Introduction
Post-incisional ventral hernias are abdominal wall defects secondary to a previous surgical event. The risk of presenting this complication is 5-30%1 after a midline exploratory laparotomy. It is an entity that increases morbidity and has a direct impact on the quality of life of patients. The ventral hernia that initially formed tends to increase in dimensions due to a mechanical effect, generating retraction of the muscles of the wall in a lateral direction, which conditions atrophy and fibrosis2. When presenting these anatomical changes, a series of events occur that can modify the respiratory physiology. As the viscera migrate to the hernial sac (HSV), there is a decrease in intra-abdominal pressure, affecting the stability, balance, and movement of the diaphragm, as well as a decrease in venous return in the porta and cava. The mesentery, omentum, and intestine become swollen and thickened by chronic inflammation caused by mechanical irritation with the hernial ring, with the consequent formation of flanges or adhesions. The skin and subcutaneous cellular tissue atrophy by mechanical compression of the HSV3. The dimensions of the defect and the systemic effects classify it as a hernia with loss of dominance, of which there is no standardized definition2. Tanaka et al., through tomography, he described the volume of the HSV and volume of the abdominal cavity (VAC) to generate a HSV/VAC ratio, if it is > 25% then it can be defined as loss of domain4. There is the possibility of performing pre-operative procedures such as the application of tissue expanders, bolutinum toxin Type A (BTA), and progressive pneumoperitoneum (PN).
Clinical case
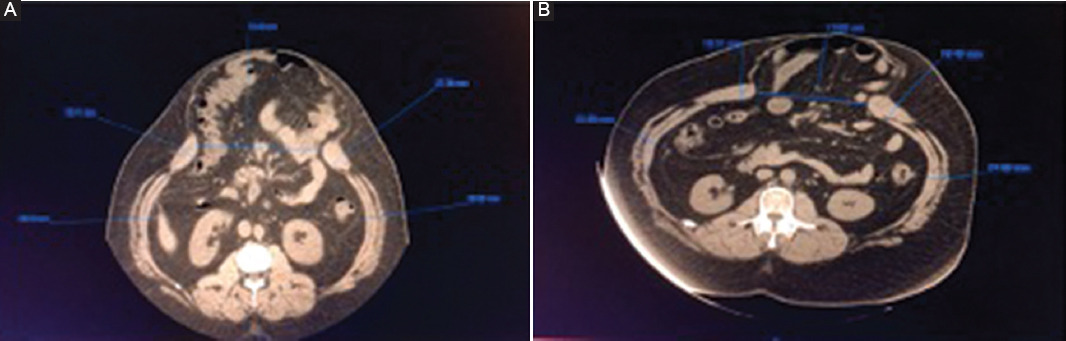
This is a 27-year-old male patient, which presents Grade 3 obesity according to the body mass index (43.4 kg/m2), without chronic degenerative diseases. He suffered from complicated appendicitis in 2019, which required emergency exploratory laparotomy. A post-incisional ventral hernia involving the midline was detected (Fig. 1). The patient was classified as a ventral hernia with loss of domain of 19 months of evolution. We use application of BTA in the muscles of the lateral wall of the abdomen and NP. Before applying both techniques, the patient was given an informed consent form, explaining the risks and benefits of both procedures. It began with a tomographic control in which a defect of the abdominal wall of 18.46 cm in its transverse diameter and a diameter of 28.43 mm and 28.52 mm of the muscle groups of the lateral wall (right and left, respectively), with a Tanaka index of 58%. The first step was the application of BTA Xeomeen® (Merz Pharmaceuticals GmbH, Frankfurt, Germany). The procedure was scheduled in the ultrasound room, 1 month before the planned date for surgery. The presentation of the vial of BTA (Xeomeen®) is 100 units. Three vials were used, each diluted in 5 mL of 0.9% sodium chloride solution. Our goal was to use 300 units in total, of which 150 U on each side of the abdomen and 30 U per application site. The patient was placed in a lateral decubitus position, after mapping the 5 points established in the literature. Under the asepsis and antisepsis protocol, local anesthesia with 2% lidocaine was infiltrated at the puncture sites. By means of ultrasound, the muscular bellies were located; The 22 Gauge Quincke needle was introduced, depositing 0.5 mL in each muscle layer, starting in the transverse muscle, followed by the minor oblique and finally the greater oblique; depositing 1.5 mL in total, which is equivalent to 30 U of BTA (Fig. 2). The application is made on both sides of the abdominal wall. At the end of the procedure, the patient was kept under observation for 1 h without complications. The patient was summoned 4 weeks later, who only mentioned perceiving the sensation of "flaccidity" in the abdomen.
The PN guided by tomography was performed in week 4. Local anesthesia was infiltrated with 2% lidocaine and the Veress needle was inserted at the Palmer point corroborating its entry into the abdominal cavity by means of tomography. Subsequently, the metal guide was inserted and the Veress needle was withdrawn; the site is enlarged with a scalpel and the dilator is placed, which is then removed, and the central venous catheter is inserted through the guide (a double lumen catheter of 7Fr and 20 cm in diameter was used). With a 60 cc syringe, 100 cc of ambient air was introduced, corroborated by image and at the moment of insufflation with the movement of the HSV; therefore, the administration of 2000 cc of ambient air is concluded. Finally, the catheter is fixed to the skin and covered with sterile gauze. The patient is kept under surveillance for 2 h without complications. Was monitored as an outpatient with analgesics and antibiotics. The patient was summoned 9 days later to the outpatient clinic to maintain the PN, performing the insufflations and applying approximately 500-1000 cc once a day, to observe distension of the abdominal cavity and a feeling of fullness (Fig. 3). A total of 7500 cc was insufflated for 9 days. The patient presented left subscapular pain that subsided with the administration of paracetamol and emphysema in the lateral wall of the abdomen that resolved spontaneously.

Figure 3 Tomography-guided PN placement. A: insufflation of ambient air through the catheter. B: axial tomography with the presence of the catheter and PN. C: the catheter is covered and the PN is maintained.
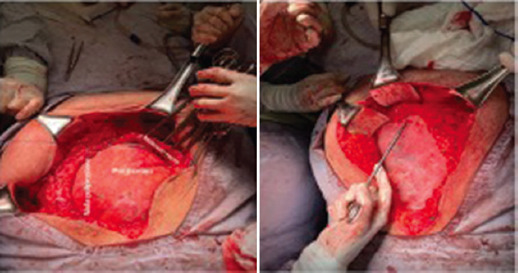
The baseline tomography was compared with the control at week 4 after the application of BTA, where a reduction of 4.81 cm was evidenced in the defect, as well as 5.55 mm in the right and 3.86 mm in the left in the diameter of the lateral muscle groups (Fig. 4). The patient was hospitalized 24 h before the date of surgery. The ventral plasty was performed with Rives technique 5 weeks after the application of BTA and 9 days of PN (Fig. 5). The catheter was removed in the operating room. With a surgical time of 180 min, the surgery was completed with the patient hemodynamically stable. The patient undergoes the mediate postoperative period in adequate general conditions; Intra-abdominal pressure was monitored, ruling out intra-abdominal hypertension. It was started orally at 24 h, did not present complications, and was discharged at 96 h. In outpatient follow-up, drains were removed at 2 weeks when the output was < 30 cc/24 h and the skin staples at 3-week postoperatively. In 6 months of follow-up (Fig. 6), the patients were without complications, clinical evidence of recurrence, with a full reintegration to work life.
Discussion
Botulinum toxin Type A is one of the eight toxin serotypes (A-H) produced by bacteria of the genus clostridium (botulinum, argentinensis, barati, and butyrricum)5. Known for its multiple medical applications in urological conditions, achalasia, hyperhidrosis, migraines, cerebral palsy, cosmetics, strabismus, depression, and among others6,7. It acts at the nerve endings, inhibiting the release of acetylcholine in the neuromuscular plate8, causing a chemical denervation that will weaken muscle contraction, generating reversible muscle atrophy. Its use has currently been implemented in the preparation of patients with incisional hernias of the abdominal wall, first reported in 2009 by Ibarra-Hurtado et al.9 There is no equivalence or standard dose between the different commercial presentations for use on the abdominal wall. Studies have been carried out on the pharmaceutical and biological properties of the different BTA presentations, finding a 1:1 relationship between Xeomeen® and Botox® (Allergan, Irvine, CA), and these in turn 1: 2.5-3 with Dysport® (Ipsen Ltd, Slough, Berkshire, UK)10. Its application in the muscles of the lateral wall of the abdomen will condition a flaccid paralysis that will allow its lengthening temporarily11, with a maximum effect reported between week 4 and 6 after its application, which is reversible and can last from 6 to 9 months. Achieving a decrease in the transverse diameter of the HSV, thinning the diameter of the lateral muscles and the dimensions of the abdominal cavity, favoring a tension-free repair9,12. Contraindications for its use are hypersensitivity to the toxin or its components, infection of the site, and myasthenia gravis7. The application is carried out by electromyography and guided by ultrasound to deposit the BTA with precision in each muscle layer13. Using anatomical references, Ibarra-Hurtado et al.9 described 5 points of application on each side of the abdomen and later other authors have proposed 3 points of application12,13. The dose varies in different reviews, documenting from low doses of 100 U14-500 U9 in total. The toxic dose was studied by intraperitoneal injection in mice (MLD50) and in Rhesus monkeys, calculating that the toxicity in intramuscular application is 2730 U of Botox® and the lethal dose is 5,000 U of Botox®7,15. Its use is considered safe, since the dose used is well below the toxic dose; in the same way, due to its localized effect at the application site, reporting up to 25% of mild, temporary, and non-systemic adverse effects related to the mechanism of action6, no mortality has been reported due to its application to the abdominal wall. Incobotulinumtoxin A itself does not have complex proteins; therefore, it has low immunogenic potential. Some studies describe that it does not produce antibodies10, reducing the probability of tachyphylaxis.
PN as a preparation for ventral hernias was first described in 1946 by Goni-Moreno16. Its objective is to increase intra-abdominal pressure to improve ventilatory function, correcting the position of the diaphragm, returning the organs to the cavity, improving portal circulation, and reducing intestinal and mesentery edema. The presence of air in the cavity generates pneumatic lysis of adhesions, it also has an impact on the immune system, improving healing. The puncture site described varies according to the patient, identifying a point far from the scars on the skin from the previous surgeries. The amount of ambient air to be insufflated will depend on the size of the hernia and the patient's tolerance to PN; which regularly does not exceed 12-15 mmHg. Initially, 1000-4000 cc of ambient air are introduced, and later maintenance with daily insufflation of 1000-2000 cc17. An objective measurement can be carried out with the insufflator of the laparoscopy tower or a sphingomanometer. The PN maintenance time varies according to the authors, from 7 to 15 days until the day of surgery. Up to 12% complications are reported due to its application, mainly pain radiating to the scapular region, subcutaneous emphysema, and infection of the puncture site, without associated direct mortality. There are case series in which both techniques were used18,19. During the review of the literature for the preparation of this article, we did not find another publication in which incobotulinumtoxin A has been used for application to the abdominal wall.
Conclusion
Both techniques have shown a benefit to achieve a tension-free closure of the abdominal wall, which is one of the objectives when performing hernia repair. These advantages are also reflected in the post-operative period avoiding the presence of abdominal compartment syndrome, although the number of cases should be increased. Despite not being standardized the dose of BTA and the amount or time of PN. Both techniques are easy to reproduce and safe, increasing their level of safety when performed guided by image. It will be necessary to carry out more studies to be able to specify it.











 nueva página del texto (beta)
nueva página del texto (beta)