to reports, intensive pre-operative early follow-up of persons with duodenal obstruction and qualified neonatal intensive care methods have dramatically reduced the morbidity and mortality of the disease3. In contrast, problems remain with a baby who starts feeding later. It has been reported for years that sepsis is inevitable in a baby who cannot be fed4. In recent years, in particular, some surgical procedures for repairing duodenal atresia have been proposed5. The placement of a transanastomotic feeding tube (TAFT) is one of the attractive treatments during the repair of duodenal atresia. In several recent studies, placement of a transanastomotic tube has been associated with early feeding and a reduced risk of sepsis6. To assess the evidence on the efficacy and safety of TAFT in neonates with CDO, we conducted a systematic review.
Methods
Search strategy
Using the databases Embase, PubMed, and Cochrane, we carried out a thorough literature search up to 2022. CDO, duodenal atresia, and annular pancreas were the search phrases used. Furthermore, we searched also "duodenal web, annular pancreas, newborn, infant, surgery, parenteral nutrition (PN), post-operative care, transanastomotic tube, and enteral feeding". References and reviews were searched manually for further relevance.
Study selection
Studies comparing TAFT + and TAFT - for CDO were included in the study. Inclusion criteria: (1) clinical studies comparing TAFT + versus TAFT - for CDO and (2) raw data including some of the following: Time to reach full feeds, PN, anastomotic leakage, sepsis, need for central venous catheter (CVC) insertion, mortality, and length of hospital stay. Exclusion criteria: (1) No comparative case series as control and (2) studies could not provide usable raw data or duplicate publications.
Data extraction
Two authors independently reviewed the included studies (SA and MA). We extracted information on sample size, study design, and year of publication. Population data were obtained, including birth weight, age at surgery, type of tube, type of feed, and associated anomaly.
Risk of bias assessment
The risk of bias in the included studies was evaluated using the risk of bias in the Non-randomized Studiesof Interventions (ROBINS-I) method. The reviewers also evaluated the overall risk of bias across all studies for each relevant outcome and considered that information when making decisions about the "quality of evidence."
Statistical analysis
The Review Manager (RevMan) software version 5.4 was applied for statistical data analysis. Measured mean differences and risk ratios were used to evaluate continuous and dichotomous variables. The I2 statistic was employed to quantify the amount of statistical heterogeneity, and the Chi-square test was utilized to determine it. Significance was set at p < 0.05. We applied a random effect model.
Results
Using a PRISMA flow diagram, figure 1 presents an overview of the selection procedure. Forty studies identified during the initial search strategy were retrieved for full-text review, and 9 studies6-14 with 505 CDO patients (223 TAFT and 282 non-TAFT) who met the inclusion criteria were selected.

Figure 1 Preferred Reporting Items for Systematic Reviews and Meta-analysis flow diagram of study selection.
Risk of bias
Table 1 provides a summary of the ROBINS-I tool's risk of bias evaluation. A "severe" or "critical" risk of bias existed in three articles with regard to "Bias due to confounding." Given their retrospective character, all studies had a "moderate" risk of bias in the other categories.
Table 1 Risk of bias (ROBINS-I tool)
| Author | Year | Bias due to confounding | Bias for other domains |
|---|---|---|---|
| Arnbjörnsson et al. | 1987 | Moderate: Integrated retrospective and prospective data. The selection criteria are confusing and not clearly stated. | Moderate |
| Bethell et al. | 2020 | Moderate: Difference in age at surgery | Moderate |
| Cresner et al. | 2022 | Moderate: Unclear study period | Moderate |
| Hall et al. | 2011 | Moderate: Both groups shared comparable fundamental traits | Moderate |
| Harword et al. | 2019 | Moderate: Both groups shared comparable fundamental traits | Moderate |
| Mooney et al. | 1987 | Serious: Patients also received gastrostomy | Moderate |
| Ruangtrakool et al. | 2001 | Critical: Infant distribution differs between the two groups inequitably (4 vs. 30) | Moderate |
| Treider et al. | 2022 | Moderate: Lower weight in the No-TAFT group | Moderate |
| Upadhyay et al. | 1996 | Serious: Patients also received gastrostomy | Moderate |
ROBINS-I: Risk Of Bias in Non-randomized Studiesof Interventions; TAFT: transanastomotic feeding tube.
Outcomes
TIME TO REACH FULL FEEDING
Although seven trials documented time to full feeding, only five studies were suitable for meta-analysis. No statistically significant difference was found between TAFT+ and TAFT- in terms of the time to full feeding, according to meta-analysis (I2 = 93%) (weighted mean differences [WMD]: −1.43, 95% confidence interval [CI]: −8.43-5.58; p > 0.05; Fig. 2). However, the TAFT group's time to reach full feeds was dramatically reduced when the high bias studies were taken out of the equation (I2 = 0%), (WMD: −6.63, 95% CI: −8.83−4.43; p < 0.001; Fig. 3).
CVC insertions
Five studies have discussed CVC insertion. The TAFT + group had significantly less CVC insertion (I2 = 85%), (risk ratio [RR]: 0.43, 95% CI: 0.19-1.00; p < 0.05; Fig. 4).
PN
Although there was no statistically significant difference in the duration of PN (I2 = 80%) (WMD: −2.02, 95% CI: −7.36-3.33; p > 0.05; Fig. 5), fewer patients in the TAFT + group received PN (I2 = 78%) (RR: 0.43, 95% CI: 0.20-0.95; p < 0.05; Fig. 6).
Anastomotic leakage
Anastomotic leakage was not significantly different across the groups (I2 = 0%) (RR: 2.81, 95% CI: 0.50-15.90; p > 0.05; Fig. 7).
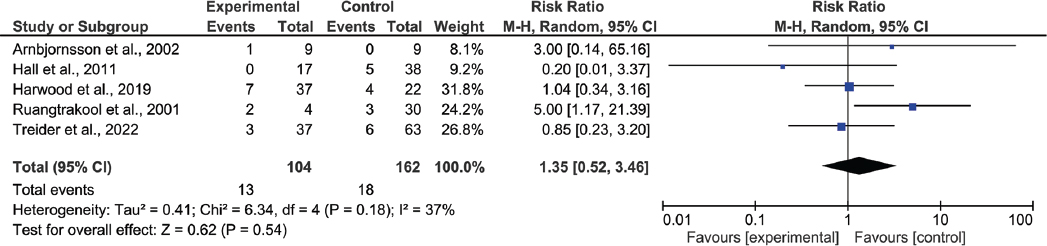
Sepsis
Sepsis was interpreted in five studies. Between the two groups, there was no statistically significant difference in terms of the development of sepsis (I2 = 37%) (RR: 1.35, 95% CI: 0.52-3.46; p > 0.05; Fig. 8).
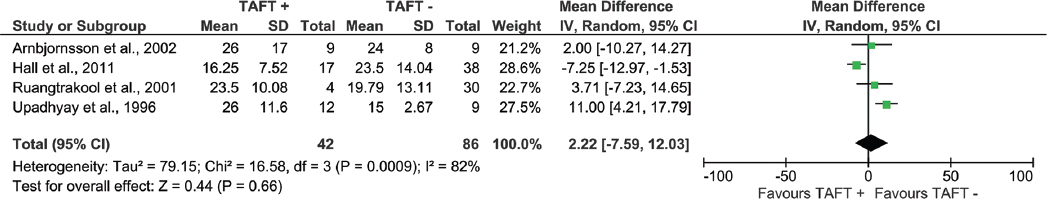
Length of stay
No statistically significant difference was observed in terms of length of stay in the hospital (I2 = 82%) (WMD: 2.22, 95% CI: −7.59-12.03; p > 0.05; Fig. 9).
Mortality
All studies included in the meta-analysis discussed mortality. However, statistical data revealed that there was no statistically significant difference between the groups (I2 = 0%) (RR: 0.55, 95% CI: 0.07-4.34; p > 0.05; Fig. 10).
Discussion
This literature review is the largest meta-analysis, in which cases of CDO treated using the transanastomotic tube are analyzed and discussed in detail. Two hundred twenty-three newborns underwent intraoperative TAFT insertion in this comprehensive review, which include 9 observational trials, while 282 did not. Sepsis and death are caused by the traditional delayed commencement of enteral feeding. Early and trophic feeding has been demonstrated in several trials to decrease sepsis4. In this circumstance, TAFT use is crucial for early feeding in patients undergoing CDO surgery5. Upadhyay et al. reported time to reach full feeding on the 22nd day in the patients who placed TAFT and on the 12th day in the patients who did not14. Ruangtrakool et al. found similar results in both groups (time to reach full feeding on the 15th day)12. However, the TAFT group's time to reach full feeds was dramatically reduced when these two high-bias studies12,14 were taken out of the equation. Similar outcomes were observed by Biradar et al.5.
Long-term malnutrition is an important problem in patients with CDO. This causes significant weight loss and accelerates the catabolic process15. CVC insertion is a recommended method for patients to feed parenterally to prevent weight loss. However, it is fact that TAFT, which has become popular recently, allows early feeding, earlier reaching the full feed. Therefore, TAFT is considered to reduce the need for CVC and PN5. This meta-analysis revealed that the TAFT+ group had significantly less CVC insertion and fewer patients in the TAFT + group received PN. Although PN duration was reported to be very short in an important study conducted in recent years6, no difference in the duration of PN was observed in our meta-analysis even when the high-bias studies were taken out of the equation.
In three studies, anastomotic leakage was detected in a total of 4 patients (3 from the TAFT group and 1 from the no-TAFT group)9,10,13. Due to the small number of observed leakage, the small number of patients in the cohort, and the fact that the studies were not randomized controlled prospective studies, it was exceedingly challenging to predict what the real cause of the anastomotic leak was. However, anastomotic leakage was not significantly different across the groups (I2 = 0%) (RR: 2.81, 95% CI: 0.50-15.90; p > 0.05). Well-designed randomized controlled prospective studies may be a benefit to predict it.
Long-term fasting can cause mucosal atrophy, decreased intestinal enzyme expression, and altered peristalsis, all of which can increase the body's resistance to enteral feeding16,17. Neonatal patients with surgical problems may fare much better if enteral feeds are started and advanced earlier in the post-operative period18,19. Otherwise, sepsis will manifest; if the circumstance worsens, the septic situation may become more severe20. On the contrary, the fed patient recovers more quickly and sepsis diminishes. While there was no sepsis observed in the TAFT + group, Hall et al. found 13% sepsis in the TAFT - group10. Although the TAFT+ group had significantly better results in this meta-analysis in terms of early feeding initiation and early attainment of full nutrition, there was no discernible difference between the two groups in terms of the proportion of patients who developed sepsis.
It was determined that patients with CDO who were treated with the laparoscopic method and patients who started early feeding and reached full nutrition in the early period were discharged early21,22. In the study of Zhang et al., among the 1348 neonatal participants with CDO in the ten studies, 304 received laparoscopic surgery (LS) and 1044 received open surgery (OS). When compared to the OS approach, the LS approach resulted in shorter hospital stays and faster time to initial and full feeding22. In this study, no statistically significant difference was observed in terms of length of stay in the hospital (I2 = 82%) (WMD: 2.22, 95% CI: −7.59-12.03; p > 0.05). However, the number of patients in this area was limited. Well-designed RCTs with a larger number are needed in this area.
Central catheter application and secondary vascular problems; PN and cholestasis after PN; delayed feeding, mucosal atrophies secondary to late feeding, and accelerated sepsis; TAFT application and anastomotic leakage, which is likely to develop secondary to it, is a condition known to be a separate risk factor for mortality5,21,22. All studies included in the meta-analysis discussed mortality. While no mortality occurred in the TAFT + group, there were 5 deaths in the TAFT - group. However, statistical data revealed that there was no statistically significant difference between the groups (I2 = 0%) (RR: 0.55, 95% CI: 0.07-4.34; p > 0.05).











 nueva página del texto (beta)
nueva página del texto (beta)