Introduction
Infra-popliteal (or below-the-knee [BTK]) atherosclerosis is the most common cause of critical limb ischemia (CLI). The pathology is associated with increased morbidity, mortality, and amputation rates1. The mortality rates of patients with peripheral arterial disease (PAD), especially in the presence of CLI, are approximately 20% in 6 months and may be more than 50% within 5 years from the first diagnosis2,3. Endovascular interventions are more frequently preferred in the current era with respect to the low success rates of open surgical revascularization in the infra-popliteal lesions1. However, despite advances in endovascular procedures, the restenosis and revascularization necessities are still challenging4,5.
Percutaneous transluminal angioplasty (PTA) alone is widely used for the treatment of infra-popliteal atherosclerosis. It may be performed with standard or drug-coated balloons. However, the long-term patency of the technique is suboptimal6. The calcification, which frequently persists in tibial arteries, limits the efficacy of PTA leading to vessel recoil, dissection, and increased target lesion revascularization (TLR)7,8.
At present, there is no approved stent available for the treatment of infra-popliteal revascularization. On the other hand, atherectomy provides atherosclerotic plaque removal from the arterial wall and may be used as a sole therapy or applied in combination with balloon angioplasty9.
The symptomatic PAD is seen in approximately 21% of the patients with diabetes mellitus10. The infra-popliteal lesions generally consist of heavy and circumferential calcifications. These characteristic features of the BTK lesions complicate revascularization and cause endovascular interventions to become more challenging11. Diabetes mellitus may lead to chronic kidney disease which in combination significantly increases incidence of PAD12. Percutanous transluminal angioplasty of complex and calcified lesions may result in the early recoiling and dissections in patients with diabetes mellitus and end-stage renal disease. Furthermore, the primary and secondary patency rates are lower in these cases and bailout stenting may be required in up to 50% of the cases13.
Patients with CLI generally have transatlantic inter-society consensus D lesions, total occlusions, and/or advanced calcified lesions, and these lesions are not fully suitable for interventional therapies. Surgical treatment is superior to PTA (with or without stenting) in the presence of a suitable ipsilateral saphenous vein and an appropriate non-calcified artery6. However, the patients with CLI, especially those with infra-popliteal lesions, sometimes do not have an appropriate saphenous vein as a graft or a non-calcified bypass-able patent artery. Besides, these patients may have multiple comorbidities, that the open surgical treatment may have higher risk for the occurrence of major adverse events6.
Preparation of the vessels before PTA in complex lesions increases the success rates of PTA. For instance, the increased lumen diameter before angioplasty could enable lesion crossing and provide higher long-term patency rates13. The atherectomy prepares vessels by debulking the plaque burden and requires lower pressures of PTA for revascularization; presenting decreased risk of intimal hyperplasia and dissection14.
The aim of the present study was to compare the long-term results of rotational atherectomy followed by drug-coated balloon angioplasty (AT+DCB) with sole drug-coated angioplasty (DCB) for the treatment of infra-popliteal PAD in patients with diabetes mellitus.
Patients and methods
This retrospective study included 128 diabetic patients with symptomatic PAD patients secondary to infra-popliteal lesions who underwent endovascular interventions with drug-coated balloon alone or in combination with atherectomy between April 2015 and January 2020. Due to the retrospective nature of the study, the ethical approval was not required. The patients older than 18 years of age, who had severe claudication (Rutherford 3) or CLI (Rutherford 4-6) were investigated retrospectively if they had at least 70% stenosis in a lower extremity, confirmed by angiography. Patients with concomitant femoropopliteal disease and in-stent restenosis were excluded from the study. The 128 patients and a total of 218 BTK interventions were categorized into two groups according to use of rotational atherectomy followed by drug-coated balloon (AT+DCB) or drug-coated balloon (DCB) alone.
All of the patients had diabetes mellitus with the mean HbA1c levels of 8.9. Mean age of the patients were 66.4 ± 10.7 years and 67.1% (n = 86) of the patients were male. About 76.5% (n = 98) of patients consisted of past and current smokers. Hypertension and hyperlipidemia were the most frequently seen comorbidities in our cohort, found in 75.8% (n = 97) and 73.4% (n = 94), respectively; followed by 71.1% (n = 91) of the patients with coronary artery disease. About 29.2% (n = 19) of patients had a history of myocardial infarction, while 32% (n = 41) of the patient population had coronary artery revascularization either percutaneously or with coronary artery bypass surgery. About 11.7% (n = 15) of the patients had prior amputations.
Percutaneous interventions were performed with standard techniques as femoral ante- and retrograde approach. Dual antiplatelet therapy including 300 mg aspirin and 300 mg or 600 mg clopidogrel were initiated in all patients before the procedures. Heparin (100 units/kg) was administered for periprocedural anticoagulation. Drug-coated balloon was applied with (BioPath 035 paclitaxel-eluting balloon dilatation catheter) balloon diameters of 80-90% of reference vessel with low pressure and 60 s inflation time. Additional inflations were not hesitated if necessary. Phoenix rotational atherectomy device (Volcano Corporation, San Diego, California) was utilized in this study. Distal protection systems were not used. The interventions with a result of postprocedural TIMI 3 flow, without dissection, and residual stenosis were defined as successful intervention.
The primary endpoints of this study were determined as primary patency rates, clinically driven repeat endovascular and surgical limb revascularization (CD-TLR). The change in ankle brachial index (ABI) and Rutherford classification at 1 and 2 years were also evaluated. The secondary endpoints included 1-year all-cause mortality, major and minor amputations, and peri-procedural complications such as perforation, dissection, and distal embolization.
All the patients were prescribed 40 mg/day atorvastatin and dual antiplatelet therapy with clopidogrel (75 mg) and acetylsalicylic acid (100 mg) once a day. Dual antiplatelet therapy was used to prevent the risk of acute or subacute thrombosis originating from the intima-media exposure of reticulocytes after atherectomy15.
Statistical analysis
All the statistical analysis was performed with SPSS 18.0 software (Statistical Package for the Social Sciences Inc., Chicago, Ill, US). Data are expressed as mean ± SD for continuous variables and as counts for categorical variables. Categorical variables are presented as percentages. Comparisons of clinical, angiographic, and procedural characteristics were performed with the Fisher exact test for categorical variables and Mann–Whitney U-test for non-parametric continuous variables. Odds ratio and 95% confidence interval were calculated with univariate logistic regression. Variables with p ≤ 0.2 in the univariate model or known to be significantly associated were entered into a multivariate logistic regression model. The target vessel revascularization, primary, and secondary patency rates during the follow-up were presented with Kaplan–Meier event-free survival curves. A value of p < 0.05 was described statistically significant.
Results
The features of patients and characteristics of the lesions are described in Table 1. A total of 228 BTK procedures were performed in 128 patients. The AT+DCB group consisted 50.7% (n = 65) of the interventions and 49.3% (n = 63) of the patients were treated only with DCB. Clinical characteristics of the patients were similar in both groups. An indication for the treatment of CLI was present in 74.2% (n = 95) of the patients.
Table 1 Baseline characteristics and risk factors
| Variables | Total (n = 128) | RA-DCB (n = 65) | DCB (n = 63) | p-value |
|---|---|---|---|---|
| Mean age, years | 66.4 ± 10.7 | 68.6 ± 12.4 | 63.2 ± 11.3 | 0.528 |
| Male, gender | 67.1% (86/128) | 67.6% (44/65) | 67.8% (42/63) | 0.423 |
| Diabetes Mellitus | 100% (128/128) | 100% (65/65) | 100% (63/63) | 1.000 |
| HbA1c (SD) | 8.9 (1.6) | 9.2 (1.3) | 8.7 (1.8) | 0.758 |
| Hypertension | 75.8% (97/128) | 87.5% (48/65) | 77.8% (49/63) | 0.856 |
| Hyperlipidemia | 73.4% (94/128) | 73.5% (49/65) | 71.4% (45/63) | 0.793 |
| Smoking | ||||
| Current smoker | 46.1% (59/128) | 46.1% (30/65) | 46.0% (29/63) | 0.563 |
| Past smoker | 30.4% (39/128) | 32.3% (21/65) | 25.6% (18/63) | 0.647 |
| Never smoker | 21.7% (30/128) | 27.7% (18/65) | 19.0% (12/63) | 0.452 |
| BMI (kg/m2) | 32.3 ± 6.7 | 32.7 ± 6.8 | 31.7 ± 6.4 | 0.482 |
| CAD | 71.1% (91/128) | 78.5% (51/65) | 63.4% (40/63) | 0.453 |
| History of stroke | 10.1% (13/128) | 12.3% (8/65) | 7.9% (5/63) | 0.352 |
| History of MI | 29.2% (19/128) | 18.4% (12/65) | 11.1% (9/63) | 0.567 |
| CHF | 14.1% (18/128) | 16.9% (11/65) | 11.1% (7/63) | 0.752 |
| CABG or PCI | 32.0% (41/128) | 33.8% (22/65) | 30.1% (19/63) | 0.468 |
| CRD | 20.3% (26/128) | 21.5% (14/65) | 19% (12/63) | 0.355 |
| ESRD | 21% (21/128) | 20% (13/65) | 12.6% (8/63) | 0.582 |
| COPD | 28.2% (36/128) | 32.3% (21/65) | 23.8% (15/39) | 0.498 |
| Aspirin | 94.45% (121/128) | 95.3% (62/65) | 93.6% (59/63) | 0.454 |
| Clopidogrel | 96.1% (123/128) | 96.9% (63/65) | 95.2% (60/63) | 0.328 |
| Statin | 85.9% (110/128) | 83.1% (54/65) | 88.8% (56/63) | 0.256 |
| Prior amputation | 11.7% (15/128) | 13.8% (9/65) | 9.5% (6/63) | 0.228 |
The characteristics of the lesions such as the location and the morphology of the segments and the number of total chronic occlusions were similar in both groups. The pre-operative ABI and Rutherford classification data did not significantly differ between the two groups (p = 0.28). The mean lengths of the lesions were also similar (47.12 ± 24.03 mm in AT+DCB vs. 42.26 ± 26.5 mm in DCB, p = 0.47). Vessel calcifications (75.4% in AT+DCB vs. 69.1% in DCB) were comparable between two groups.
The location of the lesion was primarily the anterior tibial artery both in AT+DCB and DCB alone group (43.2%, n = 51 vs. 42.7%, n = 47). The mean time of inflation duration, length, and diameter of balloon angioplasty among two intervention groups were similar ([2.8±1.3 min vs. 3.1±1.5 min [p = 0.63], 3.2±0.9 mm vs. 3.4±1.1 mm [p = 0.33], and 12.3±8.2 cm vs. 11.9±6.7 cm (p = 0.47]). However, inflation pressures required for sufficient arterial patency were higher in DCB alone group (6.2±3.9 vs. 8.9±4.1 atmospheres [p = 0.001]).
Technical success rates were similar in the AT+DCB group (Fig. 1) and DCB alone group (98.4% vs. 96.8%, p = 0.228). The adverse events did not differ between two groups; however, bailout stenting was more common in the PTA alone group (DCB, 11.1% [n = 7] vs. AT+DCB, 1.5% [n = 1], p < 0.001) as a result of flow-limiting dissection. The periprocedural complications are presented in Table 2.
Table 2 Peri-procedural complications
| Complication | RA + DCB | DCB only | p-value |
|---|---|---|---|
| Distal embolism (clinically significant) | 1.5% (1/65) | 9.5% (6/63) | 0.05 |
| Dissection-grade C/D or greater | 1.5% (1/65) | 11.1% (7/63) | < 0.001 |
| Vessel recoil | 1.5% (1/65) | 4.7% (3/63) | < 0.001 |
| Arterial perforation | 1.5% (1/65) | 3.1% (2/63) | 0.638 |
| Arteriovenous fistula | 0 | 1.6% (1/63) | 0.623 |
| Pseudoaneursysm | 0 | 0 | 1.000 |
| Hematoma | 3% (2/65) | 3.1% (2/63) | 0.476 |
| Total number of events | 5 | 18 | < 0.001 |
TLR at 6 months was not different in both groups (DCB, 6.3% [n = 4] vs. AT+DCB, 3.1% [n = 2], p = 0.224). However, it was more frequent in the DCB only group at 12 months follow-up (DCB, 17.4% [n = 11] vs. AT+DCB, 6.1% [n = 4], p = 0.001) and 24 months follow-up (DCB, 30.1% [n = 7] vs. AT+DCB, 10.7% [n = 7], p < 0.001) (Fig. 2). CD-TLR rate was detected significantly lower at 1 and 2 years with the use of AT+DCB when compared with DCB (6.1% vs. 17.4%; p < 0.001) in Kaplan-Meier analysis. The rate of CD-TLR decreased by 64% at 1 year and 65% in 2 years with AT+DCB when compared with DCB only group in the adjusted Cox proportional hazard model (HR 0.23, 95% CI 0.32-0.78; p < 0.01; HR 0.23, 95% CI 0.27-0.76; p < 0.01). The values are presented in Figure 2.
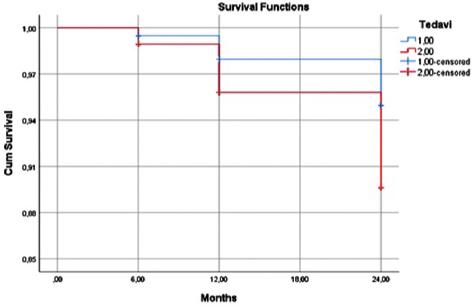
The minor amputation rates at 6-12- and 24-months follow-ups were lower in AT+DCB compared to DCB only group (3.1%, n = 2 vs. 9.5%, n = 6, p = 0.08; 6.1%, n = 4 vs. 12.6%, n = 8, p = 0.07; 7.6%, n = 5 vs. 15.8%, n = 10, p = 0.58), while the major amputation rates were similar between groups. At 6 months follow-up, there were two patients (3.1%) with below the knee + Syme amputations in DCB group and one patient (1.5%) with Syme amputation in RA+DCB (p = 0.57). At 12-month follow-up, three patients (4.7%) treated with DCB alone had above the knee amputation and two of the patients (3.1%) in AT+DCB group had Syme amputations (p = 0.64). At 24-month follow-up, four patients (6.3%) in DCB only group and two patients (3.1%) in AT+DCB group required below the knee amputations (p = 0.58) (Fig. 2). The all-cause mortality rates at 6, 12, and 24 months were also similar (Fig. 3). At 6-month follow-up, two patients (3.1%) in DCB alone group and one patient in (1.5%) AT+DCB group; at 12 months follow-up, three patients (4.7%) in DCB alone group and two patients (3.1%) in AT+DCB group; and at 24 months follow-up, four patients (6.3%) in DCB alone and two patients (3.1%) in AT+DCB group were deceased (p = 0.25; p = 0.23; p = 0.44). Finally, distal embolization rates were significantly lower in the AT+DCB group when compared with DCB only group (1.5%, n = 1 vs. 9.5%; n = 6, p = 0.05). The amputation free survival and all-cause mortality are presented in Figures 3 and 4.
Discussion
Patients with diabetes mellitus often experience atherosclerotic peripheral arterial lesions in the course of the disease. Advanced infra-popliteal atherosclerosis is associated with severe lower extremity ischemia16. The comorbidities such as older age, diabetes mellitus, and end-stage renal disease are associated with high risk of complex and highly calcified lesions which increase the risk of amputation and mortality. Even at a rate as high as 67% amputation is performed as an initial therapy without diagnostic angiography or further vascular interventions in this particular patient population with CLI17.
Atherectomy has been shown to be a useful adjunctive therapy in the long term, especially in the long and calcified lesions. While directional atherectomy devices are generally used in short or chronic totally occluded lesions, rotational atherectomy devices are more effective in long, highly calcified lesions. The improved luminal gain and decreased requirement for stenting are the main advantages of atherectomy when compared with PTA. These advantages allow inflation of the balloon at lower pressures providing lower dissection rates18-20.
Atherectomy provides a reduction in plaque burden and facilitates PTA. Such an advantage has proven superior to PTA alone treatment in patients with CLI due to complex infra-popliteal diseases21. The patency rates and patient outcomes have been improved parallelly with increased clinical experience for the use of atherectomy as an alternative or additive technique for the treatment of PAD22.
According to the randomized trial in 2005, amputation-free survival at 6 months was similar between the infra-inguinal saphenous vein bypass and PTA at the above-knee or below-knee segments (BASIL). Since then, endovascular interventions decreased morbidity, lowered the costs, and provided sufficient quality of life outcomes for the patients equal to the surgery23.
The DEBATE-BTK trial included 132 diabetic patients with CLI. The study compared drug-eluting balloon (In.Pact Amphirion, Medtronic Cardiovascular) and PTA in 158 infra-popliteal lesions. The mean length of lesion was 129 ± 83 mm and this was longer than other randomized trials with drug-eluting stents for the treatment of the infra-popliteal lesions. The restenosis rate and target vessel occlusion were higher in PTA group at 1 year, and major adverse events were less often in the drug-eluting balloon group. However, amputation, limb salvage, and mortality rates were similar between the two groups24.
In another study, the results of atherectomy were compared on patients with diabetes mellitus and non-diabetic patients with PAD. The TLR, amputation, or death rates were not significantly different between the groups. In addition, there was no statistically significant difference in the time to TLR, amputation or death in Kaplan–Mayer analysis in this particular research25.
Stavroulakis et al.25 compared drug-coated balloon angioplasty with directional atherectomy with anti-restenotic therapy in popliteal artery lesions. The freedom from TLR was similar between two groups (82% vs. 94%, p = 0.072), while the primary patency rates were found significantly higher in the DAART group (p = 0.021) at 12-month follow-up. Secondary patency rates were similar (96% vs. 96%) between two groups at 12 months. Bailout stenting was more often following DCB angioplasty (p = 0.13) and aneurysmal degeneration was more common after DAART (p = 0.25)26.
In another recent meta-analysis, there was no significant benefit associated with single use of atherectomy compared to balloon angioplasty27. Atherectomy was typically used for highly calcified lesions that were challenging for stent or balloon expansion, or in the regions that are risky for stent fracture (common femoral and popliteal arteries). Despite more often occurrence of distal embolization in the registry data, it was found lower in the contemporary non-randomized DEFINITIVE-LE study28. Literature lacks information about the use of distal protection for atherectomy; however, it is generally applied in the existence of poor or single-vessel distal run-off29.
Severity of illness, amputation level, gender, and comorbidities may influence the amputation rates. The amputation rates were higher in male and diabetic patients in the reported analysis and the procedure types (DCB or PTA alone vs. atherectomy-PTA or atherectomy-DCB) were not found superior to one another in terms of amputation rates in the multivariate analysis30. Among the included studies, all-cause mortality rates did not differ between both groups at 12 and 24 months. The patients with more advanced diseases had higher mortality rates22,31.
In our study, although the major amputation rates were similar between two groups, minor amputation rates were lower in the AT+DCB group. CD-TLR rate was significantly lower in AT+DCB group and the rate of CD-TLR was decreased by 64% at 1-year and 65% at 2-year with AT+DCB when compared with DCB alone, in the adjusted Cox proportional hazard model. The all-cause mortality rates and adverse events did not differ significantly between two groups; however, bailout stenting and distal embolization rates were lower in AT+DCB group.











 nueva página del texto (beta)
nueva página del texto (beta)