Introduction
Periampullary region tumors (PRT) include the tumors arising from pancreatic head, ampulla of Vater, duodenum, and distal common bile duct1. Among these tumors, pancreatic head adenocarcinomas present the worst prognosis with a 5-year overall survival of 20%2,3. Pancreaticoduodenectomy (PD) is considered as the curative resection method for the PRT. However, mortality rates of PD are reported < 5% in many published series, morbidity rates are still remains high from 40% to 50%4.
Sarcopenia is defined as loss of skeletal muscle mass, strength and function. It is related to prolonged hospitalization, mortality, adverse metabolic affects, and poor quality of life5. There are many different types of methods used for evaluating the quantity and quality of muscle mass such as dual-energy X-ray absorptiometry, bioelectrical impedance analysis, lumbar muscle cross-sectional area by computed tomography (CT), or magnetic resonance imaging. The skeletal muscle area (SMA) is one of the parameters that shows sarcopenia. SMA is measured on the inferior end plate of the L3 vertebra and reflects the sum of the surface areas of all the muscles (i.e., psoas, paraspinal, transversus abdominis, rectus abdominis, quadratus lumborum, and internal and external obliques) in this axial image6,7. Prognostic nutritional index (PNI) is calculated with the formula 10 × serum albumin level (g/dL) + 0.005 × total peripheral lymphocyte count (per mm3) from serum albumin level and total lymphocyte count8. PNI shows the nutritional status of the patients and it is known as a predictive value of morbidity and mortality in pancreatic cancer9. In this study, we aimed to identify the effects of pre-operative SMA and PNI values on post-operative mortality and morbidity in patients with PRT.
Materials and methods
Patients that underwent PD for periampullary region malignant tumors between January 2010 and January 2020 were retrospectively analyzed. Patients' age, gender, comorbidities, localizations of the tumor, histological types of tumor, tumor stages, American Society of Anesthesiology (ASA) scores, total lymphocyte counts, pre-operative levels of albumin, pre-operative PNI, pre-operative SMA, post-operative mortality and morbidity, post-operative hospital stay, and post-operative Clavien Dindo complication scores were defined as parameters. PNI was calculated with the formula of Onodera according to the laboratory parameters that checked 1 week before the operation. SMA values of patients were measured by retrospective examination of CT scans that taken in the supine position for the tumor staging before the surgery. Patients were divided into two groups for SMA and PNI according to their cutoff values that found in receiver operating characteristic (ROC) curve analysis. Differences between these groups for post-operative hospital stay, mortality, and morbidity were statistically analyzed. Data were statistically analyzed using IBM SPSS Statistics 25.0 package program. As the descriptive statistics, the number of units (n), percent (%), mean ± standard deviation (x´ ± ss), and Median (Q1-Q3) values was given. Pearson Chi-square and Fisher's exact test were used to evaluate categorical variables. The normal distribution of data's continuous variables were evaluated by Shapiro-Wilk, normality test, and Q-Q graphs. In the comparison of the continuous variables of the two groups, the Independent Sample T test was used for variables with normal distribution, and Mann-Whitney U test for variables that did not fit the normal distribution. Univariate analysis was performed to find potential risk factors and then multivariate analysis was added to identify independent factors. p < 0.05 value was considered statistically significant.
Results
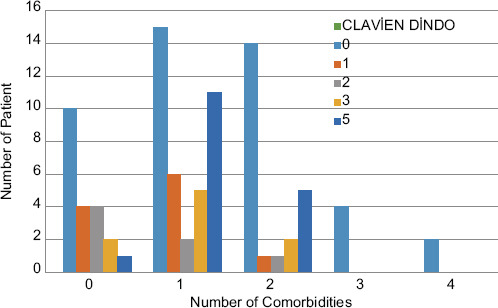
A total of 89 patients were detected. The mean age was 65.94 ± 11.242 and 54 (60.6 %) of the patients were male. Eleven (12.4%) patients were diagnosed as distal common bile duct tumor, 42 (47.2%) patients were diagnosed as pancreatic head tumor, and 36 (40.4%) patients were diagnosed as ampulla tumor. Patients' tumor localizations, histological types of tumor, and stages are summarized in table 1 in detail. The mortality and morbidity rate were 19% and 30%, respectively. The most common complication after PD was surgical site infection with 13 patients and the second one was pneumonia with 10 patients. Other complications are summarized in table 2 with details. Patients were divided into two groups according to their cutoff PNI and SMA values that calculated with the ROC analysis. Mean for the PNI in patients who have morbidity and mortality was found 42.52 ± 8.034 and 38.40 ± 7.881, respectively. Cutoff value for PNI was found 43 and patients were divided into two groups as patients with PNI ≤ 43 and PNI > 43. Morbidity, mortality, hospital stay, and Clavien Dindo complication scores were compared between these groups. In patients with low PNI group, mortality and Clavien Dindo complication score were significantly higher (p = 0.010, p = 0.011) (OR for mortality 0.220, 95% CI 0.065-0.740) (Table 3). SMA values were calculated separately for male and female patients. Mean SMA values for male and female in patients with mortality and morbidity were found as 112 ± 26.453, 109.83 ± 26.713, and 94.20 ± 14.412, 87.55 ± 15.572, respectively. According to SMA ROC analysis, cutoff values for female and male were 87 and 113, respectively. Patients were divided into two groups and they were compared for morbidity, mortality, hospital stay, and Clavien Dindo complication scores. In both groups, SMA was not associated with morbidity, mortality, hospital stay, and Clavien Dindo complication score (Table 3). We also categorized patients according to presence of mortality and morbidity. Then, we compared these groups for age, gender, ASA score, lyphocyte count, serum level of albumin, and comorbidities. Hypertension and diabetes mellitus were significantly lower in patients with morbidity (p = 0.035 and p = 0.045). Serum level of albumin was lower in patients with mortality (p = 0.011). Furthermore, chronic obstructive pulmonary disease (COPD) was higher in patients with mortality (p = 0.040) (Table 4). Distribution of comorbidity numbers according to Clavien Dindo complication score was also analyzed and we could not find an association between these parameters (Fig. 1). We did univariate and multivariate analysis for factors affecting morbidity and mortality. Hypertension was found a reducing factor for morbidity in both univariate and multivariate analysis (p = 0.039 and p = 0.045) (odds ratio [95% CI]: 0.350 [0.129-0.946] and 0.303 [0.095-0.973]). COPD and low PNI were found as enhancing factors for mortality in univariate analysis (p = 0.046 and p = 0.014) (odds ratio [95% CI]: 3.177 [1.019-9.907] and 4.550 [1.351-15.329]). However, only low PNI was found as enhancing factor for mortality in multivariate analysis (p = 0.024) (odds ratio [95% CI]: 4.836 [1.233-18.967]) (Table 5).
Table 1 Localizations, histological types, and stages of the periampullary region tumors
| Histological type and stage | Localization of the tumor, n (%) | ||
|---|---|---|---|
| Distal Choledoc (n = 11) (12.4%) | Pancreatic head (n = 42) (47.2%) | Ampulla of Vater (n = 36) (40.4%) | |
| Histological type of tumor | |||
| Adenocarcinoma | 7 (63.6%) | 33 (78.6%) | 34 (94.4%) |
| Cholangiocarcinoma | 4 (36.4%) | - | - |
| Intraductal papillary mucinous neoplasia | - | 6 (14.35%) | - |
| Neuroendocrine tumor | - | 2 (4.8%) | - |
| Lymphoma | - | 1 (2.4%) | - |
| Squamous cell cancer | - | - | 1 (2.8%) |
| Gastrointestinal Stromal tumor | - | 1 (2.8%) | |
| Tumor stages | |||
| Stage 1 | 2 (18.2%) | 5 (11.9%) | 12 (33.3%) |
| Stage 2 | 6 (54.5%) | 18 (42.9%) | 3 (8.3%) |
| Stage 3 | 3 (27.3%) | 10 (23.8%) | 19 (52.8%) |
Table 2 Post-operative complications in patients underwent PD
| Complication | Number of patients (n) |
|---|---|
| Surgical site infection | 13 |
| Pneumonia | 10 |
| Acute renal failure | 4 |
| Brid ileus | 3 |
| Intra-abdominal abscess | 2 |
| Eviscereation | 2 |
| Gastrointestinal bleeding | 1 |
| Grade D esophagitis | 1 |
| Hepatic abscess | 1 |
| Cholangitis | 1 |
| Central venous catheter infection | 1 |
PD: pancreaticoduodenectomy.
Table 3 Factors associated with low and high PNI and SMA values
| Postoperative features | All patients (n = 89) | Low PNI (PNI £ 43) (n = 43) | High PNI (PNI > 43) (n = 46) | p value | Low SMA (n = 43) | High SMA (n = 46) | p value |
|---|---|---|---|---|---|---|---|
| Postoperative length of hospital stay; median (Q1-Q3) | 13 (10-20) | 13 (9-21) | 13 (11-18.5) | 0.360* | 13 (10-20) | 13.5 (10-20.25) | 0.490* |
| Morbidity, n (%) | 0.367** | 0.630** | |||||
| Yes | 27 (30.3) | 15 (34.9) | 12 (26.1) | 12 (27.9) | 15 (32.6) | ||
| No | 62 (69.7) | 28 (65.1) | 34 (73.9) | 31 (72.1) | 31 (67.4) | ||
| Clavien-Dindo classification, n (%) | 0.011** | 0.902** | |||||
| 0 | 45 (50.6) | 15 (34.9) | 30 (65.2) | 23 (53.5) | 22 (47.8) | ||
| 1 | 11 (12.4) | 8 (18.6) | 3 (6.5) | 4 (9.3) | 7 (15.2) | ||
| 2 | 7 (7.9) | 4 (9.3) | 3 (6.5) | 4 (9.3) | 3 (6.5) | ||
| 3 | 9 (10.1) | 3 (7.0) | 6 (13.0) | 4 (9.3) | 5 (10.9) | ||
| 5 | 17 (19.1) | 13 (30.2) | 4 (8.7) | 8 (18.6) | 9 (19.6) | ||
| Mortality, n (%) | 0.010** | 0.908** | |||||
| Yes | 17 (19.1) | 13 (30.2) | 4 (8.7) | 8 (18.6) | 9 (19.6) | ||
| No | 72 (80.9) | 30 (69.8) | 42 (91.3) | 35 (81.4) | 37 (80.4) |
Low SMA: SMA≤87 for female or SMA≤113 for male; High SMA: > 87 for female or SMA>113 for male.
*Mann-Whitney U test was used for P values.
**Pearson Chi-square test was used for P values.
PNI: prognostic nutritional index; SMA: skeletal muscle area.
Table 4 Factors associated with presence of mortality and morbidity
| Demographic characteristics of patients | Patients with morbidity (n = 27) | Patients without morbidity | p value | Patients with mortality (n = 17) | Patients without mortality | p value |
|---|---|---|---|---|---|---|
| Age; mean ± standard deviation | 66.93 ± 10.63 | 65.52 ± 11.55 | 0.589* | 68.94 ± 9.73 | 65.24 ± 11.52 | 0.224* |
| Sex | 0.771** | 0.705** | ||||
| Male | 17 (63%) | 37 (59.7%) | 11 (64.7%) | 43 (59.7%) | ||
| Female | 10 (37%) | 25 (40.3%) | 6 (35.3%) | 29 (40.3%) | ||
| ASA score | 0.527** | 0.098** | ||||
| ASA I | 0 | 0 | 0 | 0 | ||
| ASA II | 17 (63%) | 32 (51.6%) | 10 (58.8%) | 39 (54.2%) | ||
| ASA III | 10 (37%) | 29 (46.8%) | 6 (35.3%) | 33 (45.8%) | ||
| ASA IV | 0 | 1 (1.6%) | 1 (5.9%) | 0 | ||
| Pre-operative total peripheral lymphocyte count (per mm3); | 0.989*** | 0.113*** | ||||
| Median (Q1-Q3) | 1800 (1300-2400) | 1800 (1200-2400) | 1300 (1100-2200) | 1900 (1300-2400) | ||
| Pre-operative level of albumin (g/dl); | 0.543* | 0.011* | ||||
| Mean ± standard deviation | 3.34 ± 0.67 | 3.44 ± 0.72 | 3.02 ± 0.78 | 3.5 ± 0.65 | ||
| Comorbidities**** | ||||||
| Hypertension (HT) | 7 (25.9%) | 31 (50%) | 0.035 | 6 (35.3%) | 32 (44.4%) | 0.493 |
| Diabetes Mellitus (DM) | 5 (18.5%) | 25 (40.3%) | 0.045 | 3 (17.6%) | 27 (37.5%) | 0.119 |
| Coronary Artery Disease | 1 (3.7%) | 5 (8.1%) | 0.663 | 2 (11.8%) | 4 (5.6%) | 0.322 |
| Atrial fibrillation | 1 (3.7%) | 2 (3.2%) | 0.909 | 2 (11.8%) | 1 (1.4%) | 0.092 |
| Chronic obstructive pulmonary disease | 4 (14.8%) | 16 (25.8) | 0.253 | 7 (41.2%) | 13 (18.1%) | 0.040 |
*Independent sample T test was used for p values.
**Pearson Chi-square test was used for p values.
***Mann-Whitney U test was used for p values.
****Fisher's exact test was used for p values.
ASA: American Society of Anesthesiology.
Table 5 Univariate and multivariate analysis for the factors affecting morbidity and mortality
| Variables | Morbidity | Mortality | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analyses | p value | Multivariate analyses | p value | Univariate analyses | p value | Multivariate analyses | p value | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | |||||
| Age (year) | 1.011 (0.971-1.054) | 0.585 | 1.035 (0.980-1.093) | 0.219 | 1.032 (0.981-1.085) | 0.223 | 1.003 (0.943-1.067) | 0.930 |
| Male Gender | 1.149 (0.453-2.915) | 0.771 | 1.160 (0.381-3.532) | 0.793 | 1.236 (0.411-3.717) | 0.705 | 0.935 (0.263-3.323) | 0.917 |
| Hypertension | 0.350 (0.129-0.946) | 0.039 | 0.303 (0.095-0.973) | 0.045 | 0.682 (0.227-2.044) | 0.494 | 0.895 (0.242-3.310) | 0.868 |
| Diabetes mellitus | 0.336 (0.112-1.006) | 0.051 | 0.396 (0.122-1.287) | 0.124 | 0.357 (0.094-1.357) | 0.131 | 0.339 (0.077-1.485) | 0.151 |
| Chronic obstructive pulmonary disease | 0.500 (0.150-1.668) | 0.259 | 0.284 (0.074-1.092) | 0.067 | 3.177 (1.019-9.907) | 0.046 | 2.892 (0.821-10.185) | 0.098 |
| Low SMA | 0.800 (0.323-1.983) | 0.630 | 0.633 (0.224-1.785) | 0.387 | 0.940 (0.326-2.708) | 0.908 | 0.810 (0.246-2.668) | 0.729 |
| Low PNI | 1.518 (0.612-3.767) | 0.368 | 1.327 (0.438-4.023) | 0.617 | 4.550 (1.351-15.329) | 0.014 | 4.836 (1.233-18.967) | 0.024 |
Low SMA: SMA ≤ 87 for female or SMA ≤ 113 for male; High SMA: > 87 for female or SMA > 113 for male.
CI: confidence interval; PNI: prognostic nutritional index; SMA: skeletal muscle area.
Discussion
Our study showed that low PNI is an independent prognostic factor for post-operative mortality in patients underwent PD for PRT. On the other hand SMA was not effective on post-operative mortality and morbidity in these patients. PD is still a complicated surgery with 5% of mortality and 50% of morbidity rate. Factors affecting the post-operative mortality and morbidity are still maintain importance. Importance of nutritional status in these patients before the operation is well known. Cancer cachexia is a multifactorial syndrome characterized by a sustained loss of skeletal muscle mass and cannot be completely reversed with conventional nutritional support and cause progressive functional impairment10. Studies showed that complex tumor-host interactions, inflammatory cytokines, hormones, and neuropeptides cause the development of cancer cachexia in patients with pancreatic cancer11. In the literature, SMA value is used for many malignancies as a predictive value for mortality and morbidity12-14. Furthermore, it is measured in healthy populations in many studies5,15,16. In the study of Kim et al.5, the cutoff values for male and female were found as 119.3 cm2 and 74.2 cm2. On the other hand in the study of A. Van der Werf et al.16, they found the cutoff values in healthy Caucasian population as 134 cm2 and 89.2 cm2. In our study, we found the cutoff values in patients with PRT as 113 cm2 in male and 82 cm2 in female which were both lower than healthy population and the median that found in the study of Linder et al.17. That shows that patients with PRT are inclined sarcopenia than the healthy population. Whereas we could not find any association between the SMA value and increased morbidity and mortality rate. In many studies, SMA is used for predicting the sarcopenia and patients' survival in patients that followed in oncology departments14,15,17. Unfortunately, we could not compare the patients' follow-up SMA values due to having missing data. On the other hand, SMA values in our patients were lower than the healthy population and the patients that underwent PD in the literature. The mortality and morbidity rate in our study was 19% and 30%, respectively. We think that these mortality and morbidity rates in our study are due to being a less experienced hepatopancreatic biliary center with a low annual patient volume and patients with high ASA scores.
PNI was reported as a predictive value for nutritional risk in many studies8,9,18,19. In the study of Hoon Lee et al.9, they found the PNI as a predictive parameter for patients' survival with the 49.5 cutoff in all stages of pancreas cancer. Whereas in another study of Dogan et al., they found that PNI was not a predictive parameter for survival in patients with metastatic pancreatic cancer20. In our study, we found an association between Low PNI and Clavien Dindo complication score and mortality. Furthermore, we found PNI as a risk factor for post-operative mortality in multivariate analysis.
We also analyzed association between patients' age, sex, ASA score, and comorbidities with the mortality and morbidity. In addition, to the literature, hypertension and diabetes mellitus were significantly lower in patients with morbidity. Furthermore, serum level of albumin was significantly lower, and COPD was significantly higher in patients with mortality.
Limitations
The primary limitation of the study is to be a retrospective study. Second, we being a less experienced hepatopancreaticobiliary center with a low annual patient volume caused an incompatible morbidity and mortality rates according to the literature. Third, due to missing data of the patients, we could not analyze the skeletal muscle index which is more predictive parameter for these patients. That may have caused to find the SMA as non-effective parameter for morbidity and mortality.











 nueva página del texto (beta)
nueva página del texto (beta)