Introduction
Lumbar disc herniation (LDH) refers to lumbar disc degeneration and rupture resulting in protrusion of the nucleus pulposus. This can lead to compression of the adjacent tissues and is frequently induced by trauma1-3. The main clinical symptoms of LDH include pain in the low back and legs4. Recently, the incidence of people with sedentary lifestyles has increased due to changes in living habits and work styles which have contributed led to an increase in the incidence of LDH5. However, due to patients' insufficient understanding of surgery, the best treatment is often delayed and the long-term lower waist and lower limb pain seriously damages people's physical and mental health6. LDH can cause chronic low back pain, which may last for a long time and recur. The pain produced by LDH can seriously affect people's emotions and cause mental problems such as anxiety, depression, and insomnia7. However, the experience of pain is complex and highly subjective, and is affected by factors such as cognition, emotion, and belief, and it will directly affect the quality and level of life of patients in severe cases8,9. However, due to the insufficient understanding of surgical treatment, it is easy to delay the optimal treatment time, which has severely damaged people's physical and mental health for a long time.
At present, the main treatment measures for LDH include conservative treatments10 and surgery. Conservative treatment includes relieving symptoms and improving functions through a series of physical methods11,12. Surgery aims to decompress the spinal canal and if necessary, perform fusion internal fixation or use another method to maintaining the mechanical stability of the spine and relieve symptoms13,14.
Mixter and Barr15 first reported that sciatica caused by LDH and nerve root compression can be cured by surgery which initiated the era of surgical treatment. Open surgery is the current clinical treatment for severe LDH. The development of minimally invasive technologies16 for disc surgery has recently become more widely used in clinical practice. Open surgery is a high invasive surgery and requires extensive dissection of the muscles and soft tissues of the lower back resulting in severe trauma and post-operative pain17. FD discectomy is a modification of traditional open surgery. LDH surgery can be performed by full or hemilaminectomy. Compared to full laminectomy, hemilaminectomy reduces injuries and complications with good efficacy and shorter recovery times but it cannot completely overcome the disadvantages of traditional open surgery18.
Minimally invasive spinal techniques19 continue to emerge that do not require the paravertebral soft tissues to be stripped and cause reduced levels of trauma, intraoperative bleeding, and post-operative pain with faster recovery times. Furthermore, minimally invasive surgery can overcome the manipulation limitation of spinal canal stenosis and has unique advantages in the treatment of LDH. In this study, we analyzed and compared the safety and efficacy of percutaneous transforaminal discectomy (PTED) and fenestration discectomy (FD) in the treatment of LDH to inform the most appropriate choice of surgical method.
Materials and methods
Research subjects
The complete clinical data of 87 patients with LDH who were treated in our hospital from May 2018 to March 2020 were retrospectively analyzed. The patients were divided into a control group (n = 39) and a research group (n = 48) according to surgical methods. The inclusion criteria were diagnosis of LDH by X-ray and computer tomography examination, complete clinical pathological and follow-up data, patients who had volunteered to participate in the study, patients who were aware of the research and had given written informed consent after the operation, and patients who met the surgical indications.
The exclusion criteria were patients with malignant tumors and liver or kidney dysfunction. No statistically significant differences were observed between the two patient groups in terms of age, gender, stage of disease, course of the disease, and other baseline characteristics. These data are summarized in table 1. This study was approved by the Medical Ethics Committee of our hospital.
Table 1 Baseline data
| Characteristics | Control group (n = 39) | Research group (n = 48) | χ2/t | p |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Male | 21 | 24 | 0.1275 | 0.7211 |
| Female | 18 | 24 | ||
| Mean age (years) | 55.26 ± 16.14 | 54.81 ± 15.83 | 0.1321 | 0.8952 |
| BMI (kg/m2) | 22.31 ± 2.62 | 21.84 ± 2.03 | 0.9427 | 0.3484 |
| Course of disease (day) | 10.26 ± 4.33 | 10.73 ± 4.06 | 0.5212 | 0.6036 |
| Segment | ||||
| L3-L4 | 5 | 9 | 0.5624 | 0.7549 |
| L4-L5 | 26 | 30 | ||
| L5-S1 | 8 | 9 | ||
| Prominent type | ||||
| Side | 27 | 35 | 0.8681 | 0.8331 |
| Central | 6 | 5 | ||
| Near the central | 4 | 4 | ||
| Lateral | 2 | 4 |
BMI: Body mass index.
Surgical methods
Patients in the control group were treated with FD. After successful anesthesia, the patients were placed in the prone position. Iodine and alcohol were routinely used to disinfect the skin in the surgical area, and a sterile surgical drape was put in place. The C-arm of an X-ray machine was used for fluoroscopy. After disinfection, a median incision of 4 cm was made with the spinous process space of the diseased segment defined as the center. The skin was incised from the bony surface of the spinous process on the protruding side of the nucleus pulposus. The tissues were sequentially separated to the upper and lower margins of the lamina space. The bone window was opened and the tissues were separated to expose the dural sac, nerve roots, and the protruding nucleus pulposus. The protruding nucleus pulposus tissue was removed while avoiding the nerve root and dural sac. Finally, a large amount of normal saline was used to wash the operative incision and the dural sac was protected using a collagen sponge to stop the bleeding. After sufficient hemostasis, all the instruments were checked, one drainage tube was put in place and the operative incision was sutured layer by layer to complete the operation.
Patients in the research group were treated with PTED. After routine disinfection, the surgical drape was placed around the surgical field. Under C-arm X-ray fluoroscopy, the location of the surgical incision was marked on the skin using a marker pen. Appropriate lidocaine was used for local infiltration anesthesia and an 18 G puncture needle was used for layer by layer anesthesia. C-arm fluoroscopy showed that the puncture needle was located at the medial edge of the pedicle and the posterior edge of the vertebral body. The puncture needle was inserted into the intervertebral disc and the guide wire was inserted. The dilator was used to expand the channel step by step and the endoscope was inserted. Under the microscope guidance, the diameter of the intervertebral foramen was shown to be too small. The inner edge of the articular process was removed visually using a power grinding drill to ensure that the intervertebral foramen was expanded and the endoscopic channel was established. Under endoscopy, the nerve root was compressed by the protruding nucleus pulposus and the nerve root was fully exposed. The protruding nucleus pulposus tissue was removed by the nucleus pulposus forceps to relieve the nerve root compression. Endoscopic observation showed sufficient decompression of the nerve roots with significant fluctuation. Under direct observation, the endoscope and working cannula were removed and the subcutaneous tissue and skin were sutured with absorbable sutures. The wound was covered with a sterile dressing and the operation was completed. All patients were followed for 1 year after surgery.
Observational indicators
− The surgical conditions of patients in the two groups were compared including intraoperative blood loss, operation times, the length of surgical incisions, the post-operative ambulation starting time, and the length of hospital stays.
− The visual analog scale (VAS) was used to scores pain in the lumbar and legs of patients before surgery, after discharge, and at 3 and 6 months after surgery20. The score was a 10-point system in which 0 indicated no pain and 10 indicated severe pain.
− The surgical efficacy was compared between the two groups. Six months after the operation, the surgical efficacy was determined according to the modified MacNab scoring standard21. When no significant improvements in lumbar and leg pain, lower limb muscle strength and sensorimotor, straight leg elevation were observed, the treatment was considered as having poor efficacy. If slight lumbar and leg pain was reported that did not affect life and work, the muscle strength and sensorimotor of lower limbs were weakened, and the straight leg elevation was ≤ 70° but e 30°, the treatment was considered as having good efficacy. If the lumbar and leg pain disappeared, the muscle strength and sensorimotor of lower limbs returned to normal, and the straight leg elevation was > 70° treatment was considered as having excellent efficacy. Excellent and good rate = (excellent cases + good cases)/total number of cases × 100%.
− The Oswestry Disability Index (ODI)22 was used to evaluate the impact of low back pain on the daily lives of patients before the operation, and 3 months, 6 months, and 1 year after operation. The higher the score, the more serious the dysfunction.
− Before surgery, and at 3 months, 6 months, and 1 year after surgery, the Japanese Orthopaedic Association Score (JOA)23 was used to evaluate the lumbar spine function of patients from four dimensions of objective symptoms, subjective symptoms, daily life restrictions and urination function. The higher the score, the better the function.
− The incidence of complications between the two groups was compared including dural tears, nerve injury, dysesthesia of the limbs on the operation side, infections at the surgical incision, and spinal instability
− The SF-36 scale24 was used to assess the quality of life of patients before and 1 year after surgery including physiological function, role-physical, physical pain, social function, energy, emotional function, mental health, and overall health dimension. The score of each dimension was out of 100 points and higher scores indicated higher quality of life. It mainly included physical function, cognitive function, role function, social function, and emotional function. The higher the score, the better the quality of life.
Statistical analysis
Statistical analysis was performed using SPSS25.0 (SPSS Inc., Chicago, IL, USA). A T-test was used to compare the quantitative data between the two groups. A Chi-square test was used to compare the qualitative data between the two groups. Differences between the means were analyzed using one, two, or three-factor analysis of variance (ANOVA) with or without repeated measurements followed by Bonferroni correction (Bonferroni post-hoc analysis). With an α = 0.05 used as the test standard, a p-value threshold of < 0.05 was set to determine statistical significance.
Results
The operation status of the two groups of patients
The amount of intraoperative blood loss in the research group was lower than in the control group. The operation times, lengths of surgical incisions, the post-operative ambulation starting times and the lengths of hospital stays were statistically shorter in the research group compared to the control group (p < 0.05). The data are summarized in table 2.
Table 2 Comparison of surgical conditions between the two groups
| Groups | Intraoperative blood loss (mL) | Time of operation (h) | Length of incision (cm) | Postoperative ground time (day) | Length of stay (day) |
|---|---|---|---|---|---|
| Control group (n = 39) | 131.65 ± 25.14 | 1.97 ± 0.34 | 0.77 ± 0.18 | 3.34 ± 0.41 | 14.87 ± 3.94 |
| Research group (n = 48) | 29.58 ± 8.29 | 1.77 ± 0.23 | 2.87 ± 0.69 | 2.16 ± 0.97 | 10.67 ± 4.07 |
| χ2/t | 26.4450 | 3.2611 | 18.4839 | 7.0936 | 4.8556 |
| p | < 0.0001 | 0.0016 | < 0.0001 | < 0.0001 | < 0.0001 |
VAS scores of the two groups of patients
The VAS scores reporting the degrees of pain were compared between the two patient groups before surgery, at discharge, and 3 and 6 months after surgery. The results showed no significant differences in the pre-operative VAS scores between the two groups (p > 0.05). The VAS scores of patients in the research group were significantly lower than in the control group at discharge and at 3 months after surgery (p < 0.05). At 6 months after surgery, there was no significant difference in the VAS scores between the two groups (p > 0.05). The data are presented in figure 1.
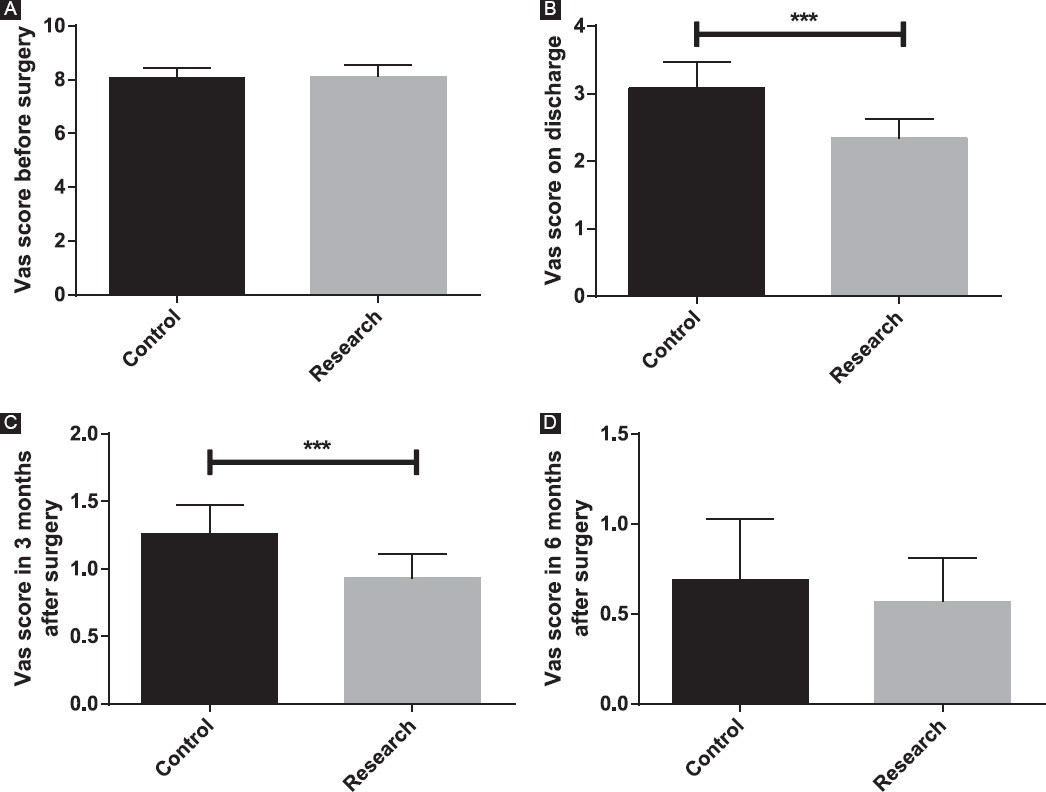
Figure 1 Comparison of visual analog scale (VAS) scores between the two groups. A: pre-operative VAS scores of the two groups of patients. B: VAS scores of the two groups of patients at discharge. C: VAS scores of the two groups of patients 3 months after surgery. D: VAS scores of the two groups of patients 6 months after surgery.*** p < 0.001
The efficacy of PTED and FD
Six months after surgery, the incidence of excellent and good surgical outcomes in the research group was significantly higher than in the control group (p < 0.05) as shown in table 3.
The ODI scores of the two groups of patients
No significant differences in pre-operative ODI scores were observed between the two groups (p > 0.05). From 3 months to 1 year after surgery, the ODI scores of the two groups showed a downward trend, and the ODI scores of the patients in the research group were significantly lower than in the control group at 3 months after surgery (p < 0.05). However, there was no significant difference in the ODI scores between the two groups at 6 months and 1 year after surgery (p > 0.05), as shown in table 4.
Table 4 Comparison of Oswestry Disability Index scores between the two groups
| Groups | Pre-operative | 3 months after surgery | 6 months after surgery | The first year after surgery |
|---|---|---|---|---|
| Control group (n = 39) | 54.68 ± 6.48 | 39.64 ± 4.68 | 14.68 ± 2.84 | 12.34 ± 1.77 |
| Research group (n = 48) | 53.84 ± 7.21 | 24.15 ± 3.22 | 13.79 ± 3.67 | 12.19 ± 1.48 |
| χ2/t | 1.4860 | 0.8494 | 0.7167 | 0.3484 |
| p | 0.5734 | < 0.0001 | 0.2177 | 0.6679 |
The JOA scores of the two groups of patients
No significant differences were observed in the pre-operative JOA scores between the two groups (p > 0.05). From 3 months to 1 year after surgery, the JOA scores of the two groups showed an upward trend, and the JOA scores of the research group were significantly higher than the control group at 3 months after surgery (p < 0.05). However, there was no significant difference in the JOA scores between the two groups at 6 months after and 1 year after surgery (p > 0.05). The results are presented in table 5.
Table 5 Comparison of Japanese Orthopaedic Association scores between the two groups
| Groups | Pre-operative | 3 months after surgery | 6 months after surgery | The 1st year after surgery |
|---|---|---|---|---|
| Control group (n = 39) | 12.64 ± 1.38 | 16.48 ± 2.06 | 21.87 ± 2.11 | 23.84 ± 3.24 |
| Research group (n = 48) | 12.21 ± 1.52 | 19.17 ± 1.87 | 22.73 ± 2.46 | 24.26 ± 3.91 |
| χ2/t | 0.3145 | 0.4219 | 0.4980 | 0.7816 |
| p | 0.1752 | < 0.0001 | 0.0878 | 0.5924 |
The incidence of complications of the two groups of patients
In the research group, there was one case of hypoesthesia in the operative limb and two cases of incision infection. The total incidence of complications was 6.25%. In the control group, there was one case of dural tear, one case of nerve injury, two cases of hypoesthesia in operative limb, three cases of incision infection, and two cases of spinal instability. The total incidence of complications was 23.7% which was significantly higher than the control group (p < 0.05).
Quality of life of the two groups of patients
After 1 year of follow-up, the two groups were compared in terms of physical, cognitive, social, and emotional functions. Our data showed that before the treatment, there was no significant difference in the quality of life indicators between the two groups (p > 0.05). At 1 year of follow-up, the scores of all indicators in the two groups showed an upward trend, but there were no significant differences between the two groups (p > 0.05). The data are summarized in table 6.
Table 6 Comparison of complications between the two groups
| Groups | Dural tear | Nerve injury | Numbness of sensation in operative limb | Infection of incisional wound | Spinal instability | Total incidence |
|---|---|---|---|---|---|---|
| Control group (n = 39) | 1 | 1 | 2 | 3 | 2 | 9 (23.1) |
| Research group (n = 48) | 0 | 0 | 1 | 2 | 0 | 3 (6.25) |
| χ2/t | 5.1241 | |||||
| p | 0.0236 |
Discussion
The intervertebral disc plays an important role in supporting the spine. As people age, the intervertebral discs begin to degenerate25. As the water content of the nucleus pulposus decreases, the probability of prolapse gradually increases. Furthermore, the fibers in the annulus fibrosus become thick, brittle, and can develop cracks. After compression or even distortion, increased pressure of the nucleus pulposus leads to protrusion from the cracks into the spinal canal. This stimulates and compresses the spinal nerves and spinal cord causing a series of symptoms associated with LDH26. LDH is caused by the disordered structure and function of the intervertebral disc. Patients with LDH often present with pain, numbness, and other symptoms27 with major impacts on quality of life. There is an unmet clinical need for the development of effective treatment for patients with LDH.
In this study, we analyzed the safety and efficacy of PTED and FD in the treatment of LDH. The results showed that the two groups of patients completed surgery. Patients in the research group had lower levels of intraoperative blood loss, operation times, incision lengths, post-operative ambulation starting times, and hospital stays compared to those in the control group. These findings may be due to the target being visible during PTED. Furthermore, the location of the ruptured annulus fibrosus can be accurately located by contrast before surgery to reach the protruding position28. The removal of the nucleus pulposus and direct decompression of nerve roots experience less damage from the spinal bone, paravertebral muscles, and soft tissue and so there is less damage to the body. Moreover, in PTED, the incision is smaller, there is less blood loss and the post-operative recovery is faster, thus shortening the hospital stay of patients.
The VAS scores of patients in the research group were significantly lower than the control group at discharge and at 3 months after surgery, but there were no significant differences between the two groups at 6 months after surgery (p < 0.05). The results showed that both surgical procedures significantly improved the pain caused by LDH but that FD required stripping of the paravertebral muscles on the articular process and spinous process. This resulted in injury of the innervation nerve, muscle denervation, muscle degeneration and atrophy, and post-operative lumbar pain29. PTED is a minimally invasive operation. Radiofrequency therapy can repair the damaged annulus fibrosus, reduce intraoperative blood loss, and reduce the risk of post-operative nerve root adhesion and intraspinal scar formation. Moreover, radiofrequency therapy can denervate the intervertebral disc and relieve pain30. By comparing the ODI and JOA scores of patients at 6 months and 1 year after surgery, the ODI score of the research group was significantly lower than the control group. At 3 months after surgery, the JOA score was significantly higher than the control group. As pain is an important factor that impacts the recovery of lumbar spine function after surgery, if the sensation of pain sensation is relatively low, it can avoid the inability to get out of bed for functional rehabilitation training due to intolerable pain, which is conducive to shortening the recovery time of the body function31.
The incidence of complications in the research group was significantly lower than the control group. PTED guarantees the safety of anatomical positions, and with the help of an endoscope can obtain a clear surgical field of vision. Furthermore, it can avoid damage to important tissues and organs such as blood vessels and the dura mater. The reduction of local damage is beneficial in lowering risks related to post-operative complications, maintaining the anatomical structure and the biomechanical stability of the lumbar spine32. Saline perfusion during PTED can also clear inflammatory mediators around the diseased intervertebral disc and prevent the accumulation of by-products caused by heat treatment to avoid infection33. Finally, we compared the pre-operative and post-operative life quality scores of the two groups, and found no significant differences between the two groups (p > 0.05). Our results showed that both surgical procedures had long-term effects.
Conclusion
In conclusion, PTED and FD can effectively relieve pain and improve lumbar function in patients with LDH. However, PTED can significantly reduce the amount of intraoperative bleeding, trauma, recovery times, and the incidence of post-operative complications. Furthermore, PTDE was shown to be a safer approach and can be routinely used in the clinic.











 nueva página del texto (beta)
nueva página del texto (beta)


